Pediatric oral health: Fluoride use recommendations
The second part of this article on integrating oral health into primary pediatric care discusses the important role of fluoride and fluoride varnish application for preventing dental caries in children.
Figures 1-4
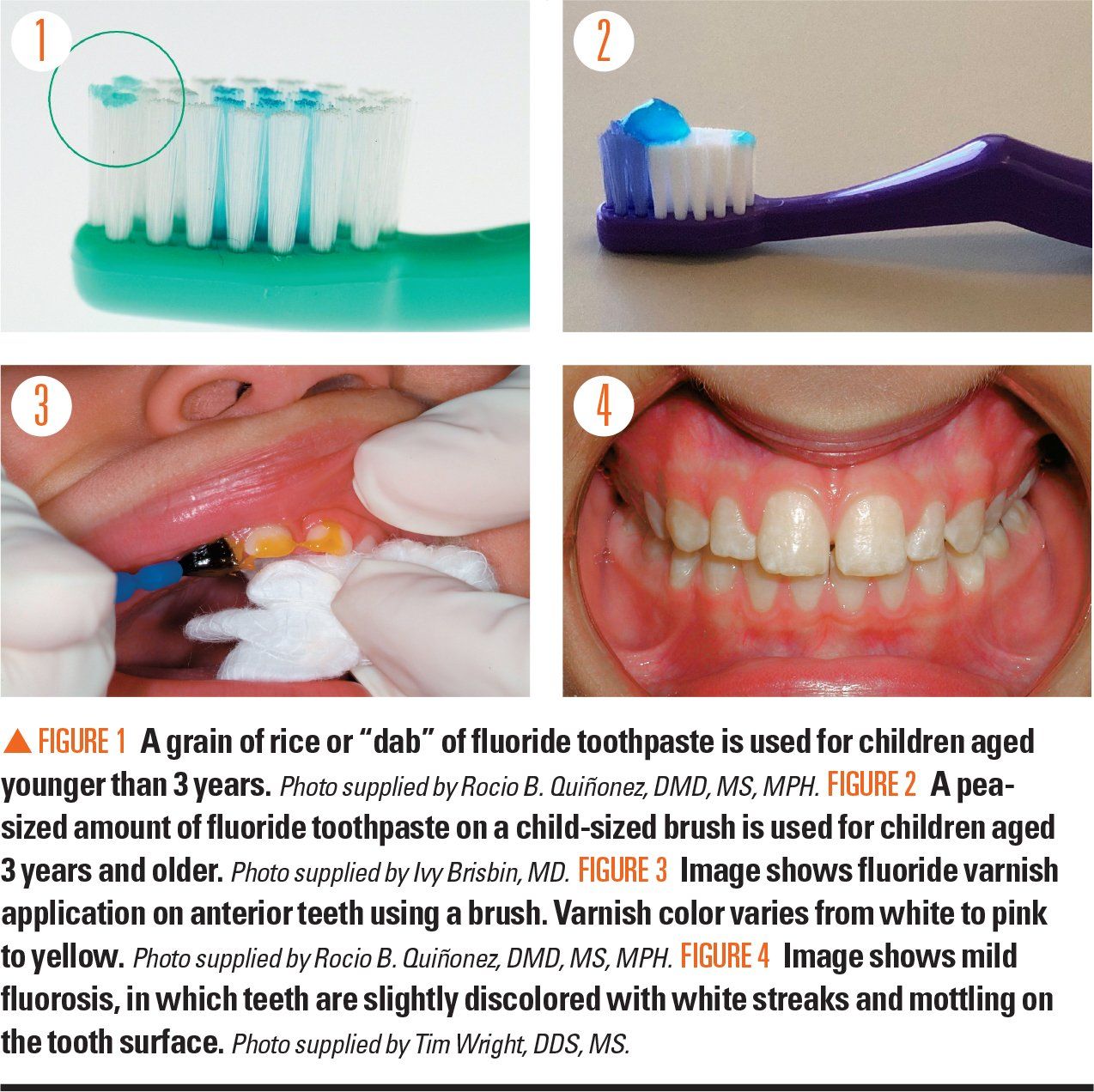
Table 1
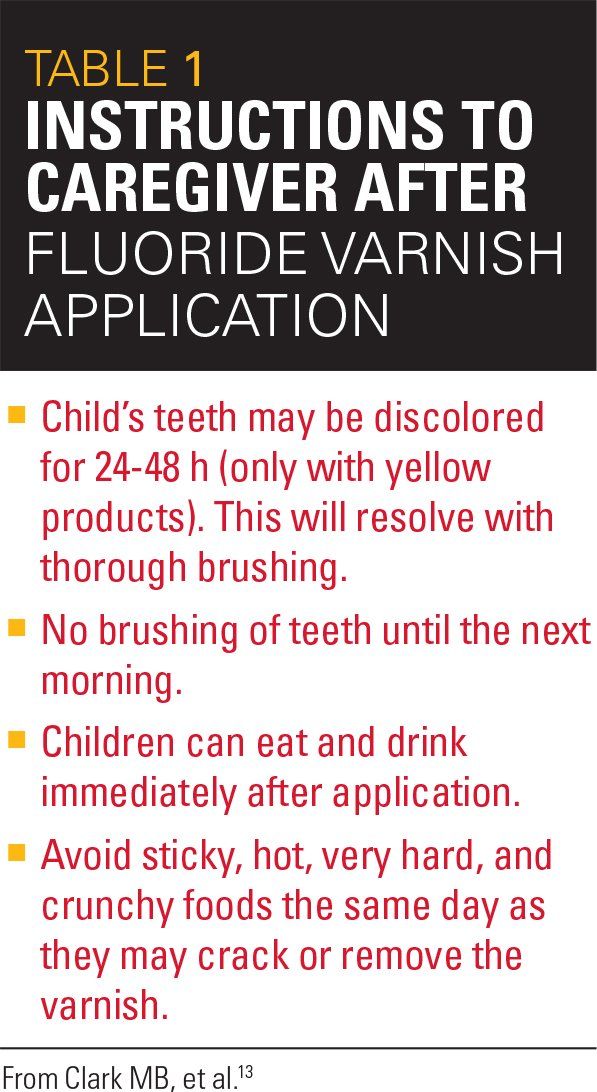
Table 2
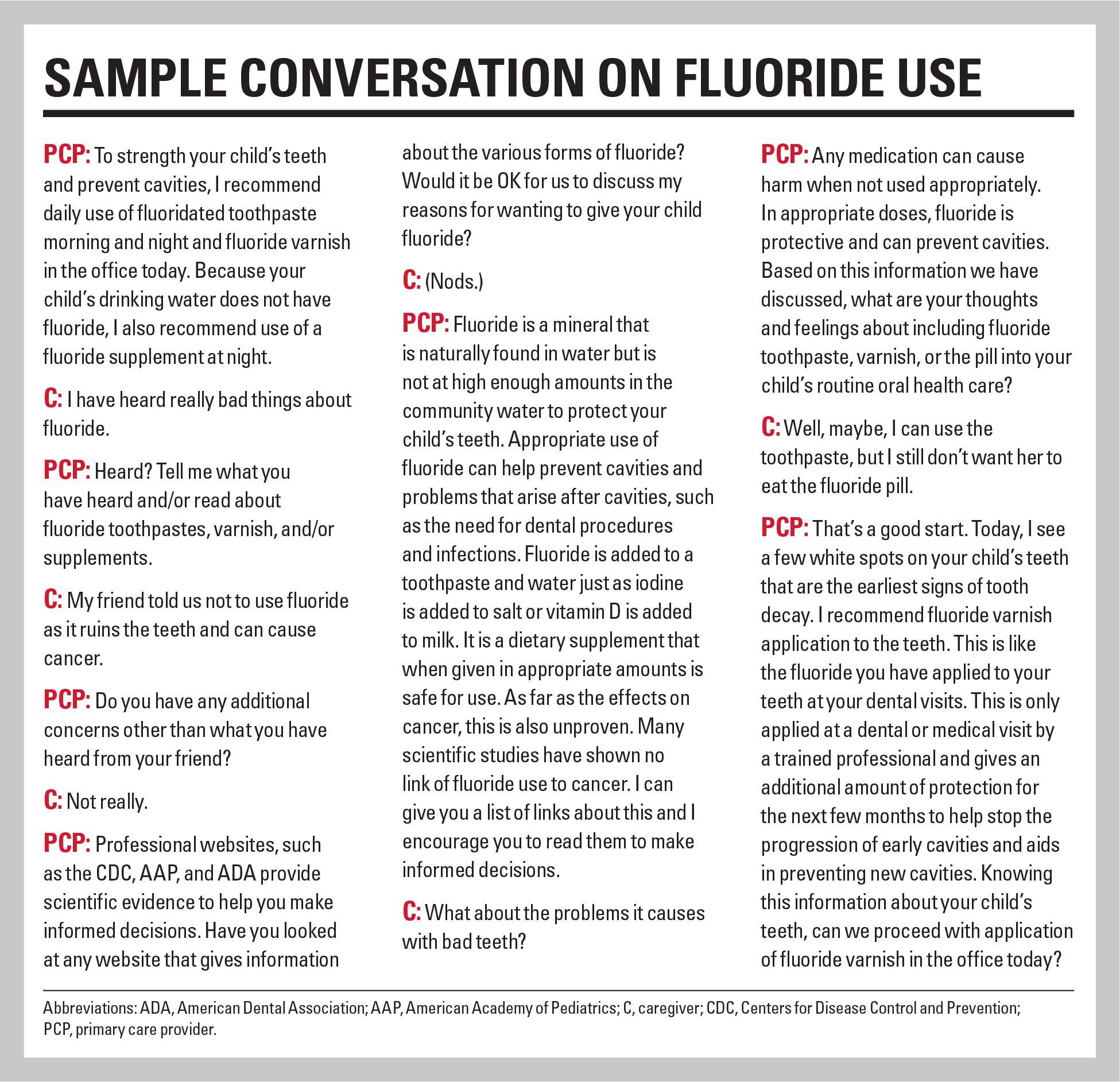
Sample conversation on fluoride use
Dental caries (cavities) continues to be the most chronic disease of childhood.1 Although dental caries is multifactorial in its etiology, fluoride is an important chemotherapeutic intervention to strengthen teeth and prevent disease progression.2 The safety of fluoride has been demonstrated in numerous research studies and community water fluoridation heralded as one of the top 10 public health achievements of the 20th century by the Centers for Disease Control and Prevention (CDC).3
How fluoride prevents dental caries
Fluoride works to prevent dental caries through both topical and systemic mechanisms via 3 processes: inhibiting tooth demineralization, enhancing remineralization, and inhibiting bacterial metabolism. Newer studies also suggest that fluoride interferes with bacterial adherence to the teeth.4 The topical effect provides the majority of the benefit. Through systemic mechanisms, the lesser effect, fluoride is incorporated into the tooth structure during tooth development to harden the enamel and make more resistant to demineralization.
What type of fluoride is recommended
Topical fluoride in the form of toothpaste (at-home use) and varnish (in-office use) should be recommended for all children starting at tooth eruption.2,5 The American Academy of Pediatrics (AAP) and United States Preventive Services Task Force (USPSTF) also recommends dietary fluoride supplements for all children who do not have an adequate supply of fluoride in their primary drinking water. The AAP additionally recommends fluoride mouth rinse use for children aged 6 years and older who are at high risk for dental caries.2,6
TOPICAL FLUORIDE
Toothpaste: Fluoridated toothpaste is recommended upon initial tooth emergence during infancy and throughout life.7,8 Do not recommend fluoride-free “training toothpaste.”
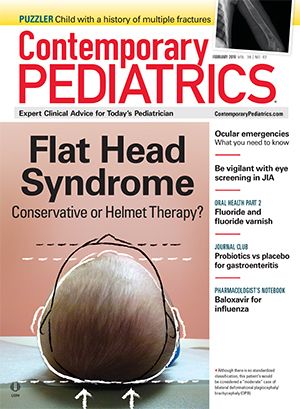
1. From tooth emergence until age 3 years, a grain of rice-sized (or “dab”) amount of fluoride toothpaste should be used to brush the teeth both morning and night (Figure 1).
2. For children aged older than 3 years, or when a child can effectively spit, a pea-sized amount of fluoride toothpaste should be applied morning and night (Figure 2).
Children should be encouraged to spit after brushing. Post-brushing rinsing with water should be limited to provide optimal fluoride exposure to the teeth from the toothpaste.2,9 Fluoride toothpaste, like all other medications, should be kept out of reach of small children.
Mouth rinses: Over-the-counter fluoride rinses may be beneficial for use for children, particularly those who have high caries risk or live in fluoride-deficient areas. Mouth rinses should be reserved for high-risk children aged older than 6 years who can rinse and spit.2,10 Alcohol-containing mouth rinses should be avoided in pediatric populations.9 Fluoride mouth rinses, supplements, or gels can be used after brushing with fluoride toothpaste.
Varnish: Fluoride varnish is a highly concentrated form of topical fluoride that is applied to teeth in a professionally supervised setting. Research shows fluoride varnish is highly effective in caries reduction with a decrease in caries incidence between 18% to 24% in 1 study and as high as 59% in another.11,12 The USPSTF “recommends that primary care clinicians apply fluoride varnish to the primary teeth of all infants and children starting at the age of primary tooth eruption” through age 5 years.6 The recommended fluoride varnish dose is 0.25 mL unidose 5% NaF (2.26% F), and frequency is every 3 to 6 months, based on the child’s caries risk considerations.2,13 Fluoride varnish application is easy and fast. A thin layer should be placed on relatively dry teeth achieved by wiping the teeth with gauze.
The steps in fluoride application are:13
1. Assemble a light source, gauze, and varnish.
2. Use gauze to blot the teeth dry. Varnish does not adhere well to teeth if they are wet.
3. Prepare for application by stirring the varnish and apply varnish to dried teeth, starting on the back teeth. Apply a thin layer to all tooth surfaces with the supplied brush.
4. Apply varnish to the front teeth last. Saliva contamination after application is expected and varnish sets on contact with saliva (Figure 3).
5. Provide caregiver instructions about varnish application after care (Table 1).13
Instructional videos of proper fluoride varnish application technique can be viewed online in the National Smiles for Life Curriculum Module 613: www.smilesforlifeoralhealth.com.
Fluoride varnish application is a safe14,15 and effective16 procedure now reimbursed by Medicaid in all 50 states and by private insurers in many states.13 In some states, not only physicians and advanced practitioners but also nurses and medical assistants can apply the varnish. In many states, trained individuals are available to instruct pediatric office personnel on fluoride varnish application. The AAP has a designated Chapter Oral Health Advocate in most states who can educate individuals and offices on fluoride varnish application or provide support as questions arise about oral health integration into practice.17
Developing a clinical workflow to include fluoride varnish application can improve the oral health of children within a practice. A recent Qualis Health White Paper offers specific strategies for integration of oral health into practice workflow.18
Other forms of topical fluoride:
Dental providers may recommend other forms of topical fluoride, including highly concentrated fluoride gels. However, these are generally not recommended for young children aged younger than 6 years. In addition, silver diamine fluoride is a modality now being used in dentistry to help arrest caries in primary teeth.19,20
Community water fluoridation:
Lastly, fluoridated community water aids in prevention of dental caries by up to 27%21 and reduces dental expenditures per capita22 by providing both topical and systemic routes of fluoride. Fluoridated tap water use should be encouraged instead of bottled water use, which may not contain fluoride and may be more acidic than previously anticipated, thus promoting demineralization of tooth structure.23 Parents who live in areas with fluoridated water should be asked if their child drinks fluoridated water. Parents often use bottled water and therefore their children may not be receiving the benefits of fluoridated water. Pediatric medical and dental providers should continue to strongly advocate for community water fluoridation as it benefits not only children, but the entire population.24
SYSTEMIC FLUORIDE
The AAP recommends systemic (dietary) fluoride supplementation in children aged 6 months to 16 years who live in areas where the primary water supply is fluoride deficient. It is important to ask about sources of fluoride in a child’s diet, such as fluoride in well water, and the fluoridation status of the local communities. Fluoride levels for well water should be determined before prescription of fluoride dietary supplements, as wells in some locations may exceed the recommended fluoride levels. For town water, the state Department of Health or the CDC’s My Water’s Fluoride website are good resources to determine fluoridated amounts in the water supply throughout individual states.
Systemic fluoride is usually prescribed by a medical or dental provider and comes in 2 forms, a liquid or a tablet. The liquid, most often used for young children aged younger than 3 years or whose primary molars are either not present or emerging, can be mixed with a small amount of water or applied into the mouth directly onto the teeth. In older children, the tablet is used and is available in 3 dosages: 0.25 mg fluoride, 0.5 mg fluoride, and 1 mg fluoride2 (Table 2). The tablet should be chewed or allowed to dissolve in the mouth for optimal exposure of the teeth to fluoride. Both the liquid and supplement should not be given within 1 hour of milk products as calcium binds fluoride and inhibits its absorption.25
Challenges
Inconsistencies remain in dietary fluoride prescribing guidelines among national organizations. The AAP and USPSTF recommend use of fluoride supplements for all children living in fluoride-deficient areas, whereas the American Academy of Pediatric Dentistry (AAPD) and the American Dental Association (ADA) recommend dietary fluoride supplementation only for children determined to be at high caries risk who drink fluoride-deficient water. Discrepancies in messaging between the medical and dental communities present a clinical challenge for primary care providers and underscores the value of a collaborative relationship between primary care and the local pediatric dental provider. Some primary care providers choose to let dental providers develop the plan of fluoride use once a child has established a dental home.
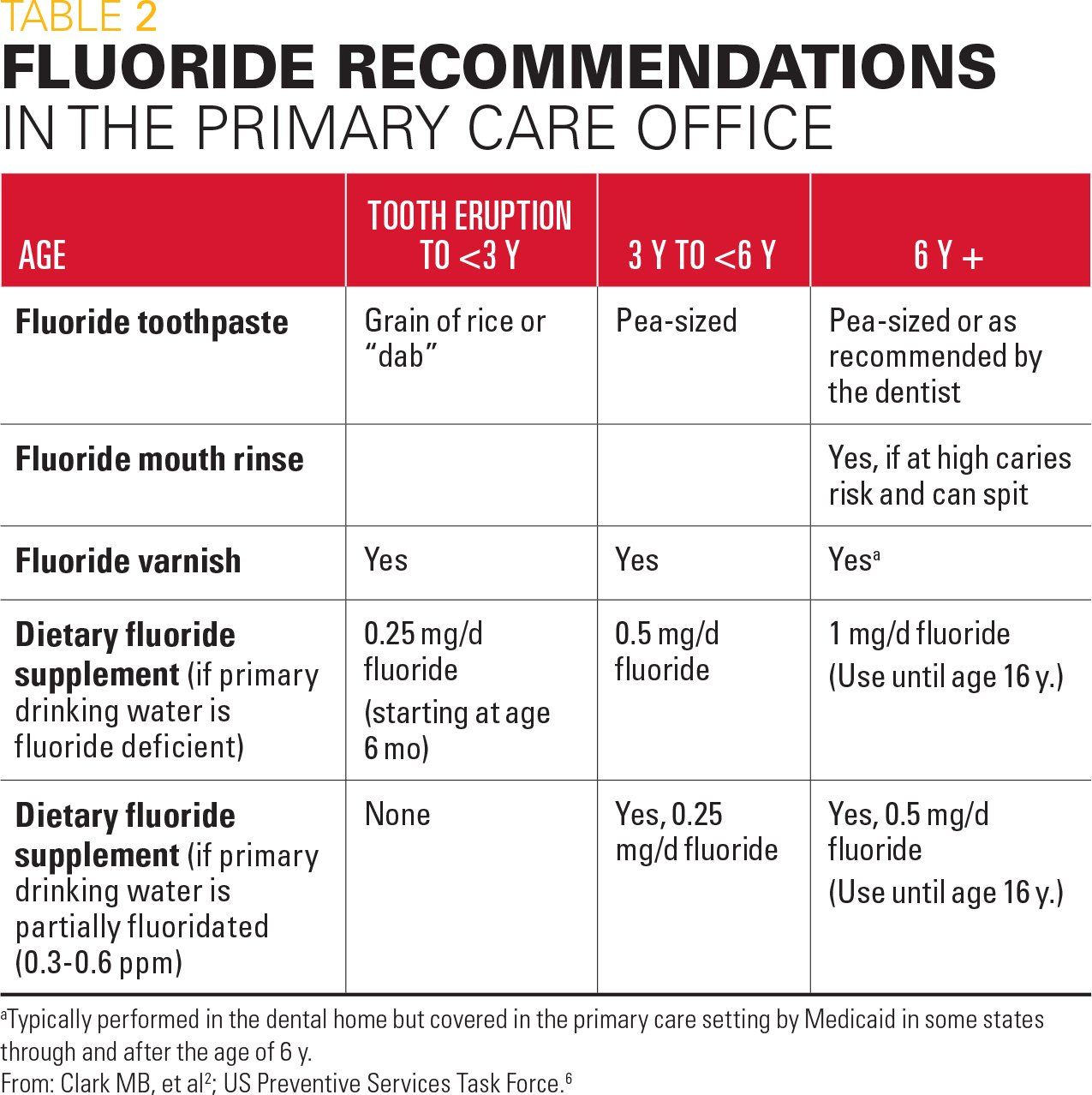
The fear of fluorosis has fueled some concerns about fluoride use. Fluorosis occurs when developing teeth are exposed to high quantities of fluoride. Fluorosis presents as white streaks or mottling on the tooth surface (Figure 4), with the milder presentations typically not noticeable except by a trained dental professional.26 The risk of fluorosis increases when fluoride is not used appropriately, such as eating large amounts of fluoride toothpaste during unsupervised brushing, or prescribing fluoride to a child who already is drinking fluoridated water. Recommend that caregivers always supervise young children during tooth brushing and keep toothpaste in a safe location out of reach of young children, just like other medications in the home.
Many other fears, such as fluoride causing cancer or a low IQ, do not have a basis in scientific evidence. A good AAP website to refer to patients to help address these myths is ilikemyteeth.org. It is important to understand concerns regarding fluoride and seize the opportunity to use motivational interviewing beginning with open-ended questions that promote dialogue, such as: “What have you heard about fluoride?” or “Help me understand your concerns about fluoride use.”
There may be times when you have given the family all the facts and they may continue to refuse fluoride. In these situations, it is best to make certain the patient has early and consistent dental care to continue the discussion. Consistent messaging from the primary care provider and dental specialists may help allay fears and encourage families to use fluoride.
Three strategies to consider are:
1. Reassure-Use language such as: “Fluoride is safe to use in appropriate amounts.”
2. Refer-Provide information from credible websites such as ilikemyteeth.org. Recommend early establishment of a dental home to help deliver consistent messages about fluoride use.
3. Renegotiate-Consider alternate fluoride usage routes if needed. Typical caregiver concerns about fluoride safety relate to ingestion of the product. As topical fluoride is the most beneficial, encourage compromise with use of limited fluoride in toothpaste, varnish, or mouth-rinse form.
Motivational interviewing is an exemplar for integration of oral health in primary care to address caregiver worries and encourage ongoing discussion (see “Sample conversation on fluoride use”).
Take-home message for pediatricians
To summarize, fluoride continues to be essential in caries prevention. Both topical and systemic fluoride play a role in maintaining good teeth and preventing oral disease, but the topical effects are foremost. Primary care providers should be aware of the appropriate fluoride modalities to advise for children at each age and whether that recommendation is universal or based on caries risk.
A well-informed pediatric provider can address concerns raised by fluoride-hesitant families through motivational interviewing and personalized communication. Early referral to establish a dental home may help provide clarity about fluoride use and improve dental health. Consistent messaging from the medical and dental communities about oral health and fluoride use will promote optimal dental and overall health.
References:
1. Dye BA, Tan S, Smith V, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;(248):1-92.
2. Clark MB, Slayton RL; Section on Oral Health. Fluoride use in caries prevention in the primary care setting. Pediatrics. 2014;134(3):626-633.
3. US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Executive summary. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. Available at: https://www.nidcr.nih.gov/research/data-statistics/surgeon-general. Reviewed January 2019. Accessed January 22, 2019.
4. Loskill P, Zeitz C, Grandthyll S, et al. Reduced adhesion of oral bacteria on hydroxyapatite by fluoride treatment. Langmuir. 2013;29 (18):5528–5533.
5. Weyant RJ, Tracy SL, Anselmo T, et al; American Dental Association Council on Scientific Affairs Expert Panel on Topical Fluoride Caries Preventive Agents. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc. 2013;144(11):1279-1291.
6. US Preventive Services Task Force. Dental caries in children from birth through age 5 years: screening. Recommendation summary. Rockville, MD: US Preventive Services Task Force; 2014. Available at: www.uspreventiveservicestaskforce.org/uspstf/uspsdnch.htm. Accessed January 22, 2019.
7. Dos Santos AP, Nadanovsky P, de Oliveira BH. A systematic review and meta-analysis of the effects of fluoride toothpastes on the prevention of dental caries in the primary dentition of preschool children. Community Dent Oral Epidemiol. 2013;41(1):1-12.
8. American Dental Association Council on Scientific Affairs. Fluoride toothpaste use for young children. J Am Dent Assoc. 2014;145(2):190-191. Erratum in: J Am Dent Assoc. 2014;145(3):236.
9. American Academy of Pediatric Dentistry. Guideline on fluoride therapy. Pediatr Dent. 2013;35(5):e165-e168.
10. Faller RV, Casey K, Amburgey J. Anticaries potential of commercial fluoride rinses as determined by fluoridation and remineralization efficiency. J Clin Dent. 2011;22(2):29-35.
11. Lawrence HP, Binguis D, Douglas J, et al. A 2-year community-randomized controlled trial of fluoride varnish to prevent early childhood caries in Aboriginal children. Community Dent Oral Epidemiol. 2008;36(6):503-516.
12. Weintraub JA, Ramos-Gomez F, Jue B, et al. Fluoride varnish efficacy in preventing early childhood caries. J Dent Res. 2006;85(2):172-176.
13. Clark MB, Douglass AB, Maier R, et al. Smiles for Life: A National Oral Health Curriculum. 3rd ed. Society of Teachers of Family Medicine. 2010. Available at: www.smilesforlifeoralhealth.com. Accessed January 22, 2019.
14. Beltrán-Aguilar ED, Goldstein JW, Lockwood SA. Fluoride varnishes: a review of their clinical use, cariostatic mechanism, efficacy and safety. J Am Dent Assoc. 2000;131(5): 589-596.
15. Garcia RI, Gregorich SE, Ramos-Gomez F, et al. Absence of fluoride varnish–related adverse events in caries prevention trials in young children, United States. Prev Chronic Dis. 2017;14:e17.
16. Pahel BT, Rozier RG, Stearns,SC, Quiñonez RB. Effectiveness of preventive dental treatments by physicians for young Medicaid enrollees. Pediatrics. 2011;127(3):e682-e689.
17. American Academy of Pediatrics. State information and resources map. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Oral-Health/Pages/State-Information-and-Resources-Map.aspx. Accessed January 22, 2019.
18. Hummel J, Phillips KE, Holt B, Hayes C. Oral Health: An Essential Component of Primary Care. Seattle, WA: Qualis Health; June 2015. Available at:
http://www.niioh.org/sites/default/files/Oral_Health_white_paper_final.pdf. Accessed January 22, 2019.
19. Fung MHT, Duangthip D, Wong MCM, Lo ECM, Chu CH. Randomized clinical trial of 12% and 38% silver diamine fluoride treatment. J Dent Res. 2018;97(2):171-178.
20. Crystal YO, Marghalani AA, Ureles SD, et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017;39(5):135-145. Available at: http://www.aapd.org/media/Policies_Guidelines/G_SDF.pdf. Accessed January 22, 2019.
21. Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. J Dent Res. 2007:86(5);410-415. Available at: http://www.ncbi.nlm.nih.gov/pubmed/17452559. Accessed January 22, 2019.
22. Ran T, Chattopadhyay SK; Community Preventive Services Task Force, Economic evaluation of community water fluoridation: a community guide systematic review. Am J Prev Med. 2016;50(6):790-796.
23. Wright KF. Is your drinking water acidic? A comparison of the varied pH of popular bottled waters. J Dent Hyg. 2015;89(suppl 2):6-12.
24. Centers for Disease Control and Prevention. Community water fluoridation. Available at: https://www.cdc.gov/fluoridation/index.html. Reviewed October 4, 2016. Accessed January 22, 2019.
25. Buzalaf MA, Whitford GM. Fluoride metabolism. Monogr Oral Sci. 2011;22:20-36.
26. Pendrys DG. Risk of enamel fluorosis in nonfluoridated and optimally fluoridated populations: considerations for the dental professional. J Am Dent Assoc. 2000;131(6):746-755.