Managing Asthma in Children, Part 1: Making the Diagnosis, Assessing Severity
Asthma is one of the most prevalent chronic diseases in the United States, and most medical practitioners encounter patients with asthma on a daily basis. The goal of this 2-part article is to discuss the diagnosis and management of asthma in children younger than 12 years. In part 1, we will briefly outline the epidemiology, pathophysiology, and risk factors; then we will review, in more detail, the diagnosis of asthma and the initial evaluation of asthma severity.
Asthma is one of the most prevalent chronic diseases in the United States, and most medical practitioners encounter patients with asthma on a daily basis. The goal of this 2-part article is to discuss the diagnosis and management of asthma in children younger than 12 years. In part 1, we will briefly outline the epidemiology, pathophysiology, and risk factors; then we will review, in more detail, the diagnosis of asthma and the initial evaluation of asthma severity. In part 2, we will focus on treatment. We will draw heavily on the recommendations of the Expert Panel Report 3 published by the National Asthma Education and Prevention Program in 2007,1 in addition to other current literature on the management of chronic asthma in children.
EPIDEMIOLOGY
It is estimated that 22 million persons in the United States have asthma; of these, approximately 6 million are children.2 It also is estimated that 12.7% of children younger than 18 years will receive a diagnosis of asthma at some point in their lives.2 The diagnosis is usually made before 1 year of age.
The prevalence of asthma in the United States has risen dramatically over the past 25 years. From 1980 to 1995, the prevalence doubled from 3.6% to 7.5%. Since 1995, the prevalence has continued to increase, but at a slower rate; in 2005, the estimated prevalence of asthma in children was 8.9%.2
The medical and societal effects of asthma are substantial. It has been estimated that more than 5% of all children will have an asthma exacerbation each year.2 This results in approximately 7 million ambulatory visits, almost 200,000 hospitalizations, and 13 million missed school days annually.2
PATHOPHYSIOLOGY
Asthma is probably caused by a complex interaction between the host and environmental exposures.3 The exact mechanism of the inflammatory process leading to asthma is not yet fully understood. Genetics appear to play an important part in the development of asthma, but as in other common diseases with complex causes, research aimed at finding specific genes that predispose persons to asthma has met with little success.3
It is known that inflammatory and structural changes occur in the preschool years when children experience more persistent symptoms. Bronchial biopsy and bronchoalveolar lavage (BAL) samples have been obtained to determine when these changes take place. One study demonstrated no differences in the reticular basement membrane thickness between infants with reversible airflow obstruction and asymptomatic infants and children.4 Another study found that the reticular basement membrane is significantly thicker in wheezing preschool children than it is in nonwheezing controls, but not as thick as in school-aged children who have difficult-to-control asthma.5
A predominance of neutrophils, but not eosinophils, has been noted in BAL specimens from wheezing preschool children.6 The eosinophil density is significantly greater in children with wheezing compared with nonwheezing children; however, similar changes are found in atopic children who do not have asthma.5 These data suggest that inflammatory and structural changes associated with asthma begin in the preschool years and progress during childhood, at which time they resemble the changes found in adults who have persistent asthma.
The immune system plays a role in the development of asthma and atopic disease. It is postulated that an imbalance in the regulation of TH1- type and TH2-type cytokine responses in early life leads to a down-regulation of the TH1 immune response that fights infection and a domination of TH2 cells, which leads to the expression of asthma and allergies.7,8 This theory is referred to as the “hygiene hypothesis” and suggests that early exposures to microbial sources, living in large families, less frequent use of antibiotics, and country living stimulate the TH1 response and thus have a protective effect.8
RISK FACTORS
Environmental and viral exposures also appear to play a role in the development of asthma. The initial wheezing episodes in young children are often linked to viral illnesses, such as infections caused by respiratory syncytial virus (RSV), rhinovirus, influenza virus, parainfluenza virus, and metapneumovirus.9 Both rhinovirus and RSV have been linked to initial wheezing episodes and the risk of recurrent wheezing in early childhood.10,11 It has not been determined whether these viruses directly cause asthma in a vulnerable host or whether they simply trigger an exacerbation in a child with established disease.
Exposure and sensitization to airborne allergens, including Alternaria and house dust mite, are associated with the subsequent development of asthma.12 Other exposures, such as tobacco smoke and air pollution, have been suggested to increase the risk of asthma. Possible protective factors include diets high in antioxidants and omega-3 fatty acids.1,13
In addition to the numerous genetic and environmental risk factors associated with an increased risk of asthma, 4 different phenotypes can be used to classify children with asthma and can help the clinician determine the likelihood of persistent symptoms and long-term outcome. These phenotypes include:
•Never wheeze.
•Early transient wheezing (symptoms present before 3 years of age but not present at age 6).
•Persistent wheezing (symptoms before 3 years of age and present at age 6).
•Late-onset wheezing (symptoms present after 3 years of age).14
The most common phenotype is early transient wheezing. Children with this phenotype typically have recurrent episodes of wheezing starting in the first year of life with no relation to atopy. Approximately 60% of these children have resolution of their symptoms by 6 years of age, and fewer than 25% continue to wheeze in adolescence. 13,14 Risk factors associated with this phenotype include having schoolaged older siblings,15 attending day care,15,16 exposure to cockroach allergen and house-dust endotoxin,12,16 male sex,12 and bottle feeding.16
The category of persistent wheezing can be subdivided into atopic and nonatopic persistent wheezing. 17 Nonatopic children with persistent wheezing account for almost 20% of children younger than 3 years who have recurrent wheezing.14,18 These children demonstrate significant airway reactivity and a reduced pre-bronchodilator forced expiratory volume in 1 second (FEV1).11 With time, the wheezing episodes become less frequent, and they typically resolve by the early teenage years.11 Risk factors for atopic wheezing include atopic dermatitis, eosinophilia at 9 months of age, male sex, parental asthma, and a history of wheezing with lower respiratory tract infections. 14 Children with this phenotype often also have a history of early sensitization to food allergens or aeroallergens19 and have a higher likelihood of wheezing as young adults.20,21
The late-onset wheezing phenotype has a prevalence of 15%.14 Children with this phenotype are more likely to have mothers with asthma, to be male, and to have had rhinitis in the first year of life than those who never wheezed.14
These phenotypes were defined as part of a longitudinal cohort study. As such, it may be difficult to categorize children into 1 of the 4 phenotypes when they are very young. Thus, a phenotype frequently cannot be assigned until the child is older.
DIAGNOSIS
The diagnosis of asthma requires a high index of suspicion and a thorough history and physical examination. An accurate diagnosis is important to prevent the morbidity and mortality associated with undertreatment of the disease. It also avoids the misdiagnosis of other respiratory diseases, such as allergic rhinitis, gastroesophageal reflux disease (GERD), laryngotracheomalacia, and vocal cord dysfunction-all of which mimic asthma but are not responsive to asthma treatments.
Consider the diagnosis of asthma if a child has episodic, reversible symptoms of airflow obstruction and airway hyperresponsiveness.1 There are several indicators that increase the probability of asthma in children. A key indicator is the presence of audible wheezing or a high-pitched sound on exhalation. Other indicators include a history of cough that is worse at night, recurrent wheezing, recurrent difficulty in breathing, and recurrent chest tightness.1 The symptoms often worsen with exercise, viral respiratory infections, exposure to allergens or irritants (such as smoke or chemicals), changes in weather, strong emotional responses, stress, or menses.1
Other aspects of a detailed history include the age at onset of symptoms and progression over time; timing and pattern of wheezing, including number of days or nights per week or month; use of short-acting β-agonists (SABAs); and response to SABAs. Determine whether acute or chronic episodes of wheezing are associated with different seasons, and establish a time line of previous visits to a clinic or emergency department for respiratory symptoms, hospitalizations, ICU admissions, and intubations. Explore comorbid conditions, including rhinosinusitis, rhinitis, GERD, obstructive sleep apnea, obesity, and psychological factors.1
A detailed family history of asthma, allergies, rhinosinusitis, eczema, or nasal polyps is important.1 In addition, an environmental history is essential and should include exposure to allergens; tobacco smoke; and conditions in the home, such as the type of heating and cooling systems, presence of mold or mildew, and the condition of the rooms where the child spends most of his or her time. Also explore the impact of symptoms on the child and family, such as missed school or work, limitation of activity, adverse effects on family dynamics or activities, and economic burden.1
Perform a thorough physical examination, with emphasis on the upper and lower respiratory tracts, chest, and skin. Physical examination findings can direct the clinician toward asthma or another disease in the differential diagnosis. Examine the upper airway for nasal secretions, mucosal swelling, nasal polyps, allergic shiners, and a transverse crease across the bridge of the nose that suggests allergic rhinitis. Examine the chest for the sounds of wheezing during normal expiration, prolonged expiratory phase, use of accessory muscles with breathing, and evidence of a barrel chest, which suggests chronic air trapping.1
Carefully examine the skin for evidence of atopic dermatitis. Other noteworthy points of the physical examination include growth parameters, the presence of cyanosis or clubbing in the extremities, and a neurological examination for signs of weakness. It is important to remember that normal physical examination findings do not exclude the diagnosis of asthma because of the variable nature of this disease and the fact that signs of airflow obstruction can be absent between exacerbations.1
Spirometry is recommended for all children older than 4 years in whom the diagnosis of asthma is being considered. Look for airflow obstruction that is at least partially reversible; this is determined by an increase in FEV1 of more than 200 mL or an increase of more than 12% after the inhalation of an SABA. Spirometry is preferred over peak flow measurements because the latter are limited by the child’s effort and because of the wide variability in peak flow meters and reference ranges. Peak flow meters are designed to monitor patients’ progress rather than to be used as a diagnostic tool.1
Several other studies that are not routinely necessary can aid in the diagnosis. Chest radiographs (preferably posteroanterior and lateral) are useful in the initial evaluation to look for signs of air trapping, such as flattening of the diaphragms, horizontal positioning of the ribs, hyperlucency, and increased anteroposterior diameter of the chest. Other common radiographic findings include atelectasis, particularly in the right middle lobe, and peribronchiolar inflammatory changes.22
Sensitization to allergens is a major contributor to both chronic airway inflammation and acute asthma symptoms; thus, skin prick testing or measuring antigen-specific IgE antibodies should be considered when evaluating children with asthma.1
INITIAL ASSESSMENT OF ASTHMA SEVERITY
Pharmacological therapy should be initiated on the basis of asthma severity. Severity is defined as the intrinsic intensity of the disease process. 2 The most accurate time to assess the severity of asthma in children is when they are not taking a long-term controller medication, since this allows the clinician to determine the severity of the underlying disease and initiate an appropriate treatment plan. Spirometry results help with the initial assessment of asthma severity in children 5 years or older.
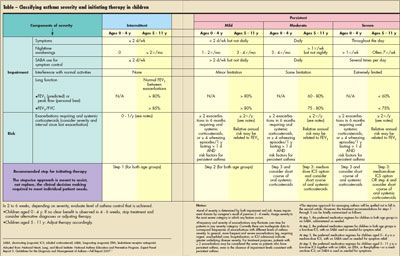
The initial assessment should classify the severity as intermittent, mild persistent, moderate persistent, or severe persistent based on the frequency of symptoms (Table). Asthma triggers and comorbid conditions should be identified. Also assess the knowledge and skills of the child and caregivers regarding asthma and their ability to identify symptoms of an exacerbation.
Guidelines for the initial assessment of severity are divided into the age ranges of 0 to 4 years and 5 to 11 years, and they take into account both impairment (symptom burden) and risk (potential morbidity).2 Impairment encompasses the severity and frequency of daytime and nocturnal symptoms, frequency of use of rescue medication, ability to perform normal daily activities, and lung function. The goals of reducing impairment include preventing chronic symptoms, minimizing the use of rescue medications, continuing baseline activity levels, maintaining lung function, and meeting the expectations of the child and family.
The category of risk includes the frequency of exacerbations that require systemic corticosteroids, the loss of lung function over time, and adverse medication effects. Risk reduction is aimed at controlling factors that lead to exacerbations and clinic or emergency department visits, preventing loss of lung function, and eliminating adverse reactions to treatments.2
Children may meet the requirements for different classes of severity based on different categories of evidence, but they should be given the severity score that relates to the highest category of symptoms.2 For example, a 5-year-old child who has had infrequent daytime and nocturnal symptoms, but has required oral corticosteroids twice in the past 6 months, has asthma that is classified as persistent and is treated accordingly.
CONCLUSION
Childhood asthma is widely prevalent in the United States. Although its exact mechanism is incompletely understood, it is probably caused by a complex interaction between the child and his or her environment. Many risk factors have been identified that might potentially be controlled. The diagnosis requires a thorough history and physical examination to exclude other common conditions that mimic asthma. Recently updated guidelines from the National Asthma Education and Prevention Program take into account both individual risk and potential impairment. These guidelines allow the clinician to easily assess the severity of a child’s symptoms. In part 2, we will discuss in depth the management of childhood asthma as set forth in these guidelines.
References:
REFERENCES
1
. National Heart, Lung, and Blood Institute: NationalAsthma Education and Prevention Program. ExpertPanel Report 3: Guidelines for the Diagnosis andManagement of AsthmaâFull Report 2007.
www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf
. PublishedAugust 28, 2007. Accessed April 16, 2009.
2
. Akinbami L; Centers for Disease Control andPrevention, National Center for Health Statistics.The state of childhood asthma, United States, 1980-2005.
Adv Data.
2006;381:1-24.
3
. Ober C. Perspectives on the past decade of asthmagenetics. J Allergy Clin Immunol. 2005;116:274-278.
4
. Saglani S, Malmström K, Pelkonen AS, et al.Airway remodeling and inflammation in symptomaticinfants with reversible airflow obstruction.
Am JRespir Crit Care Med
. 2005;171:722-727.
5
. Saglani S, Payne DN, Zhu J, et al. Early detectionof airway wall remodeling and eosinophilic inflammationin preschool wheezers.
Am J Respir CritCare Med.
2007;176:858-864.
6
. Krawiec ME, Westcott JY, Chu HW, et al. Persistentwheezing in very young children is associatedwith lower respiratory inflammation.
Am J RespirCrit Care Med
. 2001;163:1338-1343.
7
. Liu AH, Murphy JR. Hygiene hypothesis: fact orfiction? J Allergy Clin Immunol. 2003;111:471-478.8. Strachan DP. Family size, infection and atopy:the first decade of the “hygiene hypothesis.”
Thorax.
2000;55(suppl 1):S2-S10.
9
. Heymann PW, Carper HT, Murphy DD, et al.Viral infections in relation to age, atopy, and seasonof admission among children hospitalized for wheezing.
J Allergy Clin Immunol.
2004;114:239-247.
10
. Lemanske RF Jr, Jackson DJ, Gangnon RE, et al.Rhinovirus illnesses during infancy predict subsequentchildhood wheezing.
J Allergy Clin Immunol.
2005;116:571-577.
11.
Stein RT, Sherrill D, Morgan WJ, et al. Respiratorysyncytial virus in early life and risk of wheezeand allergy by age 13 years.
Lancet.
1999;354:541-545.12. Sherriff A, Peters TJ, Henderson J, Strachan D;ALSPAC Study Team. Avon Longitudinal Study ofParents and Children. Risk factor associations withwheezing patterns in children followed longitudinallyfrom birth to 3(1/2) years.
Int J Epidemiol.
2001;30:1473-1484.
13
. Moss MH, Gern JE, Lemanske RF Jr. Asthmain infancy and childhood. In: Adkinson NF, YungingerJW, Busse WW, et al, eds.
Middleton’s AllergyPrinciples and Practice
. Philadelphia: Mosby; 2003:1225-1255.
14
. Martinez FD, Wright AL, Taussig LM, et al.Asthma and wheezing in the first six years of life.The Group Health Medical Associates.
N Engl JMed.
1995;332:133-138.
15
. Ball TM, Castro-Rodriguez JA, Griffith KA,et al. Siblings, day-care attendance, and the risk ofasthma and wheezing during childhood.
N Engl JMed.
2000;343:538-543.
16
. Rusconi F, Galassi C, Corbo GM, et al. Risk factorsfor early, persistent, and late-onset wheezing inyoung children. SIDRIA Collaborative Group.
Am JRespir Crit Care Med.
1999;160:1617-1622.
17
. Stein RT, Holberg CJ, Morgan WJ, et al. Peakflow variability, methacholine responsiveness andatopy as markers for detecting different wheezingphenotypes in childhood.
Thorax.
1997;52:946-952.
18
. Martinez F, Godfrey S.
Wheezing Disorders inthe Preschool Child: Pathogenesis and Management.
New York: Martin Dunitz; 2003.
19
. Guilbert TW, Morgan WJ, Zeiger RS, et al. Atopiccharacteristics of children with recurrent wheezingat high risk for the development of childhood asthma.
J Allergy Clin Immunol
. 2004;114:1282-1287.
20
. Morgan WJ, Stern DA, Sherrill DL, et al. Outcomeof asthma and wheezing in the first 6 years oflife: follow-up through adolescence.
Am J Respir CritCare Med
. 2005;172:1253-1258.
21
. Castro-RodrÃguez JA, Holberg CJ, Wright AL,Martinez FD. A clinical index to define risk of asthmain young children with recurrent wheezing.
AmJ Respir Crit Care Med
. 2000;162:1403-1406.
22
. Dalton AM. A review of radiological abnormalitiesin 135 patients presenting with acute asthma.
Arch Emerg Med.
1991;8:36-40.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.