"He keeps getting stomachaches, Doctor. What's wrong?"
Children who complain of frequent bellyaches present a vexing clinical challenge. These guidelines will help you rule out organic disease and manage an ongoing biopsychosocial disorder.
"He keeps getting stomachaches, Doctor. What's wrong?"
By Michelle S. Dern, MD, and Martin T. Stein, MD
Children who complain of frequent bellyaches present avexing clinical challenge. These guidelines will help you rule out organicdisease and manage an ongoing biopsychosocial disorder.
When a child with recurrent abdominal pain (RAP) appears on a scheduletightly booked with health supervision visits and acute illnesses, evenseasoned practitioners are dismayed. We have developed an office-based approachto the evaluation and management of a child with RAP that can guide youthrough this challenging process. Our approach is based on an integratedphysiologic and psychosocial model. The discussion will focus on school-agechildren and the developmental tasks that provide the context of symptoms.Episodic abdominal pain in adolescents has been reviewed elsewhere in theliterature.1
A trio of criteria
John Apley, a British pediatrician, defined RAP 40 years ago in The ChildWith Abdominal Pains.2Apley's criteria for RAP come in threes:children over 3 years of age, who complain of at least three episodes ofpain, that persist for at least three months and interfere with normal activity.For practical purposes, this definition has been expanded by many pediatriciansto include children whose pain--even if it is of shorter duration--is associatedwith some functional disability such as missed school. RAP affects 10% to15% of school-age children, many of whom miss substantial amounts of schooland cause their parents to miss work.
Apley's monograph described the typical patient as a school-age childwho has recurrent episodes of vague periumbilical belly pain. The childoften refuses to go to school or is sent home from school because of persistingpain. Physical examination is usually normal, with mild, nonlocalizing tendernessin some instances. Apley's original description proposed a simple, either/oretiology: RAP was either organic or emotional in origin. Our extended modelincludes three categories of possible explanations:3
- Identifiable organic causes for which specific diagnostic tests are available, such as inflammatory bowel disease or peptic ulcer disease
- Syndromes with specific patterns of symptoms but without specific diagnostic tests, such as irritable bowel syndrome and dyspepsia
- Functional abdominal pain in the absence of organic disease or other specific pattern.
For a case description of a typical child with RAP, see the box, "Jamesand the giant bellyache".

Allowing time for the evaluation
You can expect that the evaluation of a child with RAP will take moretime than most acute visits. The initial visit, especially for a new patient,should be scheduled for 20 to 30 minutes. Even with that much time, thefirst visit may not yield all the information you need. If an extended timeslot is not possible, a second visit will be necessary to complete the evaluation.In addition, most children with RAP require one or more follow-up visitsto monitor for changes in symptoms and provide support for the patient andfamily.
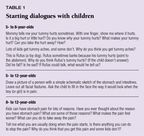
History. The first step in the evaluation is a detailed history fromthe parent and child. We suggest that you address your attention to thechild first. Specific questions that are consistent with the child's developmentallevel often reveal important information. Sample questions are listed inTable 1.
The history should focus simultaneously on physical, developmental, behavioral,and social issues. The clinician must explore both the physical diseaseprocess and the child's perceptions and feelings about the illness. Thisapproach is the foundation for a biopsychosocial perspective.
Most physical disorders are revealed in the history. Information aboutduration, frequency, timing, quality, and location of the pain may provideclues to the etiology. Find out what triggers, if any, exacerbate the pain.A specific food intolerance or anticipated anxiety at specific moments mayreveal a cause. Ask about treatments that have helped to relieve the pain.The presence or absence of associated symptoms such as fever, vomiting,diarrhea, weight loss, rash, arthritis, headache, dysuria, or bloody stoolsmay lead to specific diagnoses. Table 2lists the red flags that suggestan organic cause of the pain.

The medical history should be reviewed for surgical or nonsurgical abdominalproblems that were experienced as pain: intussusception, appendicitis, bowelobstruction, or constipation, for example. A prescription drug or an over-the-countermedication used for the abdominal pain or for other reasons may contributeto the pain. Possibilities include aspirin, ibuprofen, or other nonsteroidalanti-inflammatory medication. An assessment of the diet, with emphasis onany foods that lead to increased pain, may suggest carbohydrate intolerance.Constipation as a cause of RAP may be a sign of too little dietary fiberor an intolerance to cow's milk.4
Physical examination. Perform a complete abdominal examination, withparticular attention to abdominal distention, focal tenderness, hepatosplenomgaly,or an abdominal mass. Do a rectal examination to assess for stool impaction,occult blood, a mass, or perianal fistulae. Document vital signs and growthparameters. In most cases, the physical findings are normal.
Laboratory tests. A limited number of screening laboratory studies willrule out many organic diseases. The screening panel should include a completeblood count, erythrocyte sedimentation rate, urinalysis, and stool examinationfor ova and parasites. Giardia is the major parasite in the United Statesthat causes RAP, and it occasionally presents without diarrhea. A stoolGiardia antigen test may substitute for a microscopic examination and hasgreater sensitivity. Additional studies should be guided by specific historicalclues or findings in physical examination. Relevant laboratory tests arelisted in Table 3, which includes the more common causes of abdominal pain.

Family dynamics. The impact of the pain on the child's ability to functionat home and school and the family's adaptation to the recurrent symptomshould be assessed. Asking the child to draw a picture of the family canprovide a starting point for discussing family dynamics and the reactionsof family members to the child's problem. The drawings (shown in the figure)illustrate this approach.5 It is common for family members ofchildren with RAP to have gastrointestinal diseases or stress-related disorders.A family medical history should specifically inquire about inflammatorybowel disease, irritable bowel syndrome, and peptic ulcer disease. Abdominalsurgery, recurrent headaches, or anxiety disorders in family members maybe important clues to the origin of the child's problem.

Psychologic factors. RAP is classified by some observers as a somatoformdisorder with onset in childhood. Lipowski has defined a somatoform disorderas "the tendency to experience and communicate somatic distress andsymptoms unaccounted for by pathological findings, to attribute them tophysical illness, and to seek medical help for them."6 School-agechildren report a variety of complaints that may be symptoms of somatizationdisorder, including headache, fatigue, and sore muscles as well as abdominalpain. Studies report greater anxiety and depression in children who makethese complaints and in their mothers than among healthy controls.7Parents of children with RAP have more somatization symptoms, especiallypain syndromes, than parents whose children do not have RAP. For some children,RAP has its roots in a family model of illness behavior or a family climatein which somaticand emotional distress is freely expressed.
Sorting through the differential
The differential diagnosis of RAP in children involves multiple organsystems, as well as malignancies and infectious diseases. These diagnosesshould be considered for each patient so that treatable disorders will berecognized quickly and managed appropriately. However, the diagnostic taskshould not be daunting. The comprehensive medical, developmental, and psychosocialhistory, physical examination, and screening laboratory tests describedhere are usually sufficient. Red flags in the history or abnormalities onthe physical examination or screening laboratory studies warrant furthertesting: upper gastrointestinal radiographic study, abdominal ultrasound,contrast enema, or referral for endoscopy, for example.
Irritable bowel syndrome and dyspepsia syndrome should be considered.The symptoms of irritable bowel syndrome are abdominal pain relieved bydefecation, a variable stool pattern including diarrhea and constipation,and a sense of incomplete evacuation and abdominal distention. Dyspepsiasyndromes present with upper abdominal pain and tenderness. The cause isusually gastroesophageal reflux or Helicobacter pylori infection. Some patientswith dyspepsia may also have dysmotility symptoms with nausea, early satiety,and bloating.8H pylori infection has not been associated withRAP in the absence of dyspepsia signs.9
The differential diagnosis need not make a clear distinction betweenorganic and psychologic etiology. Indeed, as many clinicians know, the dichotomybetween organic disorders and psychological stressors is often inadequateor oversimplified as an explanation for RAP. Recent discoveries by neuroscientistssupport this clinical observation.
A useful model for understanding recurrent pain suggests that some patientswith RAP may have visceral hypersensitivity or hyperalgesia. Studies haveshown that adults with irritable bowel syndrome are more aware of balloondistention throughout the intestinal tract than other patients, and someof them are also more aware of normal intestinal motor activity.3Visceral hypersensitivity may be due to lower threshold of gut wall receptorsor altered modulation of sensory input. Patients with dyspepsia symptomsmay have greater mucosal sensitivity to acid pH or decreased threshold fordiscomfort produced by gastric distention. The child who told us, "Iguess some kids just get these pains," may have an accurate interpretationof visceral hyperalgesia.
Addressing causes and triggers
Treatments for children with RAP should address all components of thebiopsychosocial model. When specific organic diseases are identified, treatmentcan focus on the cause of the pain, the goal being a return to full functioning.When a symptom complex such as irritable bowel syndrome has been identified,dietary intervention with increased fiber may be helpful. Patients withdyspepsia often benefit from antacids or H2 blocker treatment,as well as dietary modification to eliminate food triggers suggested bythe history. When H pylori infection is found, treatment should includecombination medications. Many treatment protocols are available that addressH pylori specifically.
The treatment of the many children without an identifiable organic diseaseor syndrome poses a real challenge for the patient, parents, and pediatrician.Children with functional RAP often find relief when they recognize an environmentalor dietary trigger that initiates or exacerbates the pain. Many childrenappear to benefit significantly from a child-centered evaluation that engagesthe child in the interview and provides a running commentary on the findingsof the physical examination. For example, you might say to a 5-year-old,"Your belly feels nice and soft." An older child might be told,"Your liver and spleen are the right size; everything in your bellyfeels normal." In addition, pediatricians can teach coping skills tohelp prevent or reduce the pain. Specific approaches may include the following:
- Education for the child and parent about the nature of RAP, with reassurance that organic diseases have been excluded. It may be therapeutic to tell the child, "The pain is real but it does not mean that something is wrong with you."
- Dietary changes such as increased fiber, avoidance of potentially irritating fatty foods and caffeine, and an elimination trial of cow's milk.
- A daily diary to help identify the relationship of pain to stressors. This simple procedure may give some children a sense of control over the pain.
- Relaxation techniques such as progressive muscle relaxation or guided imagery.
- Monitoring and follow-up.
- Recognition that some children with depression, anxiety, or significant family disharmony may benefit from a referral to a mental health professional.
Treatment should be directed not only to the amelioration of pain, butalso the maintenance of self-esteem and the prevention of school absencesand pain-related changes in the normal pattern of social activities. Focusingentirely on pain management can be a trap, because the secondary gain somechildren derive from treatment and attention reinforces the need to missschool and other important social events. Instead, use the treatment processas an opportunity to teach coping skills that can have lifelong benefitsin a variety of situations.
Looking ahead
The prognosis for most children with RAP is uncertain. Several follow-upstudies report that the symptoms of RAP often persist beyond childhood.In some cases, an organic disease is eventually discovered, but this occursonly rarely.3 When Apley reviewed the outcome in adults who hadbeen diagnosed with RAP in childhoodas part of his original sample, a thirdhad continued abdominal pain and an additional third no longer had abdominalpain but had developed other symptoms such as headache. He concluded that"Little bellyachers are likely to grow up to be big bellyachers."A recent longitudinal study of 31 children with RAP reported that only onehad an organic diagnosis five years after initial evaluation. The otherscontinued to have somatic symptoms such as headaches significantly moreoften than controls, had greater functional disability, and used health-careservices more frequently.10
The lessons RAP teaches
The child with recurrent belly pains will always present a challengeto the primary care pediatrician. The symptoms are erratic and seem to suggesta long list of possible diagnoses. However, following the approach outlinedhere will lead the pediatrician to a confident diagnosis of RAP in mostcases. This confidence then allows the clinician, parents, and child tofocus on the management of chronic symptoms and return to full functioning.
DR. DERN is Assistant Clinical Professor of Pediatrics, University ofCalifornia at San Diego, La Jolla, CA.
DR. STEIN is Professor of Pediatrics, University of California at SanDiego.
REFERENCES
1. Silverberg M: Chronic abdominal pain in adolescents. Ped Annals 1991;4:179
2. Apley J: The Child With Abdominal Pains, ed 2. Oxford, England, Blackwell,1975
3. Hyams JS, Hyman PE: Recurrent abdominal pain and the biopsychosocialmodel of medical practice. J Pediatr 998;133:473
4. Giuseppe I, Cavataio F, Montalto G, et al: Intolerance of cow's milkand chronic constipation in children. N Engl J Med 1998;339:1100
5. Dixon SD, Stein MT: Encounters With Children: Pediatric Behavior andDevelopment, ed 2. St. Louis, Mosby, 1992
6. Lipowski ZJ: Somatization: The concept and its clinical application.Am J Psychiatry 1998:145:1358
7. Zeltzer LK, Barr RG, McGrath PA, et al: Pediatric pain: Interactingbehavioral and physical factors. Pediatrics 1992;90:816
8. Pineiro-Carrero VM, Andres JK, Davis RK, et al: Abnormal gastroduodenalmotility in children and adolescents with recurrent functional abdominalpain. J Peds 1988;113:820
9. Boyle JT: Recurrent abdominal pain: An update. Ped in Review 1997;18:310
10. Walker LS, Garber J, Van Slyke DA, et al: Long-term outcomes in patientswith RAP. J Pediatr Psychol 1995; 14:231