- Consultant for Pediatricians Vol 3 No 7
- Volume 3
- Issue 7
Swimmer's Itch
A 6-year-old girl and an 11-year-old boy each presented for evaluation of an erythematous, pruritic, papular rash that developed after swimming in a Wisconsin lake.
A 6-year-old girl (A) and an 11-year-old boy (B) each presented for evaluation of an erythematous, pruritic, papular rash that developed after swimming in a Wisconsin lake. Each child was otherwise completely healthy.
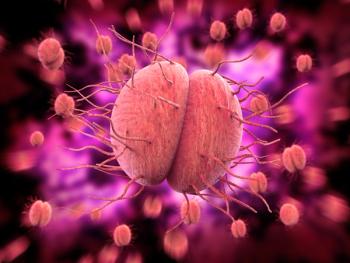
Both children have cercarial dermatitis, commonly known as swimmer's itch. This is a hypersensitivity reaction that occurs after exposure to schistosome larvae in freshwater lakes. Schistosome eggs (of trematodes, genera Schistosoma and Trichobilharzia) are passed into freshwater lakes via bird feces. The eggs hatch and develop into the larval stage called miracidia, which infect their intermediate host, freshwater mollusks. The miracidia transform into a second larval form called cercaria, which leave the mollusks and infect birds either by being ingested or penetrating their skin. Cercaria can also penetrate human skin and may infect persons swimming in infested water. The cercaria are unable to complete their life cycle in humans and die in the epidermis.
Although most common in the Great Lakes region of the United States, outbreaks occur during the summer months throughout the world. As the skin dries and the cercaria penetrate the epidermis, patients often describe the initial itching sensation. Small macules may be visible transiently at the site of penetration. Several days to 2 weeks after initial exposure, a mild to moderately pruritic, erythematous, papular, sometimes pustular eruption develops on any skin that had been exposed to infested water. In sensitized persons, the eruption develops within hours of exposure. The onset and intensity of the eruption correspond to the degree of sensitization. The rash peaks within 48 to 72 hours and usually resolves within 1 week.
Treatment is supportive and consists of oral and topical antihistamines and topical corticosteroids. Anthelmintic therapy is not indicated for this self-limited condition.
Preventive measures include avoiding exposure to fresh water that contains mollusks and toweling off immediately after swimming (since penetration into the skin occurs during evaporation).
References:
FOR MORE INFORMATION:
* Fiorillo L, Zucker M, Sawyer D, Lin AN. The
Pseudomonas
hot-foot syndrome.
N Engl J Med.
2001;345:335-338.
* Folster-Holst R, Disko R, Rowert J, et al. Cercarial dermatitis contracted via contact with an aquarium: case report and review.
Br J Dermatol.
2001;145: 638-640.
* Freudenthal AR, Joseph PR. Seabather’s eruption.
N Engl J Med.
1993;329:542-544.
* From the Centers for Disease Control and Prevention.
Pseudomonas
dermatitis/folliculitis associated with pools and hot tubs-Colorado and Maine, 1999-2000.
JAMA.
2001;285:157-158.
* Kitamura M, Kawai S, Horio T.
Pseudomonas aeruginosa
folliculitis: a sporadic case from use of a contaminated sponge.
Br J Dermatol.
1998;139:359-360.
* Kumar S, Hlady WG, Malecki JM. Risk factors for seabather’s eruption: a prospective cohort study.
Public Health Rep.
1997;112:59-62.
* MacSween RM, Williams HC. Seabather’s eruption- a case of Caribbean itch.
BMJ.
1996;312:957-958.
* Segura-Puertas L, Ramos ME, Aramburo C, et al. One Linuche mystery solved: all 3 stages of the coronate scyphomedusa Linuche unguiculata cause seabather’s eruption.
J Am Acad Dermatol.
2001;44: 624-628.
* Swimmer’s itch. Wisconsin Department of Natural Resources. Available at:
http://dnr.wi.gov/lakes/swimmersitch/
. Accessed July 1, 2009.
Articles in this issue
over 21 years ago
Hot Tub Folliculitis in an 11-Year-Old Boyover 21 years ago
Seabather's EruptionNewsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.