The pros and cons of imaging options
Knowing the benefits and limitations of computed tomography, magnetic resonance imaging, and other techniques can help you request the right studies, prepare the family for the exam, and evaluate results.
The pros and cons of imaging options
By Anne Paterson, MRCP, Lane F. Donnelly, MD, and Donald P. Frush, MD
What is the best imaging choice for a particular situation? Knowing the benefits and limitations of computed tomography, magnetic resonance imaging, and other techniques can help you request appropriate studies, prepare the family for the examination, and evaluate the results.
Advances in diagnostic imaging have greatly improved our ability to diagnose and treat pediatric illness. To decide which of a variety of contemporary imaging techniques is the best choice in a particular situation, the pediatrician must know the advantages and disadvantages of each. Familiarity with the major imaging techniques also enables the primary care provider to address the parents' or child's questions about the procedure, including any necessary examination preparations such as fasting. It also enhances an understanding of the significance and limitations of imaging results. Finally, requesting the best imaging modality potentially increases diagnostic yield and reduces the need for additional imaging. In discussing imaging options we will focus on those for parts of the body other than the central nervous system. Table 1 summarizes the salient features of the imaging techniques discussed here.
TABLE 1
Choosing the right technique
Conventional radiography
More than 100 years after X-rays were discovered, conventional radiography, also known as "plain film" and "film screen," is still the most frequently requested imaging examination. With modern film-screen combinations, these are low-dose examinations, though no radiation dose can be considered perfectly safe.1,2 The radiation risk is minimal, however, and exposure is limited to the area being examined. Lead shielding is routinely used for the more radiosensitive areas, such as the gonads and breast tissue. Radiography is relatively inexpensive, quick (each exposure takes less than a second to perform), and readily available. It requires no patient preparation and causes no pain or discomfort.
In interpreting a radiograph, the radiologist is able to discriminate four different anatomic densities: bone (including other calcifications), soft tissue or fluid, fat, and air. Other material, such as metal, can also be detected. A differential diagnosis is based on radiologic findings, but also relies on relevant clinical and laboratory data. Radiography principally is used to investigate the skeleton (Figure 1) and chest (Figure 2) and, to a lesser extent, to screen for intra-abdominal disease.


Fluoroscopy
Fluoroscopy is an enhanced X-ray that uses an image intensifier and produces images on a television monitor. The images are in real time and, like plain film radiography, the technique is widely available. The best way to describe this technology to a parent or patient may be as an "X-ray movie." Compared with plain radiographs, the patient absorbs a higher, and sometimes substantial, dose of radiation.3 Focusing only on the structure(s) of interest and shielding other regions of the body reduces the radiation dose and shortens the procedure.
Most fluoroscopy is performed for gastrointestinal (GI) evaluation (barium swallowing, upper GI series, with or without a small bowel follow-through, barium enema) or genitourinary (GU) evaluation (cystograms and voiding urethrograms) (Figures 3 to 6). Fluoroscopy provides both anatomic and functional information. Common indications for GI evaluation include nonspecific GI symptoms and constipation. For some upper GI studies, placement of a small feeding tube may be necessary, particularly if the infant or very young child will not drink. Easily placed, minimally and only transiently painful or uncomfortable, the tube has an extremely low risk of complications.




Most GU investigations are in patients with a history of urinary tract infection, in whom vesicoureteric reflux needs to be excluded. The cystogram requires placement of a catheter within the bladder, which can be painful. In some children it may be useful to administer an anxiolytic before the cystogram. Though using such agents is not routine, they do not seem to affect results. Two recent studies found no statistical differences in results of cystography in children who did and did not receive an anxiolytic.4,5 The pediatrician who thinks sedatives may be a good idea should discuss the matter with the radiologist and the child's parents before scheduling the examination.
Other minimally invasive procedures using fluoroscopy include therapeutic enemas in suspected meconium ileus, joint aspirations (often better achieved using sonographic guidance), hydrostatic or air reduction of intussusception, and removal of esophageal coins. Fluoroscopy costs about four to 16 times as much as radiography.
Sonography
In sonography, high-frequency sound waves are bounced off parts of the body, and the returning echoes are captured as images. Sonography uses sound with a frequency from 2.0 to more than 10 MHz, greater than the audible range. The transducer transmits sound and receives "echoes" so rapidly that the reconstructed images appear to be in real time. The acoustic properties of the tissue or organ being imaged determine the nature of the image. This is why the brain in newborns, the liver, the kidneys, or fluid-containing structures (such as the gallbladder or urinary bladder) look different in terms of echotexture. The time it takes for the pulse to be received determines the tissue's location. Sonography is portable and widely available. It has no harmful effects, causes no pain, and requires no sedation. The patient requires little preparation, except for gallbladder exams, when the child should fast, and pelvic studies, usually best done with a full bladder. Since sound is scattered by air and is reflected by dense structures, evaluation of lungs and bone marrow is limited.
For an optimal sonographic evaluation, the technologist must be skilled. Examinations typically cost about six times as much as radiography.
When enhanced with a technique based on the Doppler effect, sonography can depict flowing blood. The Doppler effect is a perceived change in the frequency of a sound emitted by a moving source. In medical imaging, the moving sources are red blood cells. Using the Doppler technique, the patency and flow characteristics of arteries and veins can be assessed, and the vascular supply of normal structures and pathologic processes (such as neoplasms) can be demonstrated (Figure 7). The arbitrary assignment of color to this frequency shift within vessels is called color Doppler. "Spectral" Doppler is a graphic waveform depiction of the velocity and intensity of the Doppler signals. When color and spectral Doppler are combined, the result is called duplex Doppler sonography. Power Doppler is a technique that depends only on the amplitude (or power) of the signal and is independent of the velocity and direction of flow. This technique is most sensitive to slower blood flow and flow in small or remote vessels.

Sonography can readily evaluate many common pediatric problems. It is most often used to assess renal and neonatal intracranial pathology (Figure 8). Suspected hepatobiliary disease and abdominal or pelvic processes are also indications for sonographic examinations (Figure 9). Musculoskeletal indications include hip effusions and developmental dysplasia of the hip in infants. Sonography also is used to evaluate scrotal disorders and abnormalities in the neck, including those of the thyroid gland.


Computed tomography
Computed tomography (CT) consists of many low-dose X-rays taken in sequence by a rotating X-ray tube. A computer reconstructs these views to make a single diagnostic image. CT scans are either "conventional" (slice-by-slice images) or "helical" (also called spiral). Helical scans are rapidly replacing slice-by-slice examinations. Current technology provides for faster scans and a volumetric data set, where multiple planes and three-dimensional reconstructions provide additional anatomic information (Figure 10). CT is excellent for depicting anatomical detail. CT images are less affected by operator variability than sonographic images are. CT examinations are performed rapidly, usually taking less than 30 seconds. Compared with magnetic resonance (MR) imaging, discussed below, this translates to less reliance on sedation, especially in children younger than 4 years, who are more likely to need sedation, and easier scheduling. Nonetheless, examinations take about 30 to 45 minutes because of the necessary preparations for scanning, such as getting the child properly positioned, discussing the examination with the child and parent, and allowing turnaround time for the next CT examination. The use of IV contrast material makes possible examination of organ enhancement (for example in the liver and kidneys) and direct visualization of the vessels. IV contrast media are usually necessary for abdominal and pelvic scans, improving the detection and characterization of abnormalities.6 Contrast agents are generally not required for chest scanning if the examination is intended solely to evaluate lung parenchyma, but are frequently used to assess the mediastinum.

CT delivers a higher dose of radiation than conventional radiography, one of this technology's disadvantages. In addition, CT may require sedation and IV access, if IV contrast material is used. Abdominal and pelvic scans are often performed with oral contrast media. The oral solution is either dilute barium or a water-soluble iodinated agent mixed with a beverage, such as juice or soda. The taste is still perceptibly unpleasant, and young children have more difficulty drinking this material than older children do. Oral contrast is not a requirement for scanning and depends on the radiologist's preference and the clinical indications for the scan.7 In general, the radiologist decides whether oral or IV contrast material needs to be given. This decision, which is important to convey to parents, is based on the indication for scanning. CT examinations are about two and one-half times as expensive as sonographic examinations.
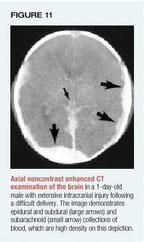
CT is particularly useful for diagnosing and monitoring cancer, for evaluating intracranial (Figure 11), abdominal, and chest trauma, for evaluating infection (Figure 12), and as a screening evaluation of nonspecific clinical symptoms, such as fever of unknown origin. CT also supplements assessment of chest parenchymal disorders and mediastinal abnormalities, which are not adequately defined with chest radiography.

Magnetic resonance imaging
MR imaging produces detailed pictures of organs and tissues. The patient is placed in a strong magnetic field, which causes the atoms within the body that have magnetic moment (those with a greater number of protons than neutrons in the nucleus) to align themselves while a radio frequency pulse is applied to upset the formation. The "echo" of these atoms, as they realign and give off energy (or signal), allows for the reconstruction of an image by an advanced computer system. In diagnostic MR, the signal from aligned hydrogen ions is used to form the image. This reconstruction results only after many pulses and echoes. The timing, length, and type of radiofrequency pulses can be varied to distinguish among different tissues (contrast resolution). Excellent contrast resolution is a major benefit of MR imaging. Physiologic information is also possible with dynamic enhancement patterns. The potential for multiplanar and three-dimensional evaluation is another benefit of this modality. IV contrast material is not commonly required for imaging of the abdomen and pelvis as it is with most CT scans of these regions.
MR images are obtained without ionizing radiation. The examinations are not painful, though the noise of the scanner can be disturbing. The scan time of an individual MR sequence ranges from less than a minute to up to 15 minutes. A complete MR exam comprises several sequences and lasts from 30 to 60 minutes. Unlike in CT or sonography, a single image cannot usually be obtained, as image reconstruction is complete only when the entire sequence is finished. Sedation is often necessary in children under 7 years, as even small movements can significantly degrade image quality in the sequence. Since the child is within the bore of the magnet and cannot be seen well, he or she must be monitored, using MRcompatible equipment, for oxygenation (pulse oximetry) and pulse rate, as well as respiratory excursion and rate. Claustrophobia is much less of a problem in children than in adults.
MR imaging can cost up to twice as much as CT examination. It cannot be used in patients with certain electronic devices, such as cardiac pacemakers and cochlear implants. The presence of metal, for example vascular clips, can significantly degrade image quality.
MR imaging most often is used for the central nervous system (Figure 13). In the remainder of the body, it is predominantly for musculoskeletal evaluation (Figure 14), including trauma, tumors, and marrow disorders. Other indications include cancer evaluation and surveillance and some cardiac and vascular evaluation. Because the lungs do not contain enough protons to generate signal, CT is preferred for pulmonary parenchymal evaluation.


Both oral and IV contrast media are available for MR imaging. These agents are used less often than CT, however. IV contrast material is used most often in CNS imaging. Occasionally, abdominal or musculoskeletal examinations (such as cancer evaluation) may benefit from administration of an MR contrast agent. When IV contrast media are used, the effect is similar to that produced by CT scanning with IV contrast.
Contrast agents
In children, IV contrast media most often are used in CT. The contrast agents contain iodine in a non-ionic, low osmolar solution. Although these contrast media do cause reactions in up to 8.5% of children if late reactions are taken into account, the reactions tend to be fewer and less severe than those that result from high osmolar drugs.8 The child who previously had a severe adverse reaction to iodinated contrast is at highest risk. For such a child, using a steroid preparation or changing to another imaging modality may be the best course. IV contrast material also often causes flushing or warmth and a metallic taste. Patients and parents can best deal with these sensations, which last only seconds to minutes, if they are discussed just before the exam.
Gadolinium (Gd), chelated to diethylenetriaminepenta-acetic acid (DTPA), is used as an IV contrast agent in MR imaging. There are no absolute contraindications for Gd-DTPA. A study of 655 patients revealed a 1.7% incidence of minor reactions to Gd-DTPA, none of which required treatment.9
A few contrast agents are available for use in Doppler sonography to improve the Doppler signal. In the United States, approved agents are used solely for echocardiography, though noncardiac applications are expected.
The contrast medium used in GI and GU examinations, except for intravenous urogram studies, is either water soluble or a barium solution, given directly into the organ system to be evaluated. Water-soluble contrast medium is preferred when perforation is suspected. Barium sulfate generally is used in the GI tract. Its high density improves image quality, and it can be combined with air or carbon dioxide (double-contrast technique) to delineate mucosal detail. Aspirated barium is relatively harmless. Leakage into the peritoneal cavity or mediastinum can cause peritonitis or granulomatous mediastinitis, however. Cystography and urethrography are routinely performed with a water-soluble, iodine-containing solution.
Nuclear medicine
Nuclear medicine shows the shape, structure, and function of organs, soft tissues, and bones. It uses a radiopharmaceutical, a minute quantity of a drug to which a radionuclide is tagged, for delivery to specific organs, bones, or tissues. Once in position, the radionuclide emits gamma radiation, which is detected by a scintillation camera. Once again, computer software reconstructs the image in this technique. Radiopharmaceuticals rarely cause adverse reactions, and the images obtained demonstrate both physiologic events and limited anatomic detail.10 Studies commonly used in children may be dynamic, relating to regional perfusion, gastroesophageal or vesicoureteric reflux, or gastric emptying. Alternatively, static images may be obtained to study specific cellular localization or tracer adsorption, such as with a bone scan for evaluation of bone infection, fractures, or metastases (Figure 15). Other than the indications mentioned above, scintigraphy is also useful in children for primary tumor evaluations, such as in lymphoma and neuroblastoma. Most scans produce two-dimensional (planar) images. Single- photon emission computerized tomography (SPECT) studies yield multiplanar images.

The isotopes are ingested or, more commonly, given intravenously. SPECT, or whole body imaging, often takes a long time, and children younger than 4 years may need to be sedated. Nuclear medicine exams nearly always deliver a lower radiation dose than fluoroscopy or CT. For example, the dose used in nuclear cystography may be as little as 1/100th of conventional fluoroscopic cystography.11 Nuclear examinations provide limited anatomic information compared with radiography/ fluoroscopy, sonography, and CT and MR imaging.
Positron emission tomography (PET) is becoming more widely available than it was in the past. The most commonly used isotopes, all given IV, are short-lived and require on-site or regional production in a cyclotron, though express delivery from remote locations is making the isotopes available more routinely. The equipment is expensive and the radiation dose is higher than with other nuclear medicine examinations. Examinations typically last up to an hour, and sedation is often required for infants and young children. Typical indications in children are limited primarily to evaluation of metastatic disease (Figure 16) and seizure disorders.

Making the right choice
Pediatricians should be familiar with the variety of imaging options for children, indications for their use, and their benefits and limitations. Armed with this information, the physician is better able to request the appropriate study, prepare the child and family for the examination, and understand the significance and limitations of the results.
REFERENCES
1. Chu WK, Sangster W, Dobry CA: Comparison of radiation exposures between conventional and rare-earth screen/film systems. Health Phys 1985;49:958
2. Russell JGB: How dangerous are diagnostic X-rays? Clin Radiol 1984;35:347
3. West M: The principles of dose limitation and the various means of dose reduction to the patient, including protection of the gonads, in Wootton R (ed): Radiation Protection of Patients. New York, Cambridge University Press, 1993, pp 5865
4. Elder JS, Longenecker R: Premedication with oral midazolam for voiding cystourethrography in children. AJR 1995;164:1229
5. Bozkurt P, Kiliq N, Kaya G, et al: The effects of intranasal midazolam on urodynamic studies in children. Br J Urol 1996;78:282
6. Frush DIP, Donnelly LF: Helical CT in children: Technical considerations and body applications. Radiology 1998;209:37
7. Donnelly LF: Oral contrast medium administration for abdominal CT: Reevaluating the benefits and disadvantages in the pediatric patient. Pediatr Radiol 1997;27:770
8. Cohen MD: A review of the toxicity of nonionic contrast agents in children. Invest Radiol 1993;28:S87
9. Ge H-L, Hirsch WL, Wolf GL, et al: Diagnostic role of gadolinium: DTPA in pediatric neuroradiology. Neuroradiology 1992;34:122
10. Silberstein EB, Ryan J, the Pharmacopeia Committee of the Society of Nuclear Medicine: Prevalence of adverse reactions in nuclear medicine. J Nuc Med 1996;37:185
11. Treves St, Gelfand M, Willi UW: Vesicoureteric reflux and radionuclear cystography, in Willi U, Treves ST (eds): Pediatric Nuclear Medicine, ed 2. New York, Springer Verlag, 1985, pp 411430
DR. PATERSON is Consultant, Paediatric Radiologist, Royal Belfast Hospital for Sick Children, Belfast, Northern Ireland.
DR. DONNELLY is Associate Professor of Radiology, Children's Hospital Medical Center, Cincinnati, Ohio.
DR. FRUSH is Associate Professor of Radiology, Duke University Medical Center, Durham, N.C.
Donald Frush, Lane Donnelly. The pros and cons of imaging options. Contemporary Pediatrics 2001;4:73.
Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.