Living past cancer: Late effects and long-term care
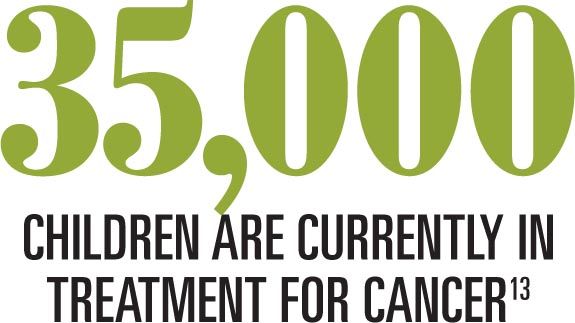
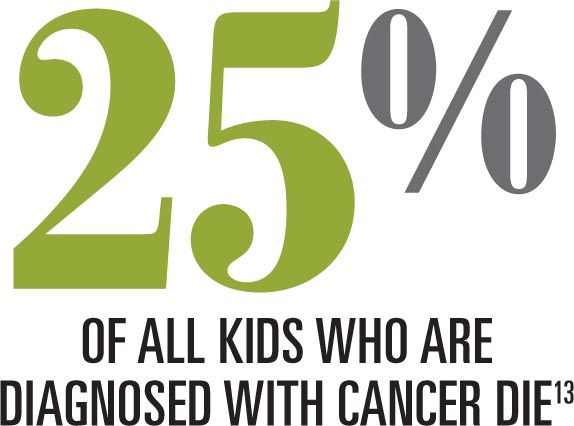
Whereas the incidence of cancer among kids is increasing, death from childhood cancer is decreasing.
Whereas the incidence of cancer among kids is increasing, death from childhood cancer is decreasing.1,2 As a result of increased survivorship, pediatricians need to think of cancer more like a chronic disease and develop strategies and practices to improve the health and well-being of their patients. Unfortunately, this is not a role that many physicians experienced in residency or received much formal training in since completing residency.
As primary care physicians, we will play significant roles in the care of our patients throughout their cancer journey: making a diagnosis; referring patients for further workup and treatment; monitoring for late effects of the cancer and treatment; providing emotional support; following up after treatment; and assisting with palliative and end-of-life care if treatment is not successful.
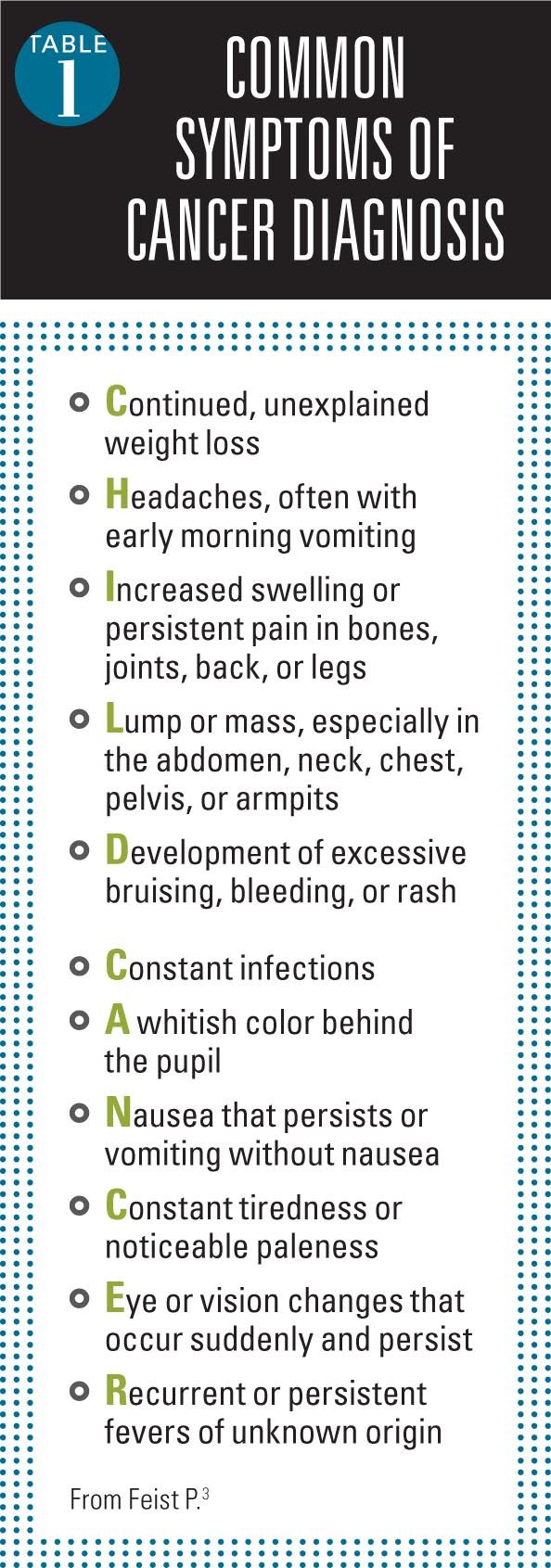
Making a diagnosis
Cancer can be elusive, and it is rarely at the top of the differential for patients presenting to our outpatient offices with common complaints. An acronym from the Pediatric Oncology Resource Center outlines many of the most common symptoms that may signal a possible cancer diagnosis (Table 1).3
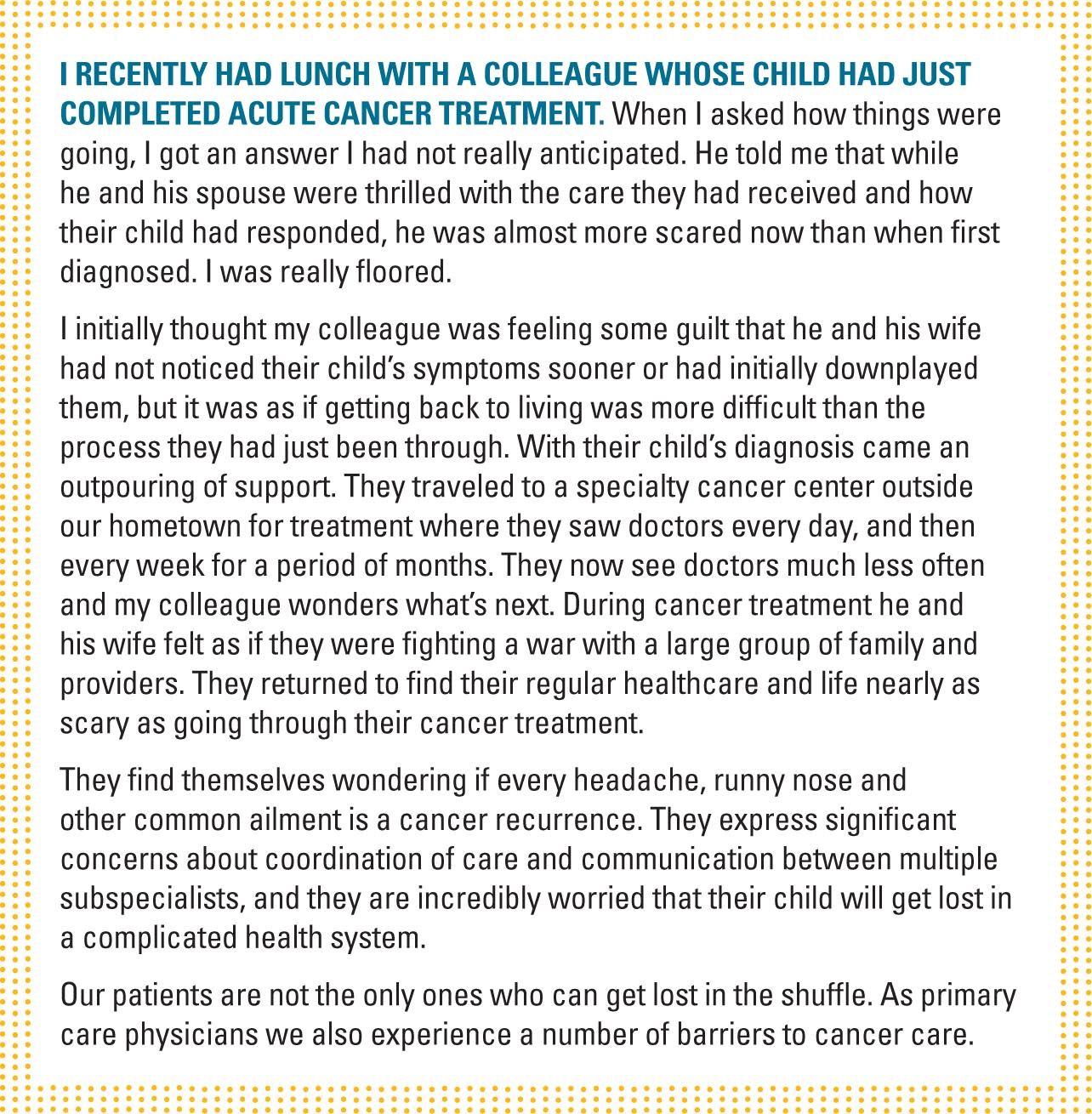
Patient barriers in cancer survivorship
Once our patients become cancer survivors and enter into long-term follow-up, a number of different barriers exist, including fragmented care, lack of education, and problems in communication.
Fragmented delivery system
Pediatric cancer care is probably at bigger risk for fragmentation compared with adult patients because of specialization and regional availability of cancer services. Whereas continuity of care is extremely important, our systems have not performed well.4 While in active treatment, the patient may see a surgeon, oncologist, radiation oncologist, and other healthcare providers in addition to the primary care physician.
Continuity of care can be thought of as “. . . the systematic assurance of uninterrupted, integrated medical and psychosocial care of the patient, in accord with the patient’s wishes, from assessment of symptoms in the prediagnostic period, throughout the phase of active treatment, and for the duration of posttreatment monitoring and/or palliative care.”5
Ultimately, poor coordination of care will lead to poor quality of care.
Lack of knowledge
While it is better in pediatrics compared with adult populations of cancer survivors, only 35% of 635 members in the Childhood Cancer Survivorship Study identified that previous cancer treatment could lead to a serious medical condition.6 In that study, 45% responded negatively and nearly 20% did not know the impact. Additionally, only small numbers of patients received written summaries of their care to give to future provides to assist in their follow-up.
Poor communication
It appears there is a disconnect between what we as a profession want to talk to our patients about following cancer treatment and what our patients want.
I think that this is likely what happened to my colleague. He and his wife were concerned with the fear of recurrence; the impact that this experience had on their relationship with their other children; potential impacts on their ability to continue to work as they had before their child’s diagnosis; and other ongoing health challenges. They did not really feel that these issues were addressed at all as part of their treatment. I also wonder how the 90 million Americans that have inadequate literacy skills deal with complicated follow-up on top of the same stresses my colleague experienced.
Our patients are not the only ones who experience barriers. We often experience the same fragmentation in attempting to get advice or records from multiple providers and centers. Often we are not reimbursed adequately to ensure delivery of comprehensive, coordinated care for complicated patients such as pediatric cancer survivors. Additionally, most of us have not had formal education in cancer survivorship, and often there are no standards related to survivorship care. However, there is something we can do to overcome some of these barriers.
Survivor care plan
Much like an asthma care plan for asthmatics, our cancer survivors need a survivorship care plan (SCP). This is a written document that patients can have and take with them. An SCP outlines their diagnosis, treatment, and possible consequences of their cancer. Many times the transition back to a primary care physician can be chaotic, much like what I have described about my colleague. If he were not a physician, I wonder how he would know:
- How often does his child need to follow up with his primary care physician (PCP)?
- How often does his child need to go back and see his cancer specialist?
- What tests should be performed as part of the postcancer treatment plan?
- How will his child be monitored?
- How will care be coordinated between the cancer specialist and the PCP?
Whereas SCPs are becoming more common, they are not commonly used. It seems reasonable to ask for an SCP from our consultants or have the patient ask for such a document.

An SCP can help bridge this gap of care (Table 2).
Having SCPs may help prevent our patients from falling through the cracks, provide a plan of care, and help us anticipate therapies and screenings they need. These SCPs are very important because patients are less likely as adults to tell doctors about pediatric cancer and they do not often have discussions with their doctors about their cancers as adults.7 In addition, SCPs provide families with reassurance because they know the long-term complications for which their child is at risk and how the child will be screened for them. Examples of care plans can be downloaded from the Memorial Sloan Kettering Cancer Center.
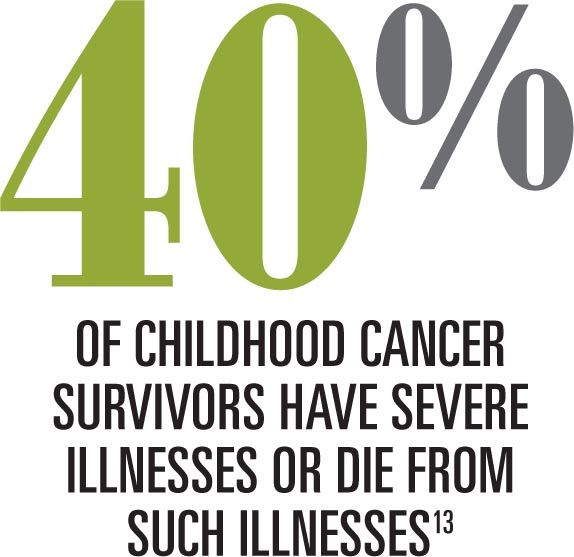
Late effects of cancer
With the improved survival of pediatric cancer, we are going to see as many as 75% of patients develop late effects (either a treatment-related toxicity or complications from the primary cancer).8,9 Late effects will be dependent on the patient’s treatment-one reason why developing an SCP is important. Recommendations for follow-up and screening based on the patient’s treatment may be obtained from the Children’s Oncology Group’s website, www.survivorshipguidelines.org/. In general, the younger the patient is when he or she begins treatment, the more risk he or she has for many late effects. Some of the late effects may include the following.8
Growth and development
Chemotherapy or radiation can lead to a number of problems. Growth failure and delayed sexual development can result from either chemotherapy or radiation and are more common the younger the age at which treatment begins. If growth hormone deficiency is suspected, obtain a bone age x-ray, consider other causes of growth problems such as hypothyroidism, and refer to an endocrinologist if abnormal.8,9
Female prepubertal cancer survivors may experience a spectrum of gonadal dysfunctions depending on their treatment, ranging from delayed puberty to premature menopause. Yearly Tanner staging is recommended until the patient is sexually developed. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), and estradiol are recommended at age 13 years and with any clinical indication such as irregular menses. Male survivors whose treatment increases risk for urologic/reproductive problems need yearly follow-up to assess pubertal and hormone status. Testosterone, FSH, and LH are recommended yearly with endocrinology follow-up for abnormalities.8
Learning issues and developmental problems such as attention-deficit/hyperactivity disorder have been attributed to cranial radiation.9-11 Besides a heightened awareness, monitoring will primarily be the same as screening other patients through history and physical exam.
Obesity and underweight
While obesity is increasing in both noncancer and cancer survivors and there may be a genetic variation predisposing survivors to obesity, many cancer survivors will be underweight as adults.9 Obesity is associated with the development of a number of chronic diseases and recurrence of some cancers. It is a particular complication for patients surviving acute lymphoblastic leukemia (ALL) and cranial tumors as well as a cancer diagnosis between ages 5 to 9 years. Obesity is also associated with metabolic syndrome, which is associated with a number of cardiac complications.
On the other hand, a number of other cancers such as Hodgkin disease, Wilms tumor, and non-Hodgkin lymphoma were associated with being underweight. Underweight survivors are more likely to experience adverse health and medical complications. Weights should be monitored annually and lab testing done every other year to monitor glucose and lipids.8
Cardiac
A common adverse effect of treatment with anthracyclines, cardiac problems are among the most common late effects with chemotherapy. Left untreated, asymptomatic left ventricular dysfunction can lead to congestive heart failure (CHF). Patients exposed to possible chemotherapy agents leading to these late effects will receive periodic echocardiograms and electrocardiograms.9,12
However, it may be possible to risk stratify some patients. Patients receiving low cumulative doses of anthracyclines (<250 mg/m2) have low risk of developing CHF compared with patients receiving higher doses (>250 mg/m2) and may be able to be screened less often.12
Liver
Both radiation and chemotherapy can potentially damage the liver. Blood tests to evaluate the liver should be obtained when entering long-term follow-up along with a yearly exam to check for liver enlargement.8
Pulmonary problems
If a patient received certain treatments such as bleomycin or busulfan, there may be an increased risk of pulmonary complications, especially if he or she was younger when treated or is exposed to secondhand smoke. Yearly history and exam are indicated as well as chest x-ray and pulmonary function tests 2 years after completing treatment to see if there are any problems that are not immediately apparent.8
Bone problems
Osteoporosis, osteopenia, and osteonecrosis result from failing to reach peak bone mass. These conditions are being more commonly identified in cancer survivors and can result in a number of problems such as fractures, spine deformities (kyphosis, lordosis, scoliosis), abnormal gait, or pain in bone/muscle.8,9 Periodic screening is performed with dual energy x-ray absorptiometry (DEXA) scans.
Oral health
Chemotherapy or radiation can lead to a number of dental problems following cancer treatment. Both treatments may lead to increased risk for cavities and problems with enamel, absence of teeth, or tooth development. Treatment beginning before age 5 years or a longer treatment course increases risk of these problems.8 Radiation may also increase risk of tooth sensitivity, xerostomia, alterations in taste, temporomandibular joint dysfunction, or periodontal disease.
Fertility
Women surviving pediatric cancer have a number of pregnancy-related problems. They are less likely to get pregnant than their siblings and their infants are more likely to be preterm and low birth weight. However, babies of survivors of pediatric cancer are not at increased risk for congenital malformations.9
Kidneys
It is recommended that pediatric survivors have their kidney function and electrolytes monitored at their first long-term monitoring visit and for a period of 2 years. Additionally, it is recommended that blood pressure and urinalysis be monitored yearly.8
Thyroid
Primary hypothyroidism (resulting from damage or removal of the thyroid gland), central hypothyroidism (resulting from damage to the hypothalamus or pituitary gland), or compensated hypothyroidism are common in childhood cancer survivors.8 Thyroid problems primarily affect patients receiving radiation near the thyroid gland and may occur years after treatment. Radiation affecting the thyroid gland also increases risk for thyroid nodules and thyroid cancer.
Patients receiving radiation to the head are at increased risk for central hypothyroidism. The younger a patient is when treated, the more likely he or she is to develop thyroid problems.8 In addition to examining the thyroid during a yearly exam, yearly checking of TSH and T4 is indicated in at-risk children. During times of rapid growth, screening may be recommended more frequently. Additionally, it is important to have thyroid levels checked before becoming pregnant.
Second and recurrent cancers
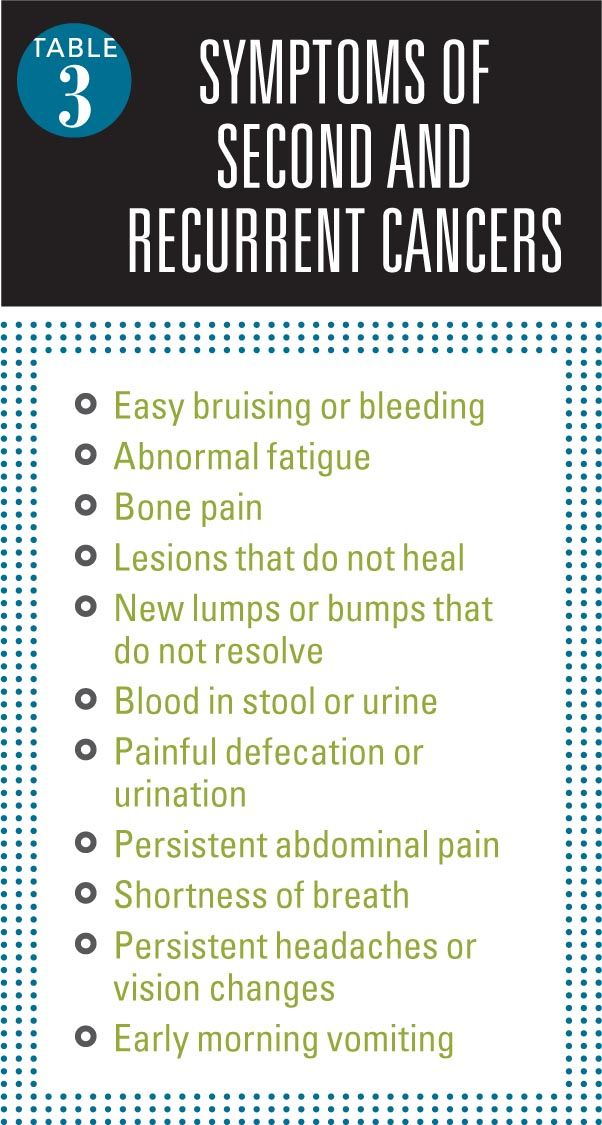
A second malignancy is the most common cause of death in patients who survive longer than 15 years. These cancers generally fall into 2 groups: 1) solid tumors related to radiation treatment; and 2) myelodysplasia and acute myelogenous leukemia related to chemotherapy.9 It is important for parents and caregivers to realize they need to report any of the symptoms (Table 3).
Additionally, all patients should avoid cancer-promoting habits such as smoking. Patients should be encouraged to exercise and adopt dietary habits such as increasing fruits and vegetables that may decrease cancer risk.
Mental health
Survivors of pediatric cancer experience a number of adverse mental health symptoms. Compared with their siblings, pediatric survivors are more likely to report depressive symptoms, somatic complaints, and posttraumatic stress disorder. As pediatric survivors grow into adulthood, they are more likely to report suicidal ideation compared with the general population. Additionally, there are a number of life situations that can potentially lead to or contribute to mental health symptoms. Pediatric survivors report increased problems related to employment (more unemployment, underemployment, and job discrimination) and marriage (less likely to marry, but no difference in divorce) compared with their siblings.9
Pediatricians’ role in cancer care
Whereas specific cancer treatment will be provided by other specialists, pediatricians will remain involved in the care of cancer survivors. We will likely make a diagnosis or refer patients for testing that will reveal a potential diagnosis. During treatment we need to be available to support families, act as a confidant to discuss alternative treatments, and support families in the decisions they make.
After the completion of treatment, we will need to participate not only in monitoring the late effects of cancer treatment, but also in monitoring for secondary cancer and cancer recurrence. I have experienced parents who sometimes want significant amounts of testing for seemingly nonserious complaints. Surprising to me, I have found very little written about this other than the previously mentioned studies that indicate we may be able to screen for cardiac conditions less frequently.
Facing a parent who is concerned that a cancer has returned when I think their child just has a regular headache is a scary thing. I don’t want to miss a recurrence, but I also don’t want to irradiate a child needlessly. Making the best clinical decision I can, trying to explain my reasoning to the parents, and providing them with close follow-up is all I know to do. Finally, I think it is important that we are available if treatment fails and parents want advice about palliation and end-of-life care.
Our role in pediatric cancer care is important first as a diagnostician, then in monitoring after treatment, and finally at the end of life. Most of our training was likely deficient in at least one of these areas, so let’s make it a point to improve our skills in this important aspect of what we do.
REFERENCES
1. Ward EM, Thun MJ, Hannan LM, Jemal A. Interpreting cancer trends. Ann N Y Acad Sci. 2006;1076:29-53.
2. Centers for Disease Control and Prevention (CDC). Trends in childhood cancer mortality-United States, 1990-2004. MMWR Morb Mortal Wkly Rep. 2007;56(48):1257-1261.
3. Feist P. Signs of childhood cancer. Ped-One Resource Center web site. Available at: http://www.ped-onc.org/diseases/SOCC.html. Published July 2005. Updated April 11, 2011. Accessed August 26, 2014.
4. Hewitt ME, Greenfield S, Stovall E, eds. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2005.
5. Lauria MM. Continuity of cancer care. Cancer. 1991;67(6 suppl):1759-1766.
6. Kadan-Lottick NS, Robison LL, Gurney JG, et al. Childhood cancer survivors' knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. JAMA. 2002;287(14):1832-1839.
7. Kirchhoff AC, Montenegro RE, Warner EL, et al. Childhood cancer survivors' primary care and follow-up experiences. Support Care Cancer. 2014;22(6):1629-1635.
8. Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. Version 3.0. Arcadia, CA: Children’s Oncology Group; 2008. Available at: http://www.survivorshipguidelines.org/pdf/LTFUGuidelines.pdf. Accessed August 26, 2014.
9. Haddy RI, Haddy TB. Lifetime follow-up care after childhood cancer. J Am Board Fam Med. 2010;23(5):647-654.
10. Zebrack BJ, Zeltzer LK, Whitton J, et al. Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin’s disease, and non-Hodgkin’s lymphoma: a report from the Childhood Cancer Survivor Study. Pediatrics. 2002;110(1 pt 1):42-52.
11. Harila-Saari AH, Lähteenmäki PM, Pukkala E, Kyyrönen P, Lanning M, Sankila R. Scholastic achievements of childhood leukemia patients: a nationwide, register-based study. J Clin Oncol. 2007;25(23):3518-3524.
12. Yeh JM, Nohria A, Diller L. Routine echocardiography screening for asymptomatic left ventricular dysfunction in childhood cancer survivors: a model-based estimation of the clinical and economic effects. Ann Intern Med. 2014;160(10):661-671.
13. American Cancer Society. National Action Plan for Childhoodf Cancer. Report on the National Summit Meeting on Childhood Cancer. 2010.
Dr Bass is chief medical information officer and associate professor of medicine and pediatrics, Louisiana State University Health Science Center–Shreveport. The author has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.
Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.
Meet the Board: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI
May 20th 2022Contemporary Pediatrics sat down with one of our newest editorial advisory board members: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI to discuss what led to her career in medicine and what she thinks the future holds for pediatrics.