Improve compliance to save your medical home
Making some simple changes to your practice can improve patients’ compliance and keep them loyal to your medical home.
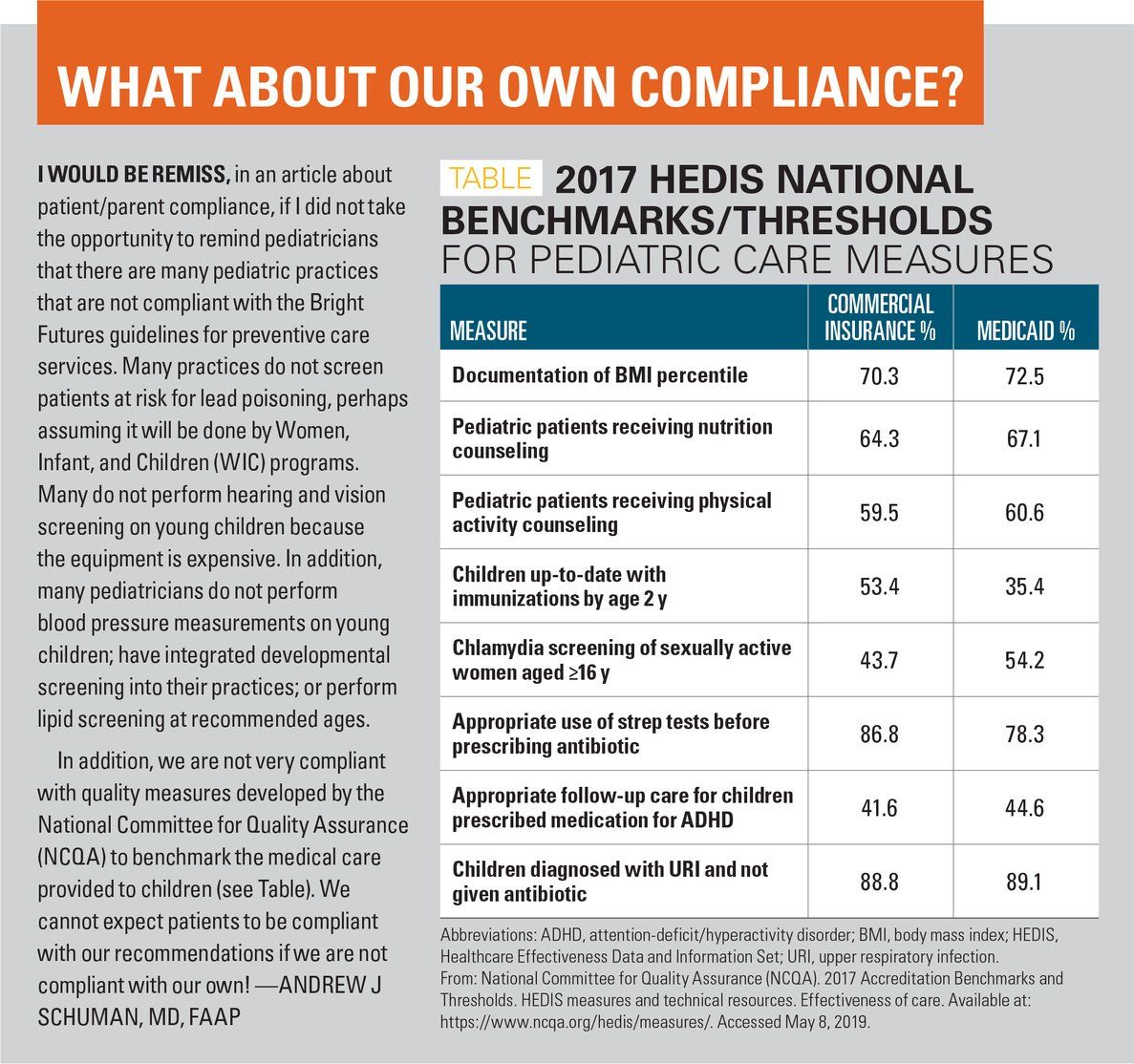
Table
Unfortunately, patients are often noncompliant with recommendations by pediatricians. Many parents fail to fill prescribed medications, and those that do often do not complete a full course of therapy. Patients frequently do not see consultants once referrals are made or make dental appointments for their children.
Let’s take a look at the many reasons for noncompliance among patients and parents, and detail solutions that will improve compliance rates for a wide variety of issues.
Routine care outside the medical home
One of the most egregious compliance failures is when patients don’t see their primary care physician for routine illnesses or well-child checks and choose instead to utilize urgent care clinics (UCCs).
There are many reasons for this. First and foremost, office visits can be expensive, and most parents have high-deductible insurance plans as a consequence of the Affordable Care Act. Parents save substantially by using the UCC down the street rather than making an appointment to be seen in your office. Many pediatric practices do not provide the extended evening and weekend hours that UCCs provide, and many practices do not facilitate access to care (see “Improve your practice: Facilitate patient access, Contemporary Pediatrics, January 2017).
In many pediatric practices, parents may be subjected to long waits on hold in order to speak with a secretary; convenient appointments often are not available; and patients are sometimes compelled to speak with a triage nurse even before an appointment is permitted to be scheduled. Additionally, if a family is enrolled in a large practice, they may not be able to see their own primary care provider due to availability of appointments.
As a consequence, the patient’s “medical home” is broken, care is fragmented, and unless practices take appropriate actions to remedy this situation, parents will continue to utilize UCCs. (See “Renovating your medical home,” Contemporary Pediatrics, July 2014).
The solution is simple. You need to modify your practice to compete with UCCs. This means modifying your practice style to improve availability; lower patient costs (see “How to help parents cut healthcare costs,” Contemporary Pediatrics, February 2018); and modify your schedule to accommodate walk-in patients.
If patients had a choice, most would prefer to see their own physician who is familiar with the patient and family. Primary care pediatricians can promote patient allegiance, and dissuade patients from using UCCs, by adopting the policy of shared decision-making; ie, giving patients options for diagnosis strategies and managements. By partnering with patients, rather than providing inflexible recommendations, compliance is likely to improve significantly.
Compliance varies with diagnosis
Parents’ compliance with recommendations depends on the parental perception of the diagnosis as well as the consequences of noncompliance. For example, consider a child with new-onset seizure disorder. Seizures are a dramatic and frightening event for children and families. Parents will tend to be compliant with administering anticonvulsant medication in order to prevent further seizures and will almost always attend follow-up visits for repeat electroencephalograms (EEGs), imaging studies, and neurologists’ consultations. Similarly, one would expect excellent compliance on the part of parents whose children are diagnosed with cancers, hematologic disorders, and diabetes, to name a few. For these conditions, the lack of compliance may have devastating consequences.
In my experience, responsible parents of children with attention-deficit/hyperactivity disorder (ADHD) who are well controlled with medication are likely to make and keep regular follow-up appointments for medication renewals. In contrast, when patients are given a less “profound” diagnosis, for which the consequences of noncompliance are likely not severe, then parents are likely to let follow-up appointments slip, and only seek new guidance when there are exacerbations of a chronic medical condition. Examples of these situations are many and include compliance for regimens given for constipation, allergies, asthma, and many others.
Make compliance easy
It is easier to comply with a provider’s recommendations when your practice makes efforts to facilitate compliance. Parents are much more likely to agree to have a lead screening and hemoglobin test done if you perform these tests in your office using point-of-care devices. Consider offering the fluoride varnish application to young patients so parents will not need to visit their dentist to have this done. If a child fails an otoacoustic emission (OAE) hearing screen, it would be advantageous to be able to perform a pure tone audiogram in your office rather than refer a patient to an audiologist.
Consider performing point-of-care polymerase chain reaction (PCR)-based strep tests so patients won’t need to wait for lab confirmation days later when a throat culture returns. In addition, many pediatricians have integrated mental health providers including psychiatrists or psychologists into their practice to facilitate access to mental health services. There are many ways practices can be creative in order to improve compliance.
Use education and care coordinators
Another way to improve compliance is to educate parents about the consequences of noncompliance. These may include recurrence of an ear infection if the antibiotic is not administered correctly or for the duration recommended; wheezing in the asthmatic child who fails to take controller medications regularly; or out-of-control blood sugars for the diabetic child who does not monitor sugars as advised. Reminders sent by e-mail can be helpful.
Helpful, too, is the incorporation of a care coordinator, usually a nurse with special training, into your practice. Following a visit, have selected patients visit your care coordinator prior to checkout. The coordinator can book referrals and schedule imaging studies, which will dramatically increase the likelihood of compliance. Thus, the patient leaves with a scheduled appointment for services in hand, rather than “getting around” to making the appointment themselves. The coordinator also can be used to reinforce instructions you provide patients, or, if necessary, take a few minutes to educate patients.
Care coordinators also can be utilized to contact patients several days following a visit to check in. These calls are much appreciated by patients and build confidence in you and your practice, increasing the likelihood of future compliance.
Telehealth improves compliance
I’ve been a fan of Telehealth for years. Now that my state has mandated coverage for Telehealth visits, I have assimilated this service into my own clinic and use it routinely.
Although I typically use Telehealth visits for patients being treated for ADHD, depression, and anxiety, such visits can be used for patients with acne, asthma, conjunctivitis, rashes, and other conditions not requiring auscultation or an otoscopic examination. A telehealth visit also can be used by nursing staff to triage patients and provide advice.
Because FaceTime video communications are now universally accepted by patients, pediatric practices would be well advised to have nursing and office staff communicate with patients via HIPAA-compliant video calls. (The Health Insurance Portability and Accountability Act [HIPAA] of 1996 provides data privacy and security for patients’ medical information.) One can communicate more effectively by interacting with parents and patients face-to-face as you do in the office, because this method lets you determine the parent’s level of concern and visually determine where and when an ill child needs to be seen.
In conclusion
This article has described measures that will improve patient access and compliance with your recommendations. If you transform your practice, you will be able to preserve the patient’s medical home and encourage parents to bypass the UCCs that are now on every street corner.
Anger hurts your team’s performance and health, and yours too
October 25th 2024Anger in health care affects both patients and professionals with rising violence and negative health outcomes, but understanding its triggers and applying de-escalation techniques can help manage this pervasive issue.