- November/December 2023
- Volume 40
- Issue 10
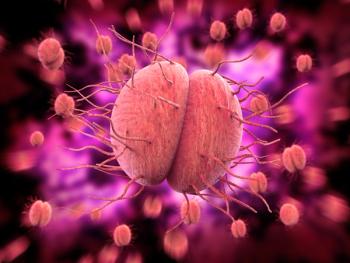
The transformative impact of HPV vaccines
At IDWeek 2023, a session on how increased rates of the HPV vaccine have resulted in a decline in certain conditions and disease states.
In her comprehensive update, "How HPV vaccination has changed HPV epidemiology and HPV-related disease," Lauri Markowitz, MD, team lead, HPV, associate director of science, from the CDC in Atlanta, Georgia, shared an in-depth analysis of the transformative impact of HPV vaccines.
Prophylactic HPV vaccines have demonstrated remarkable efficacy, exceeding 98%, and they are already proving to be effective in the prevention of anogenital warts, precancerous lesions, and cancer alike.
Recommendations for HPV vaccination have evolved since 2006, Markowitz noted. While initially recommended for females 11 or 12 years (with catch-up available through age 26), the guidelines expanded in 2011 to include males of the same age. With the addition of shared clinical decision-making for older individuals, vaccination is now available to those as young as 9 years, or as old as 45 years.
The impact of HPV vaccination in the United States has been impressive. Despite a lower rate of uptake compared to other vaccines, coverage rates for females now reaches 65%, with 78% receiving at least one dose. For males, the uptake was faster, with coverage roughly at similar levels. However, there remains a notable variation in coverage state-to-state, with the lowest rates in Montana, Texas, Florida, Wyoming, and Mississippi according to a 2021 CDC National Immunization Survey.
The most immediate marker of vaccination impact has been the decline in genital warts prevalence. Among those aged 14 to 19 years, there was a 56% reduction in prevalence from 2007 to 2010 (comparing pre- and post-vaccine eras). As coverage increased, the prevalence continued to decline, with an 88% reduction in vaccine-type HPV prevalence in those aged 14 to 19 years in 2018.
While monitoring the impact on cervical precancer screening is challenging due to evolving screening recommendations, there has been a significant decrease in precancerous lesions among younger age groups, while an increase was observed in older age groups (possibly due to increased detection and improved screening). Interestingly, these declines were strongest for vaccine types, with some additional evidence of cross-protection for non-vaccine types.
While the evidence for improved cancer rates will take years to manifest, the impact of these vaccines is also evident when assessing the incidence of juvenile onset recurrent respiratory papillomatosis. This rare but severe disease caused by HPV 6 or 11 has shown a steady and marked decrease since 2004.
Internationally, the vaccine's impact is just as clear. A meta-analysis from 65 studies across 4 high-income countries showed rapid declines in anogenital warts among females, even with herd immunity effects observed in males where vaccination was only offered to females. Further, a Swedish study linked HPV vaccination to a reduced risk of cervical cancer at a population level.
Despite these impressive results, Markowitz emphasized that challenges persist. The World Health Organization notes that many countries with high cervical cancer rates do not utilize the vaccine, primarily due to cost, delivery, and supply constraints.
Markowitz's lecture underscored the transformative role of HPV vaccination in reshaping the epidemiological landscape of HPV and its associated sequelae. Her work at the CDC, coupled with her collaboration with the Advisory Committee on Immunization Practices, has shaped the HPV vaccination program in the United States, and contributed to the hope for a future with reduced HPV-related morbidity and mortality thanks to this “cancer-preventing vaccine," said Markowitz.
Reference
Markowitz, L. How HPV vaccination has changed HPV epidemiology and HPV-related disease. IDWeek 2023. October 14, 2023. Boston, Massachusetts.
Articles in this issue
almost 2 years ago
Measuring TSB with an app may be nextalmost 2 years ago
Newborn with midline neck lesionalmost 2 years ago
If a fetus with DS has a normal OB-US, how useful is further screening?about 2 years ago
A toddler with a pruritic rashabout 2 years ago
The role of culinary education in pediatricsabout 2 years ago
Delta-8 accessibility to minors onlineabout 2 years ago
How childhood sexual abuse affects adult survivorsNewsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.