High-tech stethoscopes
Computer-assisted auscultation (CAA) devices use revolutionary technology developed to acquire, record, and analyze the acoustic signals of the heart. Pediatricians can use CAA software to identify specific heart sounds, including suspected murmurs.
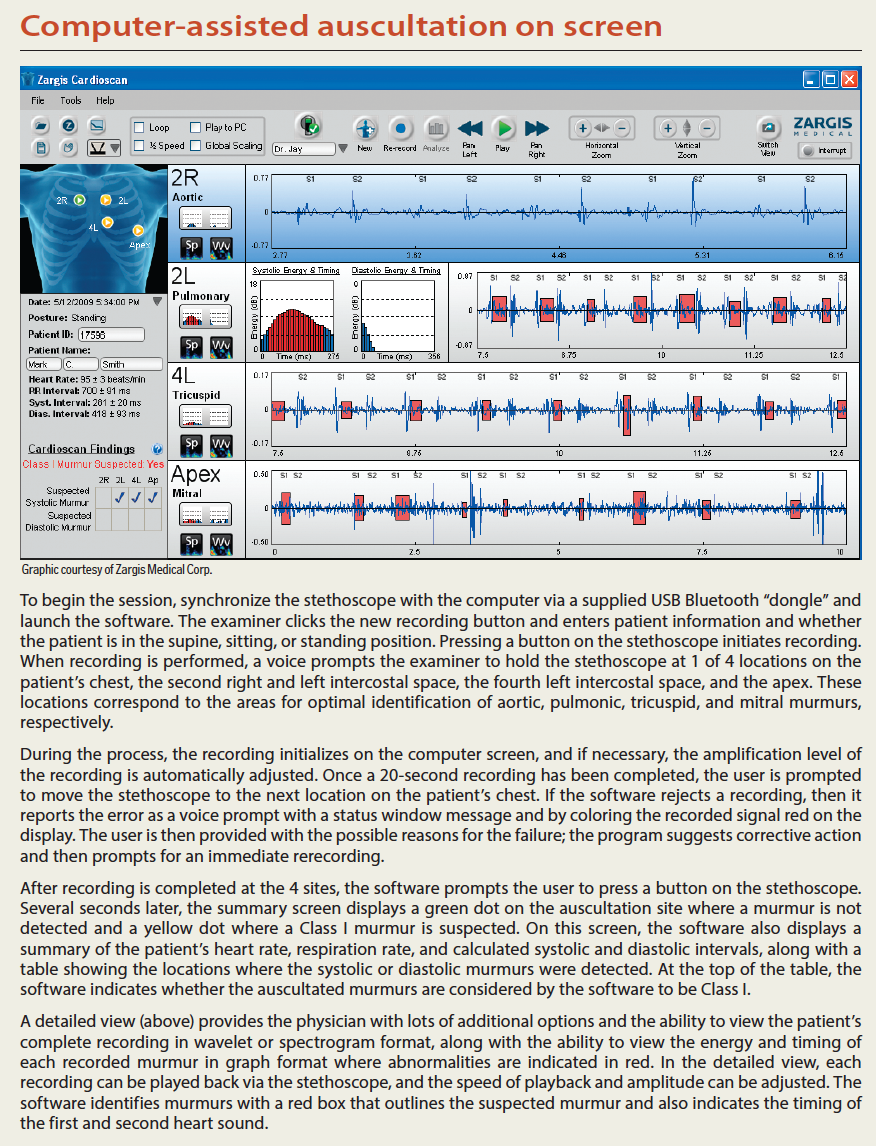
Computer-assisted auscultation on screen
When I first wrote about high-tech pediatric offices more than 20 years ago, I could not imagine the role computer-based technologies would play in pediatric practice. Today, many pediatricians use otoacoustic emission tests to rapidly screen infants and children for hearing loss and photoscreeners to identify children who have amblyopia, strabismus, or those who may need glasses. Some of us are even using computer-based surveys to screen our patients for autism, behavior problems, and attention deficit hyperactivity disorder. Last year, another new computer-based screening technology became available for the primary care pediatrician with the introduction of the Bluetooth-enabled Electronic Stethoscope Model 3200 (3M Littmann). The stethoscope wirelessly communicates with a computer running Cardioscan software developed by Zargis Medical. The software analyzes auscultated heart sounds to determine whether a heart murmur is present, and if so, recommends whether an echocardiogram is indicated. This new technology is called computer-assisted auscultation (CAA), and it could help primary care pediatricians make more appropriate referrals to pediatric cardiologists.
Murmurs are common
The incidence of heart murmurs can be as high as 80% to 90% in the pediatric population, yet the vast majority of auscultated murmurs in children are innocent (ie, not associated with structural heart disease).1,2 This creates a dilemma for the pediatrician who, on hearing a previously undocumented murmur in a child during routine examination, must decide whether the murmur merits further investigation, typically by referral to a pediatric cardiologist.
A primary care pediatrician’s ability to distinguish innocent from pathologic heart murmurs based solely on auscultation pales in comparison to that of the pediatric cardiologist who typically spends 3 or more years in training, refining his or her auscultation skills. A Duke University study showed that pediatric residents could distinguish innocent murmurs from 4 common heart conditions with an accuracy of only 33%.3 Experienced physicians fare only slightly better. Rajakumar and colleagues reported that general pediatricians could correctly distinguish innocent from pathologic murmurs only 55% of the time.4
In contrast, pediatric cardiologists do not always need to corroborate their auscultation diagnosis with an echocardiogram. In 2 studies, pediatric cardiologists demonstrated the ability to distinguish innocent from pathologic heart murmurs with sensitivities as high as 98%.5,6 As a result of the relatively poor auscultation skills of primary care physicians, at least 60% of murmurs referred to pediatric cardiologists end up being nonpathologic (ie, innocent murmurs).7 This is not to say that such referrals are inappropriate, but any method that can improve primary care physicians’ diagnostic acumen would save significant medical expenses and unwarranted parental concern as well.
Indications for echocardiography
Auscultated heart sounds correspond to physiologic and anatomic events of the cardiac cycle and are associated with closing of heart valves, vibrations of the heart walls, and vibrations of the major heart vessels associated with blood flow. According to the 2006 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for the management of patients with valvular heart disease, the production of murmurs is because of 3 main factors.8 The first is because of high blood flow rate through normal or abnormal orifices; the second is because of forward flow through a narrowed or irregular orifice into a dilated vessel or chamber; and the final reason is a regurgitant flow through an incompetent valve, septal defect, or patent ductus arteriosus.
The incidence of structural heart disease in children is less than 1%, and therefore, most auscultated murmurs are because of turbulent flow through the cardiac chambers. Echocardiography can distinguish a functional murmur from one that is pathologic and is recommended according to the ACC/AHA guidelines for asymptomatic patients with diastolic murmurs, continuous murmurs, holosystolic or late systolic murmurs, and mid-systolic murmurs of grade 3 or higher.8 These are considered Class I recommendations for echocardiography. The ACC/AHA guidelines also suggest that echocardiography can be useful in investigating any murmurs associated with signs or symptoms of heart disease, such as syncope or chest pain with exertion and/or abnormal chest x-rays (CXRs) or electrocardiograms (ECGs). These are considered Class IIa indications for echocardiography.
Echocardiograms are not always performed when a patient with a murmur is referred to a pediatric cardiologist for an evaluation. This decision is based on the patient and family history, evaluation of ECG and CXR, and the pediatric cardiac exam that includes evaluation of blood pressure and pulses as well as auscultation. In many instances, these findings allow pediatric cardiologists to identify physiologic murmurs and may save the cost of echocardiography, which can exceed $800 per study.9 Many pediatric cardiologists recommend that physicians refer patients with suspect murmurs to them rather than reflexively ordering an echocardiogram.
A lost art
A variety of factors likely contribute to the suboptimal auscultation skills of many primary care physicians-including minimal auscultation training in residency, lack of practice, variations in listening ability, and the need to expedite office visits. The majority of heart sounds and murmurs occur in the frequency range of 5 Hz to 800 Hz. Because human ears are most sensitive to sounds in the 500 Hz to 4000 Hz frequency range, many murmurs need to be amplified via stethoscopy for them to be appreciated by examiners.10
Auscultation is also restricted by the physical limitations of the human ear, which is susceptible to temporary or permanent hearing deficits. The human ear is also subject to psychoacoustic phenomena called temporal masking, which can affect an auscultator’s ability to interpret cardiac sounds. Because of temporal masking during auscultation, one sound may obscure another sound that is in close temporal proximity.
New technologies in cardiac diagnosis
Computers, however, have no frequency limitations, and their sensitivity to sound depends primarily on the sensitivity of microphone sensors used. Computers convert sound waves into digital signals, and signal-processing technology facilitates the examination of the resultant data. In 2006, researchers from Helsinki, Finland, demonstrated that murmurs recorded in a phonocardiogram could be analyzed with the help of computer software to determine murmur frequency, intensity, and duration. They showed that with computer assistance, pathologic pediatric heart murmurs could be identified with a 90% sensitivity and specificity.11 Software engineering science has continued to evolve, and today, engineers have developed sophisticated signal-processing algorithms built on the concept of neural networking (ie, teaching computers to learn the same way the human brain does). These computer algorithms enable computers running CAA software to distinguish between physiologic and pathologic murmurs automatically within a standard cardiac examination.
Computers and clinical decisions
Physicians have used computer-based devices in hospitals for many years. Computer technologies are at the core of our spirometers, electrocardiograms, and electroencephalograms, as well as many diagnostic radiology devices such as computerized tomography scanners and magnetic resonance imaging scanners. These devices facilitate patient diagnosis by producing data that must be interpreted by clinicians with specialized training.
In contrast, otoacoustic emission tests and photoscreeners evaluate recorded digital information and then render a diagnostic screening decision, which physicians then pursue as appropriate. These “interpretive” screening devices represent a new category of medical technology that is described by informatics experts as a clinical decision support system (CDSS). The computers integrated into these devices represent clinical tools that assist providers with the diagnostic process.
CAA is the newest CDSS technology and may herald a new era in medical technology. Although CAA cannot identify the cardiac pathology associated with each heart murmur, it is proving to be useful in helping physicians make more appropriate referrals.
A study was published last year in which 7 primary care physicians (including 3 pediatricians) were asked to classify 100 heart sounds as having or not having a murmur-and when a murmur was present to classify it as innocent or pathologic when using auscultation alone versus using CAA.12 In the study, CAA improved the sensitivity of correctly identifying pathologic murmur cases from 82.4% to 90.0% and improved the specificity of correctly identifying benign cases (with innocent or no murmurs) from 74.9% to 88.8%. In addition, the average physician’s referral accuracy increased from 70.4% to 82.9% using CAA. Physicians were also able to reduce their average false-positive referral rate for nonmurmurs and innocent murmurs from 36.5% to 21.4%, while simultaneously reducing their false-negative referral rate for pathologic murmurs from 13.3% to 7.1%.
Years in the making
Alan Stein, MD, a physician as well as an engineer, is the chief medical and technology officer for Zargis Medical Corp, the company that developed CAA software. He speaks with great passion about the potential for computers to assist physicians in providing medical care. When asked to explain how the CAA software performs its analysis, he said, “The process by which our software detects and classifies suspected murmurs is analogous to the algorithms used for speech recognition. The digital auscultation is transmitted from the stethoscope to the personal computer for analysis. After some basic signal processing, it becomes a statistical process to map murmur events as they occur in the heart sound recording. Heartbeats may have beat-to-beat variability, but we ultimately desire an aggregate judgment of the auscultation: ‘Was there a murmur? If so, does it meet the Class I guidelines for referral for echocardiography?’ So some intermediate metrics are computed, and the software then computes an aggregate view of murmur energy present in the entire 20-second recording. It is a relatively simple way of visualizing the amplitude of murmur energy and timing with respect to the cardiac cycle. The software is then able to easily distinguish a mid-systolic murmur from a diastolic murmur based on these computations.”
It took close to a decade to develop the algorithms necessary to make the CAA software accurate and reliable. Even so, the software will not perform an analysis when the patient’s heart rate is less than 50 beats per minute (bpm) or more than 120 bpm. This currently limits its use in the newborn nursery, where this new technology would be perhaps most valuable. Dr Stein says he thinks that CAA has great potential and explains, “We’ve had electronic stethoscopes for decades which have been capable of amplifying signals and applying preset sound filters. But digital stethoscopy implies that the full benefits of digital computing can finally be available to auscultation. This means signal transmission to multiple clinicians halfway around the globe without any loss in quality, automated algorithms that detect and diagnose disease, and the ability to record and process vast quantities of data thereby enabling new methods of wellness monitoring.”
CAA in practice
When I use CAA in my exams, parents are quite impressed with the technology. It has been my practice, when appropriate, to share my observations of physical findings with parents. This helps with their understanding of my diagnosis and motivates parents to comply with my recommendations. Before CAA, if I heard a suspicious murmur, parents had to wait several weeks until their child was evaluated by a cardiologist.
CAA is extremely easy to use. The software uses a voice to guide the user through a brief process in which the stethoscope records 20-second sequences of heart sounds at 4 different positions on the patient’s chest. Once completed, the software analyzes the recorded sounds and, in seconds, the software indicates whether the murmur or murmurs detected have a Class I recommendation for echocardiography.
Parents watch the brief recording session intently, and after the CAA software analyzes the murmur, they are reassured when it reports that a referral is not warranted. CAA allows me to relisten to the recorded murmur and assures me, “I really heard what I heard.”
Based on the patient’s history and my own judgment, I do often make a referral when the software reports that a Class I murmur was not suspected if I still think a further evaluation is warranted. This is particularly the case with murmurs I detect in infants. After using CAA for several months, my ability to identify innocent heart murmurs has definitely improved and is a welcome benefit of this technology.
Implications for the pediatrician
CAA is a welcome addition to our limited arsenal of office screening devices. CAA is relatively inexpensive. The stethoscope and software combination costs less than $900, and laptop computers cost less than $500.
Unlike vision and hearing screenings, CAA is not intended to be used on every patient-only when the primary care pediatrician hears a suspicious murmur. Given the high incidence of heart murmurs in the pediatric population, I use it often. Currently useful in evaluating heart murmurs, with some modification CAA technology could eventually be used to assist pediatricians managing children with respiratory infections and reactive airway disease. Perhaps soon, our computers will be able to analyze simultaneous data received from several sources, including pulse oximeter, auscultation, spirometry, and ECGs, further enhancing our diagnostic abilities.
Although it is easy to get excited about innovation, one must be very cautious when any new technology is introduced. When ear thermometers first came out 20 years ago, we were all excited about the technology. Studies showed that these devices had limitations, and pediatricians learned that ear thermometers should be used as screening devices and not when temperature measurement was critical (ie, in deciding when a young infant needed an evaluation for possible sepsis).
CAA must be scrutinized carefully in independent studies to best determine its limitations as well as advantages. The current CAA software sensitivity for detecting Class I murmurs as reported to the FDA is 97%, which means that the software reports very few false negatives and is very good at detecting murmurs that are likely to be nonphysiologic. The software’s specificity is only 76%, meaning that the software does report some false-positive results, and there will continue to be murmurs it reports as referable that will be discovered to be benign. CAA is not perfect in its analysis, but much better than what pediatricians are capable of doing without computer-based technology.
The few pediatric cardiologists I’ve shown the stethoscope and software to have been impressed, and some have even expressed concern that their services may be made obsolete by computers. I reassured them that this would never be the case and that the listening abilities of pediatric cardiologists will continue to be essential to pediatric cardiac auscultation for many years.
References:
1. Harris JP. Consultation with the specialist. Evaluation of heart murmurs. Pediatr Rev. 1994;15(12):490-494.
2. Hoffman JI. Incidence of congenital heart disease: I. postnatal incidence. Pediatr Cardiol. 1995;16(3):103-113.
3. Gaskin PR, Owens SE, Talner NS, Sanders SP, Li JS. Clinical auscultation skills in pediatric residents. Pediatrics. 2000;105(6):1184-1187.
4. Rajakumar K, Weisse M, Rosas A, et al. Comparative study of clinical evaluation of heart murmurs by general pediatricians and pediatric cardiologists. Clin Pediatr. 1999;38(9):511-518.
5. Smythe JF, Teixeira OH, Vlad P, Demers PP, Feldman W. Initial evaluation of heart murmurs: are laboratory tests necessary? Pediatrics. 1990;86(4):497-500.
6. Geva T, Hegesh J, Frand M. Reappraisal of the approach to the child with heart murmur: is echocardiography mandatory? Int J Cardiol. 1988;19(1):107-113.
7. McCrindle BW, Shaffer KM, Kan JS, Zahka KG, Rowe SA, Kidd L. Factors prompting referral for cardiology evaluation of heart murmurs in children. Arch Pediatr Adolesc Med. 1995;149(11):1277-1279.
8. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; Bonow RO, Carabello BA, Danu C, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006;114(5):e84-e231. Erratum in: Circulation. 2010;121(23)e443. Circulation. 2007;115(15):3409.
9. Danford DA, Nasir A, Gumbiner C. Cost assessment of the evaluation of heart murmurs in children. Pediatrics. 1993;91(2): 365-368.
10. Pelech AN. The physiology of cardiac auscultation. Pediatr Clin N Am. 2004;51(6):1515-1535, vii-viii.
11. Noponen AL, Lukkarinen S, Angerla A, Sepponen R. Phono-spectrographic analysis of heart murmur in children. BMC Pediatr. 2007;7:23.
12. Watrous RL, Thompson WR, Ackerman SJ. The impact of computer-assisted auscultation on physician referrals of asymptomatic patients with heart murmurs. Clin Cardiol. 2008;31(2):79-83.