Prevent medical errors in your practice
Diagnostic and medication errors frequently occur in pediatric practices, but even minor medical errors can be prevented by creating a culture of safety.
Figure 1
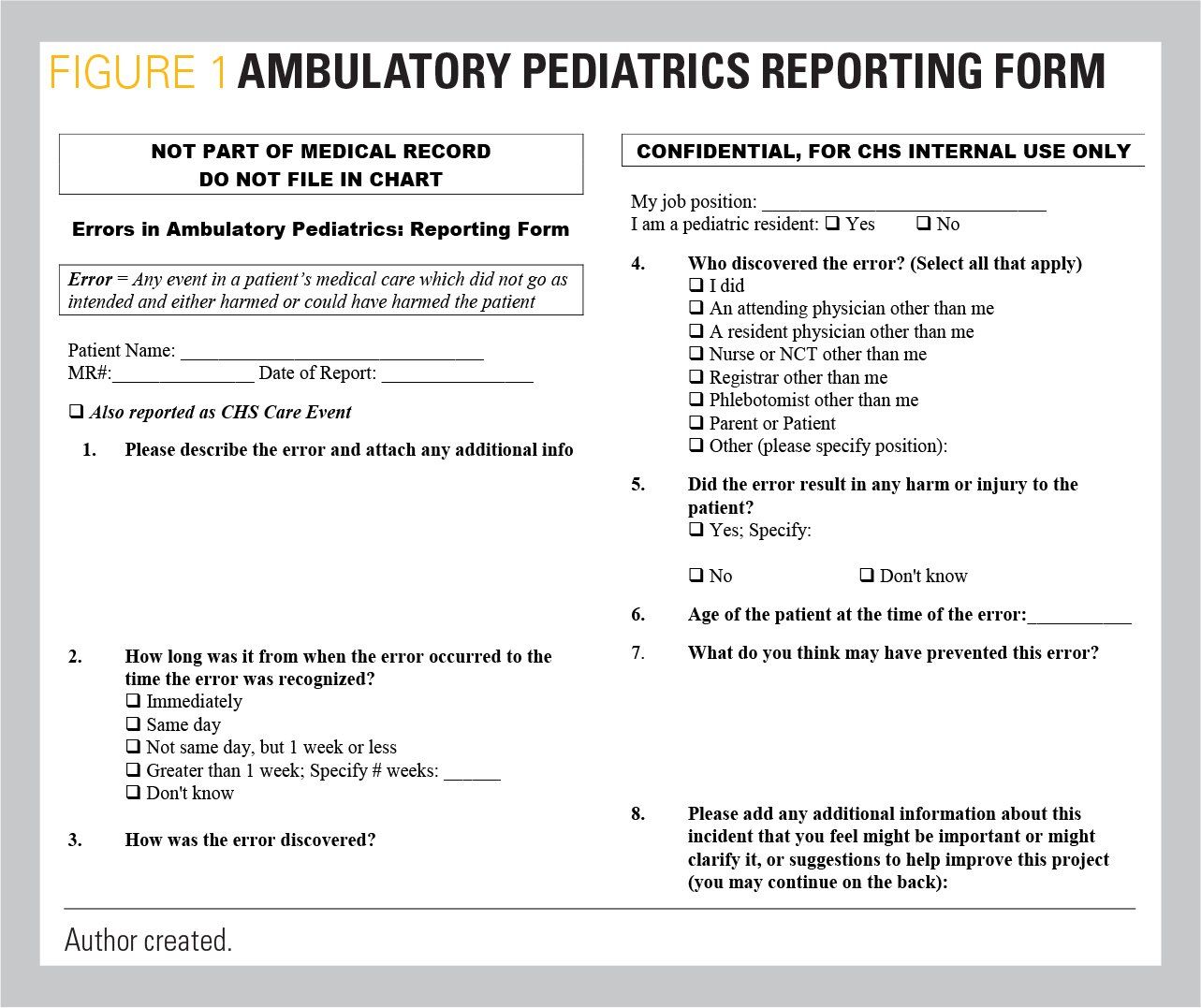
Table 1
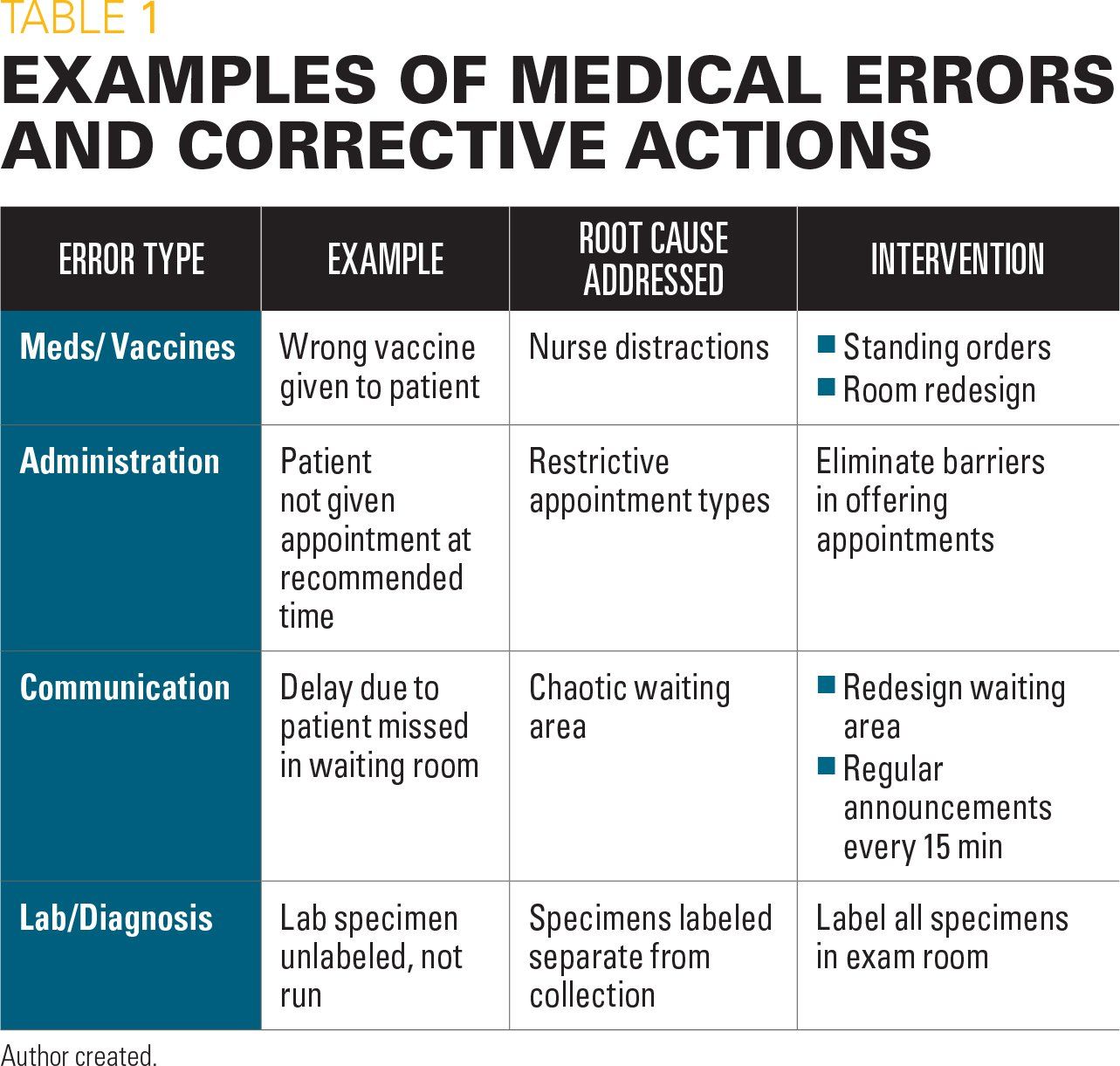
Figure 2
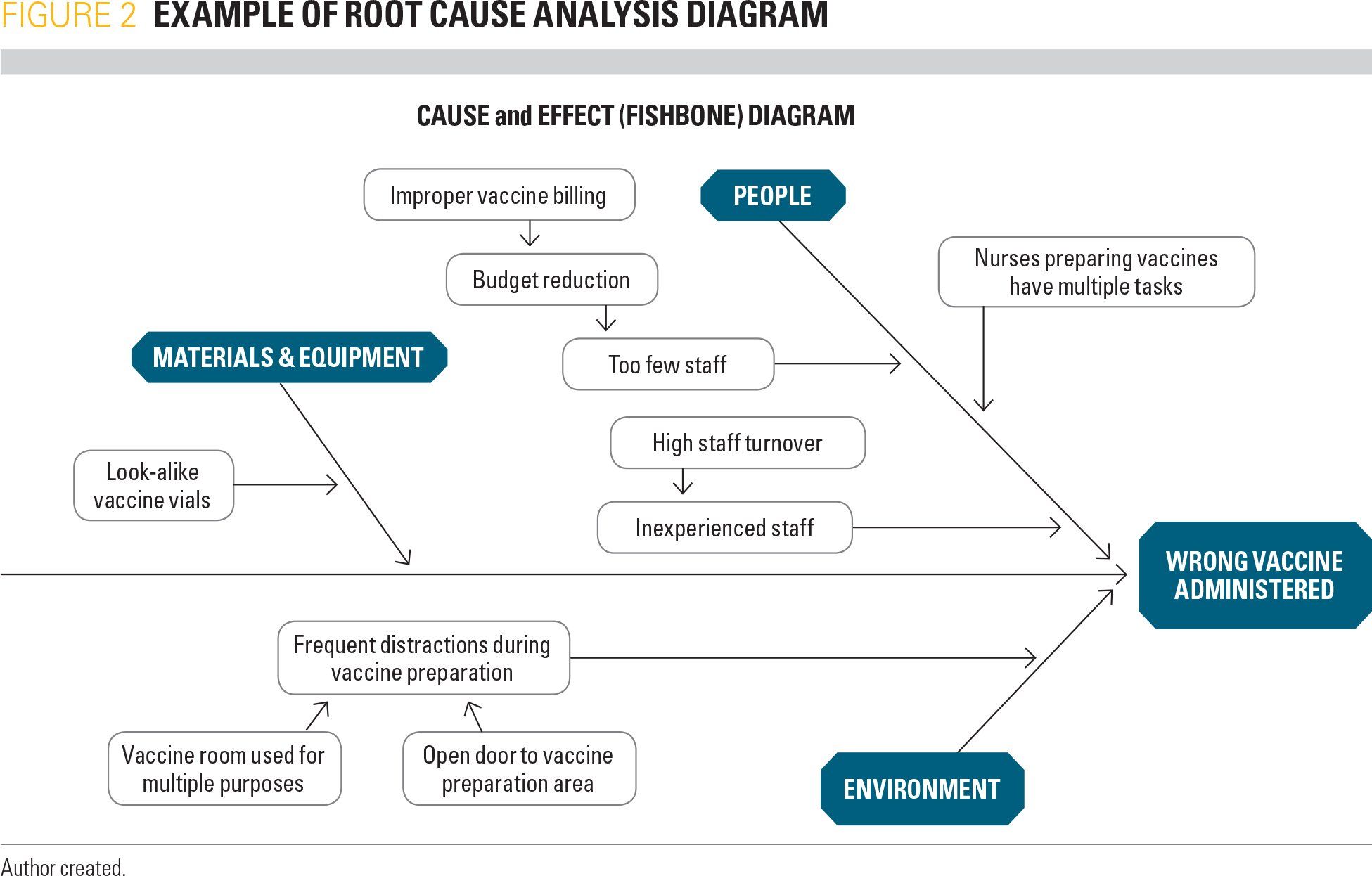
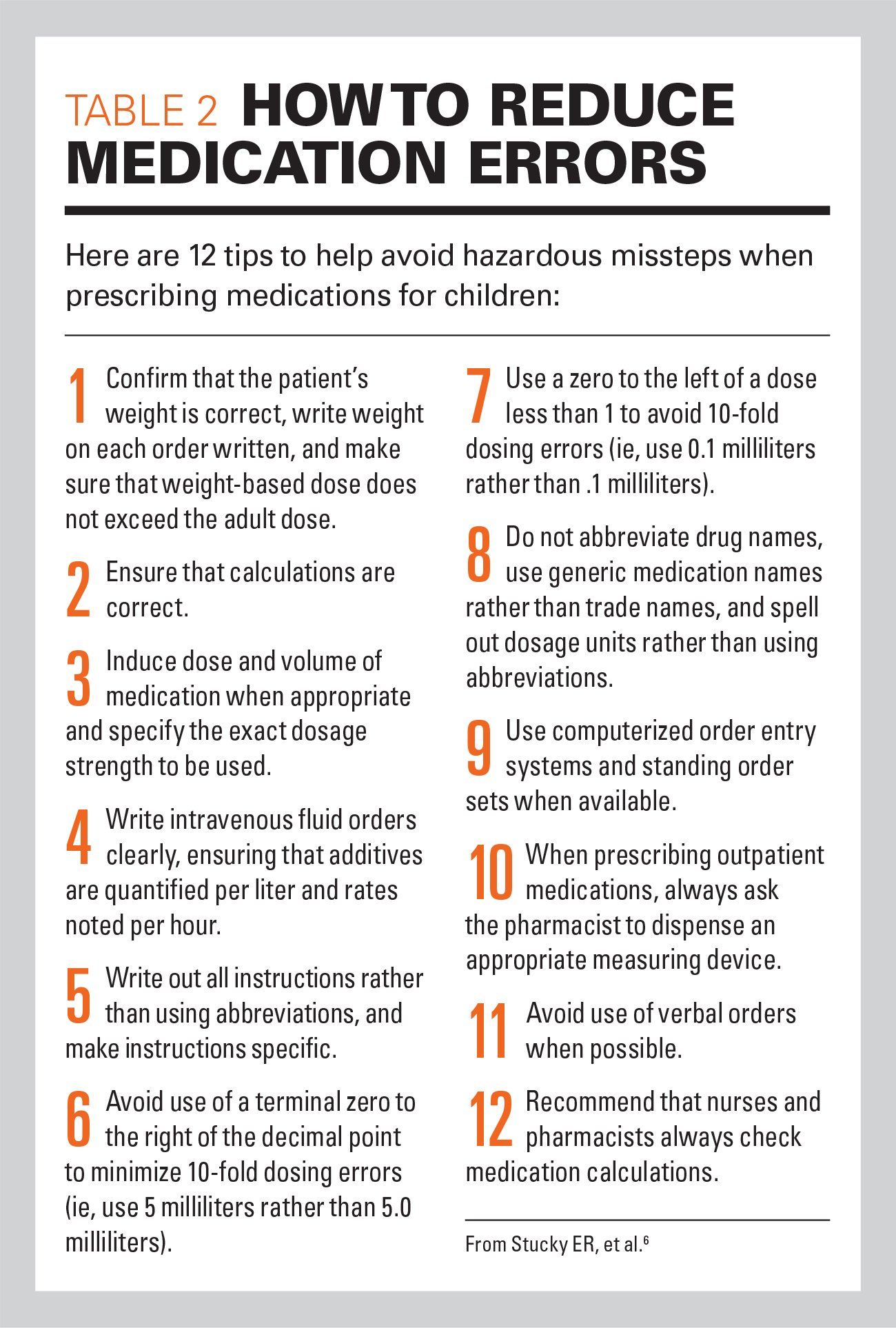
Table 2
It is important for pediatricians to be aware that medical errors are frequent occurrences in pediatric practice. To safeguard our patients, we must implement an effective system to identify errors, as well as develop a strategy to prevent them.
The Institute of Medicine (IOM, now known as the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine) published the monograph To Err is Human in 1999, alerting the medical community that medical errors were common in medical practice. According to the IOM report, “at least 44,000 people and perhaps as many as 98,000 people die in hospitals each year as a result of medical errors that could have been prevented.”
The monograph described and detailed the types of errors seen in the hospital environment. These included:
1. Diagnostic errors resulting from a failure to employ indicated tests or failure to act on the results of such tests.
2. Treatment errors in the performance of a procedure or administering of a treatment including medications, or inappropriate care.
3. Preventive errors, including failure to provide prophylactic treatment or inadequate follow-up to treatment.
The IOM report indicated that effective reporting systems needed to be implemented in healthcare facilities in order to reduce medical errors.1
Magnitude of the problem
Whereas errors are common in the inpatient setting, the number of pediatric hospitalizations pales in comparison with the number of pediatric ambulatory visits each year. In 2015, the Agency for Healthcare Research and Quality (AHRQ) reported 5.6 million pediatric hospitalizations in the United States, while the Centers for Disease Control and Prevention (CDC) reported 125 million ambulatory pediatric visits that year.
The 2003 Learning from Errors in Ambulatory Pediatrics (LEAP) study conducted by the AHRQ and the American Academy of Pediatrics (AAP) Pediatric Research in Office Setting Network produced interesting data relating to the incidence of errors occurring in the ambulatory pediatric setting. In the 4-month data collection period from 14 sites, 136 errors were identified. Error types were: 37% medical treatment, 22% patient identification, 15% preventive care, 13% diagnostic testing, and 8% patient communication.2
Practice-based safety team
One of the authors of this article, Daniel Neuspiel, MD, initiated a quality improvement project in 2008 for Myers Park Pediatrics, an affiliate of the Levine Children’s Hospital of Carolinas Medical Center in Charlotte, North Carolina. The project established a safety team that included front office staff, medical providers, nursing staff, and administrative personnel. The team developed a nonpunitive reporting system to identify errors in need of evaluation, using the reporting form in Figure 1. The team met monthly to review reports of errors, and recommended interventions that would prevent future errors.
Errors were defined as “any event in the patient’s care which did not go as intended with either potential or real harm.” Over a 30-month period from 2008 to 2010, 216 errors were reported. These included errors in office administration (94); communication (40); medication or immunizations (45); and lab or diagnostic testing (37).3 The team used a problem-solving system called root cause analysis to look at the potential causes of the errors. The analysis technique utilizes a cause-and-effect diagram to identify problems and propose solutions (Figure 2). Examples of common ambulatory pediatric practice errors along with solutions are shown in Table 1.
Medical errors in pediatric practice
Children are at higher risk than many adults for medical errors because they have medical dosages based on weight, limited ability to communicate symptoms when young, and often their care is fragmented, provided by not only their primary care physicians, but by varying caregivers, specialists, and providers that are seen in walk-in clinics and emergency departments.
According to the Physician Insurers Association of America, from 2003 to 2012, errors in diagnosis accounted for 828 closed pediatric cases with an average indemnity of $414,455; medication errors accounted for 113 closed cases with an average indemnity of $207,916.
The most frequent medical error type in pediatric practice is the diagnostic error. Children are at higher risk for diagnostic errors due to the difficulty in eliciting their symptoms, particularly in infants and toddlers. Another frequent source of error is medication administration, especially home medication use. Children are at particular risk due to mistakes in measurement of liquid medications, multiple caregivers responsible for medication administration, adolescents who are self-medicating without adult supervision, and other factors.
Reducing diagnostic errors
Diagnostic errors are problematic in that solutions may require radical changes in our healthcare system. According to the National Academies’ monograph Improving Diagnosis in Health Care,” solutions may include more reliance on clinical decision support tools, utilizing teamwork more effectively, and improving healthcare education to sharpen diagnostic acumen.4 The monograph further suggested we develop a nationwide reporting and liability system that supports the diagnostic process and design a payment and care delivery model that encourages, rather than delays, patient visits.
Reducing medication errors
According to a systematic review, as many as 10% of all pediatric medication orders result in a medication error.5 This topic was reviewed by author Andrew Schuman, MD, in the October 2017 issue of Contemporary Pediatrics (see “Safety first: How to avoid missteps when prescribing medications,” October 2017, page 38).
Providers can take a variety of steps to avoid prescribing errors (Table 2).6 We can distribute dosing charts to parents for over-the-counter medication and reinforce their use with verbal instructions. Providers must confirm the patient’s weight prior to writing a prescription and make sure the weight-based dose does not exceed the adult dose. In addition, prescriptions must indicate the exact dosage strength and the volume of medication to administer. Other measures that can reduce errors are using pediatric computerized order entry systems and standing order sets when available, and having an appropriate measuring device dispensed along with the medication. Having caregivers explain back to you how they will administer the medication (teach-back) and show you how they will measure it (show-back) are two techniques that have been helpful in reducing these errors.
Reduce other errors
There are a variety of common errors, other than diagnostic and medical errors, in medical practice that have been identified. Treating the wrong patient error is reduced by using 2 identifiers to confirm that the correct patient is being treated. Time-outs are appropriate means to reduce errors in the surgical suite. In the practice environment, electronic health records (EHRs) are often a cause of error as it is an easy matter to write the wrong note on the wrong patient and subsequently generate incorrect prescriptions. This common error can be avoided (but not eliminated) when providers take the time to confirm-twice-that they are in the correct record before writing prescriptions or documenting a visit. To make sure patients understand your recommendations, it is always a good idea to provide written instructions and have parents repeat instructions to you.
Build a culture of safety
The Myers Park Pediatric Error Reduction Project, described above, created a safety model that will work in most ambulatory pediatric settings. One needs to acknowledge that errors are frequent occurrences in pediatric practices. However, errors can be reduced and prevented by creating a multidisciplinary safety team.
Nonpunitive reporting improves the detection of even minor errors. The team meets regularly to review reporting forms, discuss errors, and develop solutions that are tested. If successful, these processes become office policy, but if unsuccessful they are reevaluated.
By implementing these few measures, you will create a safer environment for your practice and your patients and cultivate a “culture of safety.”
References:
1. Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000.
2. Mohr JJ, Lannon CM, Thoma KA, et al. Learning from errors in ambulatory pediatrics. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation (Vol 1: Research Findings). Rockville MD: Agency for Healthcare Research and Quality; 2005:355-368.
3. Neuspiel DR, Stubbs EH, Liggin L. Improving reporting of outpatient pediatric medical errors, Pediatrics. 2011;128(6):e1608-e1613.
4. National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: National Academies Press; 2015.
5. Rinke ML, Bundy DG, Velasquez CA, et al. Interventions to reduce pediatric medication errors: a systematic review. Pediatrics. 2014;134(2):338-360.
6. Stucky ER; American Academy of Pediatrics Committee on Drugs; American Academy of Pediatrics Committee on Hospital Care. Prevention of medication errors in the pediatric inpatient setting. Pediatrics. 2003;112(2):431-436.
Anger hurts your team’s performance and health, and yours too
October 25th 2024Anger in health care affects both patients and professionals with rising violence and negative health outcomes, but understanding its triggers and applying de-escalation techniques can help manage this pervasive issue.