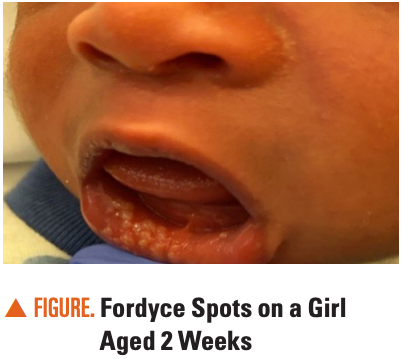
2-week-old girl with lesions on her lips, cheeks, and nasolabial folds
Can you diagnose this healthy, 8.2-lb girl with lesions primarily on her lower lip but also her upper lip, cheeks, and nasolabial folds?
The Case
A healthy, 8.2-lb girl aged 2 weeks presented with lesions primarily on her lower lip but also her upper lip, cheeks, and nasolabial folds (Figure). The lesions on her lower lip were 3- to 4-mm, shiny, white-yellowish papules, whereas those on the rest of her face were smaller (<1 mm). The girl was otherwise asymptomatic with no signs of bleeding, pain, or infection. According to her parents, she was feeding well and growing appropriately for her age.
What is the diagnosis?
Fordyce spots
Epidemiology and etiology
Fordyce spots represent benign, painless, visible, and ectopically located sebaceous glands not associated with hair follicles.1 They are uncommon in the first weeks of life. Although Fordyce spots may be present in up to 80% of adults,2 estimates suggest a prevalence of less than 5% in neonates.3,4 However, some studies show a much higher prevalence, such as 44% of 1000 Iranian neonates examined in a prospective cohort study.5
The mucosa of the lips, cheeks, and, less commonly, gums have been implicated in these ectopic sebaceous glands.6 Fordyce spots are likely a normal anatomic variant. Although their etiology is not entirely elucidated, they are caused by biological and environmental factors, including maternal hormonal changes such as androgen stimulation.1,7
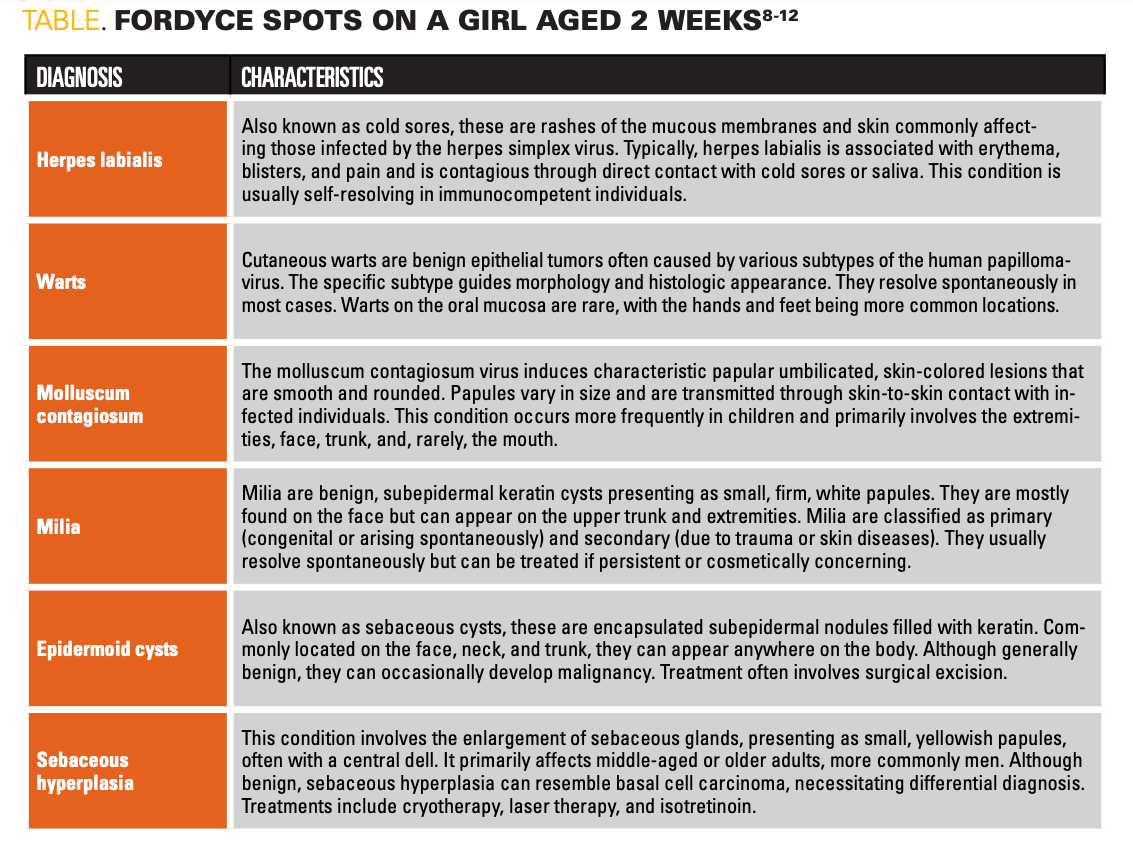
Differential diagnoses
In addition to Fordyce spots, differential diagnoses include oral herpes, warts, molluscum, milia, epidermoid cysts, and sebaceous hyperplasia (Table).8-12
Click image to zoom in
Evaluation and workup
Fordyce spots are primarily diagnosed clinically based on their characteristic appearance and distribution. In the presented case of a girl aged 2 weeks with lesions on the lips, cheeks, and nasolabial folds, the key features to note are the shiny, white-yellowish papules on the lower lip, typical of Fordyce spots. These lesions are benign ectopic sebaceous glands that do not require further invasive diagnostic testing. However, a thorough medical history and physical examination are crucial to rule out other conditions in the differential diagnosis, such as oral herpes, milia, epidermoid cysts, and sebaceous hyperplasia.3,5
No specific laboratory or imaging studies are necessary for diagnosing Fordyce spots, as their identification is based on clinical presentation. A biopsy can be performed in cases where the diagnosis is unclear or if there are atypical features. Histological examination would reveal clusters of mature sebaceous glands without an associated hair follicle, confirming the diagnosis of Fordyce spots.2
Clinical course
Fordyce spots typically have a benign and self-limiting course, especially in neonates and infants. The lesions are often asymptomatic and do not require treatment, as they generally do not cause discomfort or complications. In most cases, the lesions may persist without significant changes or slowly regress. The cosmetic concern might be the primary issue for parents or caregivers, as these spots can be noticeable on the mucosal surfaces.3
In neonates, Fordyce spots are considered a normal variant and are expected to decrease in prominence as the child grows. The clinical course is usually uneventful, with no associated systemic symptoms or complications. The natural history of Fordyce spots is to remain static or to resolve spontaneously, usually by adolescence or early adulthood.3
Management and follow-up
Management of Fordyce spots is typically conservative, focusing on reassurance and education for the parents. Because the condition is benign and asymptomatic, no active treatment is necessary. The parents should be informed that Fordyce spots are a common and normal finding in neonates and do not indicate any underlying health issues.2,3
Follow-up is not usually required unless the lesions change in appearance, become symptomatic, or there is concern about a secondary infection or other underlying condition. In such cases, a follow-up examination may be warranted to reassess the condition and rule out other potential diagnoses.3,5
In summary, Fordyce spots in neonates are benign and self-limiting, requiring no intervention. Reassurance and education about the nature of these lesions are the mainstays of management, with follow-up only if necessary.
References
1. Farci F, Rapini RP. Sebaceous hyperplasia. In: StatPearls [Internet]. StatPearls Publishing; 2024. Accessed July 1, 2024. https://www.ncbi.nlm.nih.gov/books/NBK562148/
2. Requena L, Sangüeza O. Ectopic sebaceous glands: Fordyce’s spots, Tyson’s glands, and Montgomery’s tubercles. In: Cutaneous Adnexal Neoplasms. Springer, Cham; 2017. Accessed July 1, 2024. https://doi.org/10.1007/978-3-319-45704-8_62
3. Shubhankar M, Pravakar M, Ranjan BD, Agarwalla SK, Sambedana P, Swayamsiddha M. Prevalence and presentation of cutaneous lesions in healthy neonates: a single-center study from Eastern India. Indian J Child Health. 2017;4(4):566-570. doi:10.32677/IJCH.2017.v04.i04.024
4. Flinck A, Paludan A, Matsson L, Holm AK, Axelsson I. Oral findings in a group of newborn Swedish children. Int J Paediatr Dent. 1994;4(2):67-73. doi:10.1111/j.1365-263x.1994.tb00107.x
5. Moosavi Z, Hosseini T. One-year survey of cutaneous lesions in 1000 consecutive Iranian newborns. Pediatr Dermatol. 2006;23(1):61-63. doi:10.1111/j.1525-1470.2006.00172.x
6. James WD, Elston DM, McMahon PJ. Andrews’ Diseases of the Skin: Clinical Atlas. Elsevier; 2018.
7. Paller AS, Mancini AJ. Hurwitz Clinical Pediatric Dermatology: A Textbook Of Skin Disorders of Childhood and Adolescence. 6th ed. Elsevier; 2021.
8. Opstelten W, Neven AK, Eekhof J. Treatment and prevention of herpes labialis. Can Fam Physician. 2008;54(12):1683-1687.
9. Jablonska S, Orth G, Obalek S, Croissant O. Cutaneous warts: clinical, histologic, and virologic correlations. Clin Dermatol. 1985;3(4):71-82. doi:10.1016/0738-081x(85)90051-3
10. Hanson D, Diven DG. Molluscum contagiosum. Dermatol Online J. 2003;9(2):2.
11. Gallardo Avila PP, Mendez MD. Milia. In: StatPearls [Internet]. StatPearls Publishing; 2024. Accessed July 1, 2024. https://www.ncbi.nlm.nih.gov/books/NBK538168/
12. Zito PM, Scharf R. Epidermoid cyst. In: StatPearls [Internet]. StatPearls Publishing; 2024. Accessed July 1, 2024. https://www.ncbi.nlm.nih.gov/books/NBK499974/
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.
