Teenaged Girl With Acute Chest Pain
A previously healthy 15-year-old girl presents with right-sided chest pain that began a few hours earlier during Spanish class. The pain is nonradiating; it is alleviated by leaning forward and exacerbated by sitting still. Shortly after its onset, the patient had taken acetaminophen, which provided temporary relief. However, when she returned home from school, the pain resumed. She denies fever, shortness of breath, nausea, vomiting, and cough.

A previously healthy 15-year-old girl presents with right-sided chest pain that began a few hours earlier during Spanish class. The pain is nonradiating; it is alleviated by leaning forward and exacerbated by sitting still. Shortly after its onset, the patient had taken acetaminophen, which provided temporary relief. However, when she returned home from school, the pain resumed. She denies fever, shortness of breath, nausea, vomiting, and cough.
At 6 years of age, she had been hospitalized for Stevens-Johnson syndrome (exact cause unknown).
The patient is alert, oriented, talkative, and in no acute distress. She is slightly underweight (52 kg, 49th percentile) and tall (170 cm, 89th percentile). Temperature is 36.1ºC (96.9ºF); heart rate, 62 beats per minute; respiration rate, 20 breaths per minute; and blood pressure, 108/59 mm Hg. Oxygen saturation, measured with pulse oximetry, is 98% on room air.
The lungs are clear to auscultation bilaterally; breath sounds are slightly diminished on the right side. Head, eye, ear, nose, and throat examination findings are normal. Heart sounds are regular, without murmurs, rubs, or gallops. Abdomen is soft, nontender, and nondistended. Extremities are nonedematous. There is no rash or evidence of lymphadenopathy.
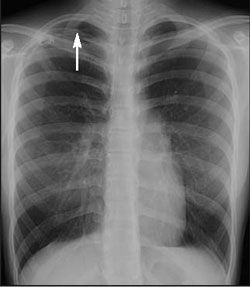
The patient's chest radiograph is shown.
What do you suspect?
(Answer and discussion on the next page)

The chest radiograph shows a moderate pneumothorax on the right (Figure 1).
The annual incidence of primary spontaneous pneumothorax is 7.4 cases per 100,000 men and 1.2 cases per 100,000 women.1 The development of primary spontaneous pneumothorax in this patient-and in adolescents in general-may be related to an ectomorphic physique or thin body habitus, which is characterized by long arms and legs and a short upper body with narrow shoulders. It is hypothesized that during the early teen years, rapid vertical growth of the thorax may affect intrathoracic pressure and promote the formation of subpleural blebs, which can then rupture spontaneously. Blebs are more likely to rupture at the apex of the lung because of the decrease in pleural pressure that occurs in this area when standing or sitting upright, as a result of gravity. Smoking and a familial pattern of inheritance have also been linked to primary spontaneous pneumothorax.2
Secondary pneumothorax is associated with preexisting lung disease, most commonly chronic obstructive pulmonary disease, and has occurred in children with cystic fibrosis and in patients with AIDS who have Pneumocystis jiroveci pneumonia.2
Symptoms, signs, and diagnosis.
Children with primary spontaneous pneumothorax may present with ipsilateral pleuritic chest pain of sudden onset, dyspnea, tachycardia, diminished breath sounds, hyperresonance, or cough.
3
Symptoms are often exacerbated when the patient is at rest.
The presence of pneumothorax is usually confirmed by plain chest radiographs. A visceral pleural line without vessel markings is a key diagnostic finding.3 Radiographs may also show hyperlucency of vascular and lung markings. Chest CT can help distinguish preexisting lung conditions, such as neoplastic disease, from spontaneous pneumothorax when the diagnosis is uncertain.2,4
Therapy. Although various approaches to the treatment of spontaneous pneumothorax may be used, the goals of therapy-to remove free air from the pleural space and prevent recurrence-remain the same.2,4 In uncomplicated cases, such as the case presented here, simple aspiration and observation are usually sufficient and effective. Therapy is guided by the patient's clinical status rather than by the size of the pneumothorax. Reexpansion edema is a potential complication of spontaneous pneumothorax and can result from delay in seeking treatment. Progressive air leakage may lead to tension pneumothorax, which is a life-threatening emergency. Chest tube placement with pleurodesis or videoassisted thoracoscopy may be indicated for patients who do not respond to initial aspiration and for those who have recurrent pneumothorax.5 In about 25% of patients, pneumothorax recurs within 2 years. The rate of recurrence also increases with each subsequent episode.3
In this patient, a pigtail catheter was used to aspirate air from the pleural cavity; serial chest radiographs performed over the following days showed gradual lung re expansion (Figure 2). She was discharged after 7 days and was scheduled for follow-up with her primary care physician.
References:
REFERENCES:
1.
Garfunkel LC, Kaczorowski J, Christy C, eds.
Pediatric Clinical Advisor: Instant Diagnosis and Treatment.
2nd ed. Philadelphia: Mosby; 2007:450-451.
2.
Baumann MH. Management of spontaneous pneumothorax.
Clin Chest Med.
2006;27:369-381.
3.
Ramberan H. Spontaneous pneumothorax. In: Ferri FF, ed.
Ferri’s Clinical Advisor: Instant Diagnosis and Treatment.
9th ed. Philadelphia: Mosby; 2007:702-703.
4.
Sahn SA, Heffer JE. Spontaneous pneumothorax.
N Engl J Med.
2000;342:868-874.
5.
Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement.
Chest.
2001;119:590-602.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.