New model emerges for hospital-based pediatric care
In the mid-1990s, David Monroe, MD, a pediatrician in Columbia, Maryland, remembers having to admit children with common diagnoses such as appendicitis, asthma, and pneumonia to hospitals 30 or more miles away. That was because Howard County General Hospital, the community hospital in Columbia, was struggling to maintain pediatric inpatient care.
In the mid-1990s, David Monroe, MD, a pediatrician in Columbia, Maryland, remembers having to admit children with common diagnoses such as appendicitis, asthma, and pneumonia to hospitals 30 or more miles away. That was because Howard County General Hospital, the community hospital in Columbia, was struggling to maintain pediatric inpatient care.

David Monroe, MD“We tried to find a way to keep patients closer to families, keep them in our community, and still deliver good quality pediatric care,” says Monroe, an assistant professor of pediatrics at Johns Hopkins, Baltimore, Maryland, and director of the Children’s Care Center at Howard County.
Like many community hospitals nationwide, Howard County couldn’t financially justify staffing a dedicated pediatric inpatient unit with pediatric nurses because of the unpredictable and variable nature of pediatric patient flow. Winters were busier, but summers were slow. Sometimes, according to Monroe, there weren’t any patients filling those beds.
This is still a common problem today. Most community hospitals that have pediatric coverage must subsidize this care, according to Monroe.1
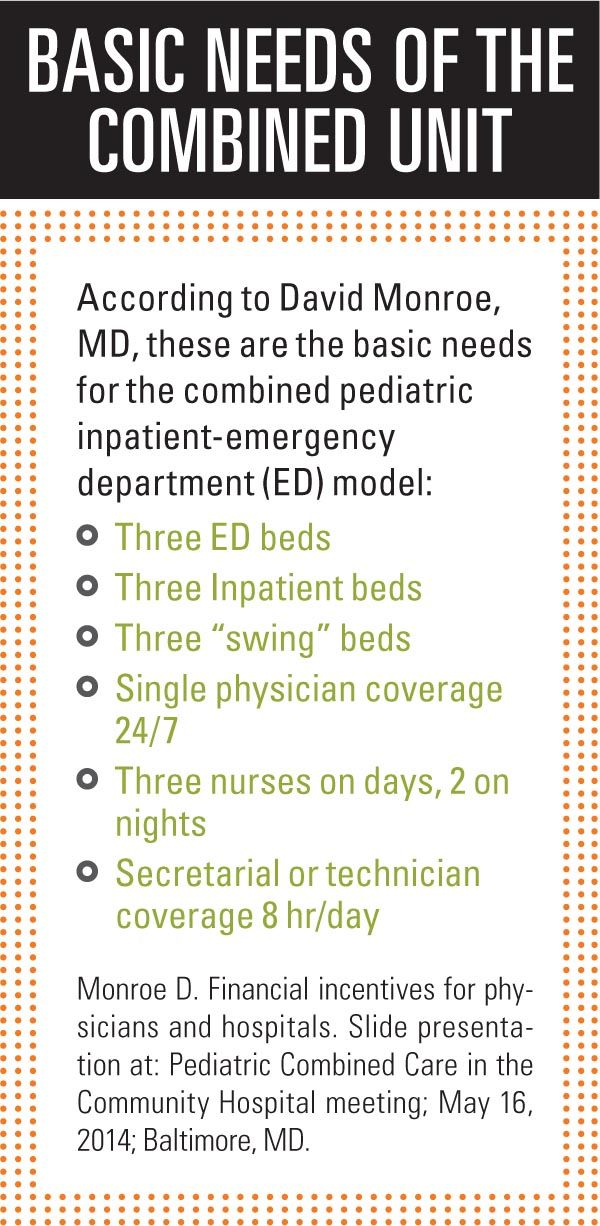
The pediatrician created a model to make the inpatient side viable by combining the pediatric emergency department (ED) with a pediatric inpatient unit, and having one staff to run both. Monroe says he figured the 5000 pediatric emergency visits the hospital had a year would drive the combination unit’s financial and staffing viability. Pediatric nurses would stay because they’d be working with only pediatric patients, and more parents and caregivers would bring their children for emergency care and inpatient care to Howard County because of the specialized approach, he predicted.
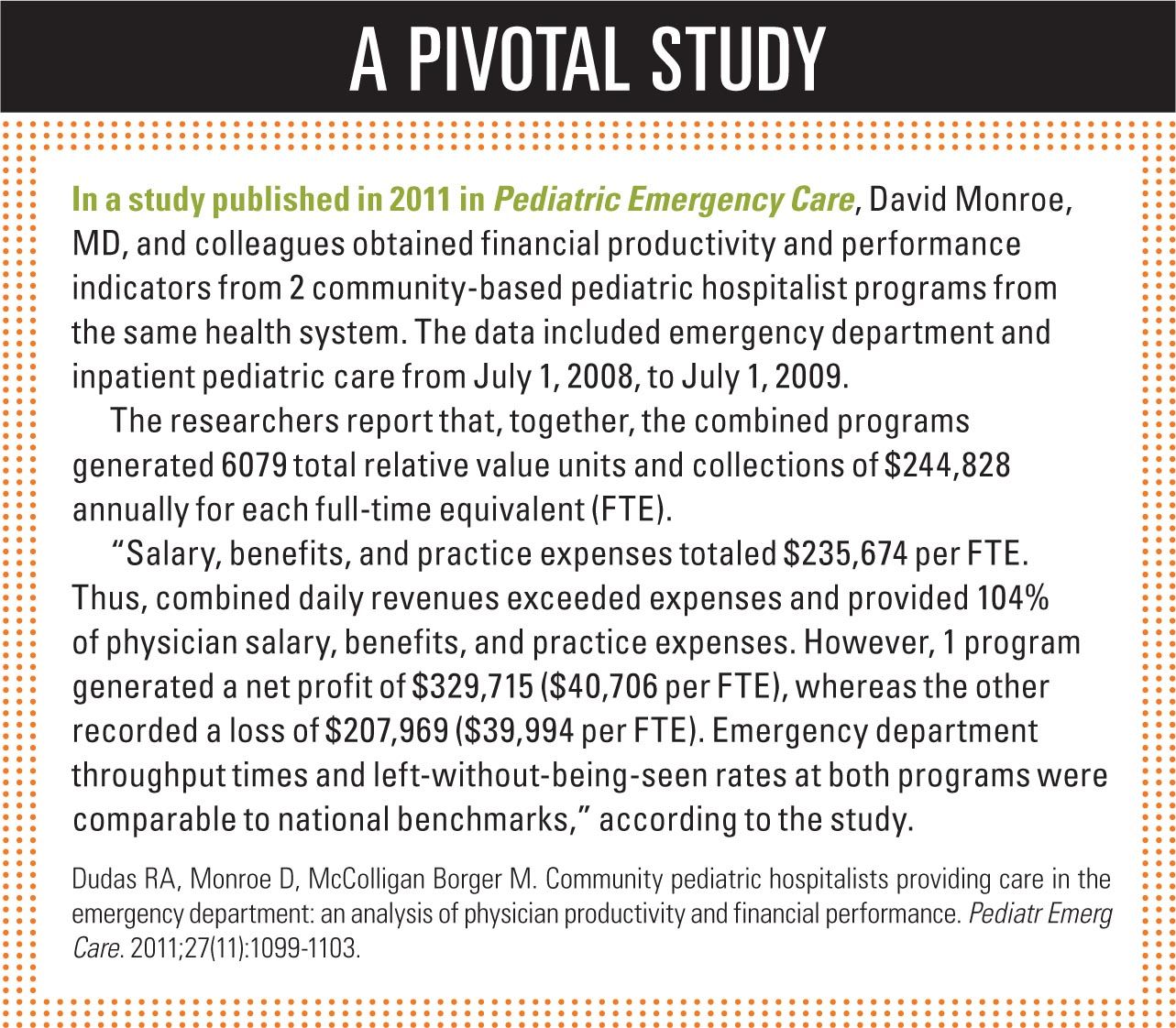
He was right. The combined unit opened at Howard County in 1997. Since then, Monroe, considered the model’s founder, has published on the concept.1
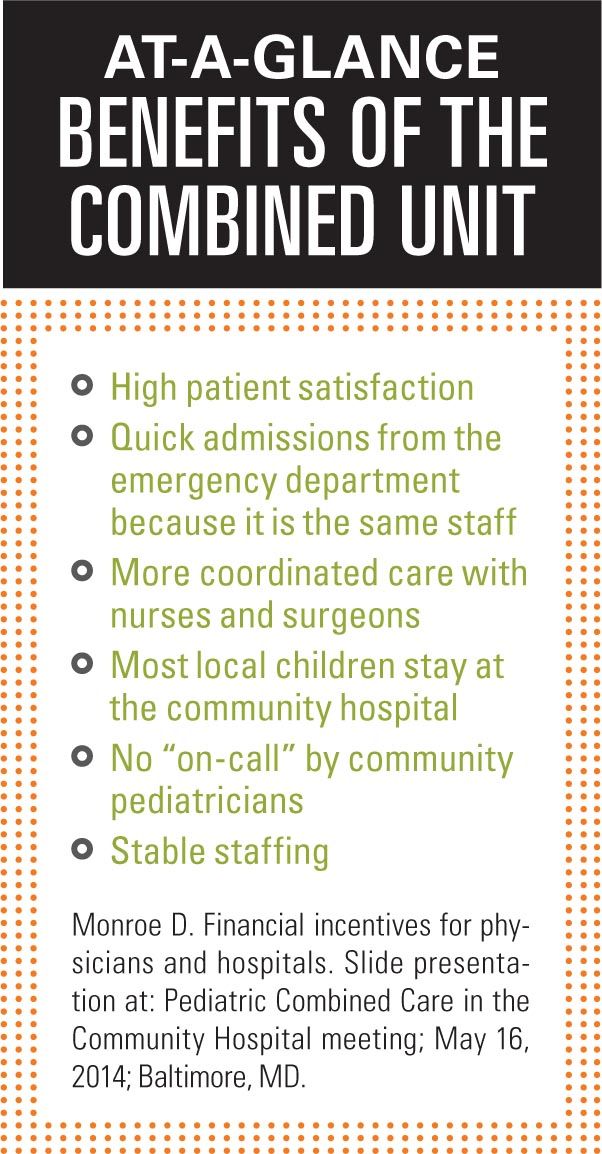
“What we found was, first, the hospital was happy because we were viable. The unit supported the full salaries for nurses and physicians, from year one all the way to now. It continues to be on the national patient satisfaction scores-if not the highest-ranking unit in the hospital, one of the highest-ranking units in the hospital. We started with 5000 patients [a year in the ED]; we’re now a little over triple that at 16,000 patients,” Monroe says.
Deliveries also have increased at Howard County, which makes sense, according to Monroe. “[It is known] that the moms often decide where the whole family gets care for every problem. So, if the moms are happy with pediatric care, they’re more likely to go to the same hospital for all their care. If the moms are happy with their delivery care, they’re more likely to come here for pediatric care,” Monroe says.
The combined unit at Howard County has been profitable for 13 to 15 years. The largest loss was $9000 out of a $2 million budget. The largest annual profit: $100,000. The losses have occurred in the last 2 years. An explanation for that, according to Monroe, could be an increasing number of local urgent care centers. “One of the nice things about the model is it’s flexible, so we’re adjusting the staff,” Monroe says.
More on the need
Pediatric inpatient volume at community hospitals has been waning for some time. “With immunizations and antibiotics, the number of hospitalized pediatric patients has gotten lower over time, and those who do need to be hospitalized often have complex illnesses that need to be taken care of at tertiary care centers,” according to Melissa M. Sparrow, MD, clinical director, inpatient and emergency services, Greater Baltimore Medical Center (GBMC), Maryland.

According to the Centers for Disease Control and Prevention (CDC) National Hospital Discharge Survey, pediatric admissions have gone from a high approaching 4 million annually in 1970 to about 2 million in 2009.2
“When you have a loss of patient volume or an unsteady volume, you can’t really maintain a care structure. A hospital can't afford full-time equivalent (FTE) staff members when you have only 1 patient on a pediatric ward 1 week and 6 patients the next week,” Sparrow says.
Greater Baltimore Medical Center opened its combined pediatric unit in 2004. The GBMC and MedStar Franklin Square Medical Center, also in Baltimore, were the second rung of US hospitals to open units based on Monroe’s model that year. Today, Sparrow teaches others about the model and in 2014 she coordinated a symposium in Baltimore for pediatricians, nurses, and community hospital administrators nationwide interested in pediatric combined care.
Pediatric units at community hospitals around the United States are having to shut down or combine with other inpatient units, such as gynecology or postoperative care, Sparrow notes. Among the problems with combining pediatrics with a nonpediatric unit is the inability to sustain highly qualified pediatric nurses, she adds. “Pediatric nurses don’t want to do a mixture of things when they have an area of expertise. They don’t want to also take care of adult patients,” she says.
Pediatric nurses, according to 1 study, find working with kids more satisfying. Researchers reported in the Journal of Pediatric Nursing that “pediatric nurses had more positive perceptions of unit support, workload, and overall nurse satisfaction than their colleagues working in nonpediatric facilities.”3
“There is also the recognition that pediatric patients treated in adult-oriented EDs don’t get the best care possible, often because they’re not seen by pediatricians,” Sparrow says. Research suggests, according to Sparrow, that children are more likely to be overadmitted and overtreated in adult EDs. “They often undergo more lab and imaging studies, like head [computed tomography] for head trauma,” she points out.

Scott Krugman, MD, MSQuality is a concern at community hospitals, says Scott Krugman, MD, MS, chairman of pediatrics, MedStar Franklin Square Medical Center. “There are concerns about the staff and training and ability to care for kids who are sick,” he says. “The combined units are 1 way to maintain highly skilled, high-quality, and high-competency people because the team is regularly caring for sick children.”
A statistics report published in 2012 suggests that many US hospital EDs do not have the recommended pediatric services, expertise, and supplies for treating pediatric emergencies.4 Researchers from the CDC reported that in 2006 only 7.2% of hospital EDs had all the recommended pediatric emergency supplies. Although 66% of children’s hospitals and hospitals with pediatric intensive care units had 24/7 access to a board-certified pediatric emergency medicine attending physician, such access was uncommon among other hospital types, according to the investigators.
Still other researchers assessed EDs’ pediatric preparedness in the United States and reported on a 2003 survey published in Pediatrics in December 2007. They wrote that 89% of pediatric (aged 0 to 14 years) ED visits occur in non–children's hospitals, and only 6% occur in a separate pediatric ED.5 Only 6% of EDs had all recommended equipment and supplies for pediatric patients. Although hospitals often have the recommended medications for children, only half of EDs surveyed had laryngeal mask airways for children.
The concept
Six community hospitals in Maryland have since combined or are in the process of combining their pediatric inpatient and ED units. A sprinkling of community hospitals outside the state-in Boston, Massachusetts, and in Missouri and New Jersey-have launched the model. In addition, there’s a lot of interest among community hospitals still struggling to maintain inpatient pediatric services, according to Sparrow.
“I’ve had many people come to us because they’re either in the process of arguing for [a combined pediatric unit] from the administration, or they’re building one and they want to know how to apportion the rooms or how to cross-train staff. There are a lot of nurses and administrators who also come to us for questions and guidance,” Sparrow says. “I’m surprised more hospitals aren’t doing it. I think this is a solution to trying to maintain quality care in the community hospital with limited resources.”
The combined model continues to have good outcomes at different hospitals. Not only does the model seem to reduce or eliminate the subsidies hospitals were paying hospitalists to staff independent inpatient pediatric units, but patients and staffs are more satisfied.
Krugman says that combining the ED and inpatient unit and having flex staffing for both areas gives a community hospital a more consistent census and the ability to adjust staff up and down more easily. “Not to mention, the biggest reason is to provide pediatric care for pediatric patients all in one location,” Krugman says.
Krugman and colleagues published a study looking at pediatric combined care at MedStar.6
“One of the things that was striking: the volumes increased dramatically. The community responds very positively to having an emergency room just for kids versus one where there’s a stroke patient, a psych patient, a patient who has been arrested, then a kid next to them. Volumes increased-both inpatient and emergency room,” Krugman says. “Another big outcome that we tracked was patient satisfaction, and our patient satisfaction actually went up. That was despite our concern about having an inpatient unit next to a [noisy, chaotic] emergency room. We have noticed a significant decrease in length of stay, which can be a good thing or can be a bad thing, if they come back, but they weren’t coming back.”
According to the study by Krugman and colleagues,6 which compares numbers from a year before opening the combination unit at Franklin Square Hospital Center (2003) to a year after (2004), Part B billings from the 5.5 FTE pediatric hospitalists increased from $1,631,583 in 2003 to $2,967,715 in 2004-a result of increased volume of ED patients seen by pediatricians. The mean inpatient satisfaction score did not significantly change: 75.7 in 2003 and 79.0 in 2004. However, the mean pediatric ED score increased from 75.8 to 83.4, respectively. Mean scores of the efficiency measures on the survey increased significantly for pediatric ED patients, with the mean score for wait time to treatment increasing from 62.0 to 75.3. Total throughput time through the ED improved from 143 minutes to 122 minutes.
“I think that we have such a well-run efficient unit that it doesn’t matter what quality measure you look at, we’ll be able to succeed in doing it,” Krugman says. “It’s the same staff doing the same thing. We’re right there talking to each other. We haven’t really tracked turnaround times, from time to admission, but in general it’s pretty darn quick because you just look across the hall and give someone sign-out.”
Michael R. Clemmens, MDAnne Arundel Health System in Annapolis, Maryland, opened its combined unit in April 2011. Michael R. Clemmens, MD, director of pediatrics, Anne Arundel Health System, says the hospital’s previous inpatient pediatric unit was a drain on the bottom line.
“There are relatively few pediatric inpatient admissions in most community hospitals. However, the standards of care have evolved to include having a pediatrician in house 24/7,” Clemmens says. “With a relatively low census, that becomes a difficult concept to support financially. Most inpatient programs require a significant financial subsidy from the hospital.”
The driving force, however, was a desire to improve the emergency medicine experience for children. “We wanted to give them their own place-away from adults having heart attacks or strokes. We wanted to staff it with doctors, nurses, and technicians that were specially trained to take care of kids,” Clemmens says.
A pediatric ED with a volume of 18,000 to 20,000 visits a year will come very close to breaking even or it might be in the black, according to Clemmens.
Key considerations
The model works best when accomplished in cooperation with and supported by adult emergency medicine colleagues, according to Clemmens.
“A positive, strong working relationship between the director of pediatrics and the director of emergency medicine is a must,” Clemmens says. “Our emergency medicine partners were concerned that we were going to take 20% of their volume away. They, in fact, were able to become more efficient and reduce wait times, and their volumes then grew about 20%. So, it was a win-win.”
Pediatricians who staff these combined units need inpatient and ED experience. The 11 pediatricians who staff Anne Arundel’s combined pediatric unit underwent additional training, according to Clemmens.
“We started as inpatient hospitalists. We developed a 1-year educational program, where we gained further training in minor trauma and in pediatric critical care. We used that with didactic sessions, workshops, and conferences,” Clemmens says. “We brought guest speakers in to lecture us on critical care topics and minor trauma. We had suture workshops, orthopedic workshops, and extensive simulation training for pediatric critical care and code situations.”
The pediatrician’s role in the combined pediatric unit is a new and emerging role, Sparrow says. “We don’t call ourselves hospitalists because this is a different model. We call ourselves pediatric attendings because we’re both ED doctors and inpatient physicians,” Sparrow says.
Community pediatricians wanting to transition to the combined unit setting will need additional training, Sparrow points out. “Most of the people who come into these positions are pediatricians just out of residency, or they’ve done hospitalist work and some ED moonlighting and come into the combined care,” she says.
The role is attractive for pediatricians, Sparrow says, because it allows for a more integrated approach to illness. “When you are emergently ill, you’re seen in the ED by 1 set of doctors. Then, you’re admitted and go to another set of doctors,” she says. “This [new concept] rejoins acute illness and convalescence in a way that I find intellectually [stimulating]. I could never go back. I want to see patients when they come in. I want to diagnose them, and I want to take care of them when they’re hospitalized.”
Nurses on the unit also need training in ED and inpatient pediatric care. At GBMC, nurses go through a 6-week orientation on both the ED side and the inpatient side.
Proven design
The model calls for the pediatric inpatient and ED units to be in the same location, according to Clemmens. Ideally, that location should be adjacent to or near the adult ED, he says.
“We designed our combined unit with parallel hallways. We have 8 emergency beds in 1 hallway. Then, there’s a central nursing corridor and nursing station. Then, there is a parallel hallway with 8 inpatient beds,” Clemmens says. One of the challenges to the design is that the inpatient unit is not as quiet as a traditional inpatient unit, he notes.
MedStar initially designed its combination unit as circular but changed it to 2 parallel halls. “[Parallel halls are] a more efficient design,” Krugman says.
Other important elements, according to Sparrow, include a playroom, a separate children’s waiting area, and separate triage. “Think about everything before you build it,” she says.
Lessons learned
Sparrow says GBMC’s combined unit has flaws. The biggest is the pediatric combined unit doesn’t see minor trauma because the adult ED negotiated to maintain that subset of patients. Minor trauma is where the summer volume and money are, Sparrow says.
“Adult EDs are going to be territorial and won’t want to give up their kids,” Sparrow says. “You have to fight for it and show them that they’ll still maintain their volumes. We made a deal where the adult ED doctors were allowed to hang onto minor trauma. That was a mistake.”
Researchers reported in May 2008 that, according to 2005 data, 6 of the top 10 reasons for children’s ED visits were for injuries such as bruises, open wounds, sprains and strains, broken arms, and other injuries from external causes.7
Monroe recommends pediatricians negotiating for these units insist on taking all levels of pediatric acute care. “That’s the only way that you’re really going to get to excellence,” Sparrow says.
MedStar conquered the potential turf problem between the adult and pediatric EDs, according to Krugman. “We have a good relationship with our adult ED group. They see patients in our ED every day. So they have a shift to see pediatric patients, to keep up their pediatric skills, and actually do a better job because they’re not competing with adult care,” Krugman says.
One of the most important things GBMC’s pediatric staff members have done right has been keeping open and regular communication with local pediatricians. The connection between pediatricians staffing the combined units and community pediatricians is critical for this model to work, Sparrow says.
“Every patient [that] we see in the ED, we write a summary of the ED visit and fax it to the doctor’s office. All patients we discharge from inpatient, we fax the doctor the summary and call to make sure they’ve received the fax. We really focus on closing that [communication] loop. I think that is what has been very appreciated by the community,” Sparrow says.
The model is a work in progress, experienced pediatricians say. For example, it can be a struggle for community hospitals to get good specialty care, according to Monroe.
“Thankfully, we’re in the Hopkins network, so we can get subspecialty care, but it’s almost always at the main hospital,” Monroe says. “So, that’s where we’re working . . . to get more care that’s appropriate in the community, to come to the community.”
Not for every community hospital
While the combined model is enticing to pediatricians and patients in the community, it’s not viable for every community hospital, according to Monroe.
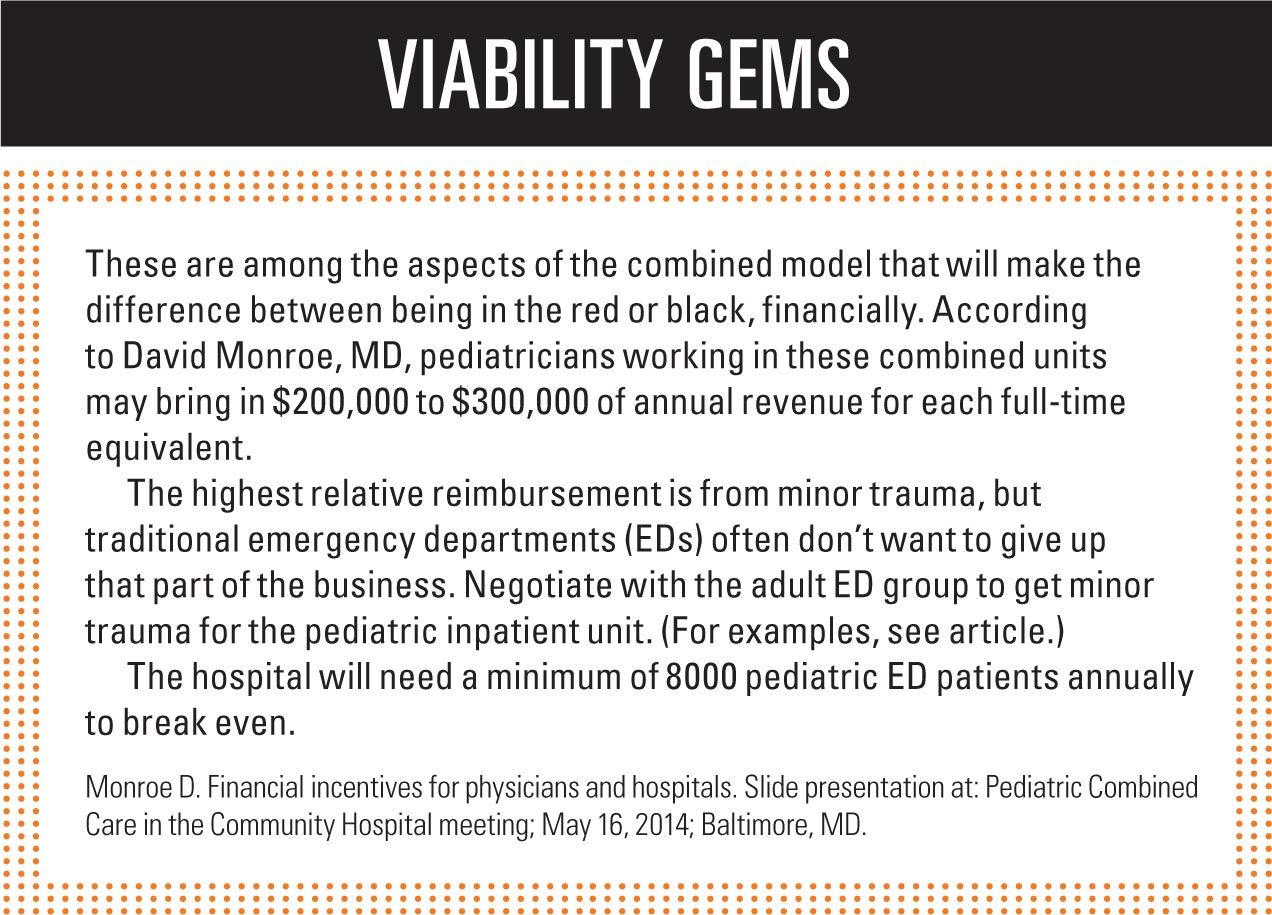
Community hospitals that do not make good fits for the model, he says, include those at which pediatric ED volumes are too low. Hospitals need to see at least 8000 pediatric ED patients annually to break even. Minor trauma is the bread and butter of these combined units, according to Monroe. Without it, community hospitals might not want to venture into this model, he says.
Hospitals with nearby tertiary care centers might not be good candidates for the model, Monroe adds.
The model also isn’t meant for academic centers, which have the pediatric volume to maintain separate inpatient units. Also, these hospitals are usually major trauma centers and their EDs need to be run by pediatric emergency medicine-trained physicians, according to Sparrow.
When it is appropriate, however, the combined pediatric unit can elevate pediatric care at the community level, Sparrow says. “What was once a suboptimal pediatric ward with a few patients here and there [can] become a Center of Excellence.”
REFERENCES
1. Dudas RA, Monroe D, McColligan Borger M. Community pediatric hospitalists providing care in the emergency department: an analysis of physician productivity and financial performance. Pediatr Emerg Care. 2011;27(11):1099-1103.
2. Krugman S. Combined care model and measurable outcomes. Slide presentation at: Pediatric Combined Care in the Community Hospital meeting; May 16, 2014; Baltimore, MD.
3. Cox KS, Teasley SL, Lacey SR, Carroll CA, Sexton KA. Work environment perceptions of pediatric nurses. J Pediatr Nurs. 2007;22(1):9-14.
4. Schappert SM, Bhuiya F. Availability of pediatric services and equipment in emergency departments: United States, 2006. Natl Health Stat Report. 2012;(47):1-21.
5. Gausche-Hill M, Schmitz C, Lewis RJ. Pediatric preparedness of US emergency departments: a 2003 survey. Pediatrics. 2007;120(6):1229-1237.
6. Krugman SD, Suggs A, Photowala HY, Beck A. Redefining the community pediatric hospitalist: the combined pediatric ED/inpatient unit. Pediatr Emerg Care. 2007;23(1):33-37.
7. Merrill CT, Owens PL, Stocks C. Pediatric emergency department visits in community hospitals from selected states, 2005. Healthcare Cost and Utilization Project (HCUP) Statistical Brief #52. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at: http://www.ncbi.nlm.nih.gov/books/NBK56039/. Published May 2008. Accessed August 13, 2014.
Ms Hilton is a medical writer who has covered health and medicine for 25 years. She resides in Boca Raton, Florida. She has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.
Study: Child heat-related illness ED visits up 170% in past decade
September 28th 2024“The significant rise in heat-related illnesses over the past decade underscores a growing public health concern that warrants further attention and action, said Taylor Merritt, MD, of the data presented at the AAP National Conference & Exhibition.














