A 3-week-old girl with vesicular rash
A 3-week old girl comes to an emergency room with vesicular eruptions and recent mild nasal congestion and fussiness. What’s the diagnosis?
The case
A 3-week-old infant with vesicular eruptions receives a diagnosis of varicella requiring hospitalization and intravenous acyclovir.
History
A 3-week-old previously healthy full term girl presented to the pediatric emergency department with 2 lesions on the body that had developed 3 days earlier—1 lesion on the forehead and 1 perianal lesion. Her parents said that she had recently developed mild nasal congestion and fussiness but denied fever, purulent drainage, bleeding from the lesions, or rashes elsewhere. The infant had been feeding well with appropriate urine output for age. Her mother had a history of genital warts, but neither parent had a history of oral or genital herpes simplex virus (HSV) infection. The patient presented to her pediatrician earlier that day and after evaluation, given her young age, she was referred to the emergency department for work-up of a possible HSV infection.
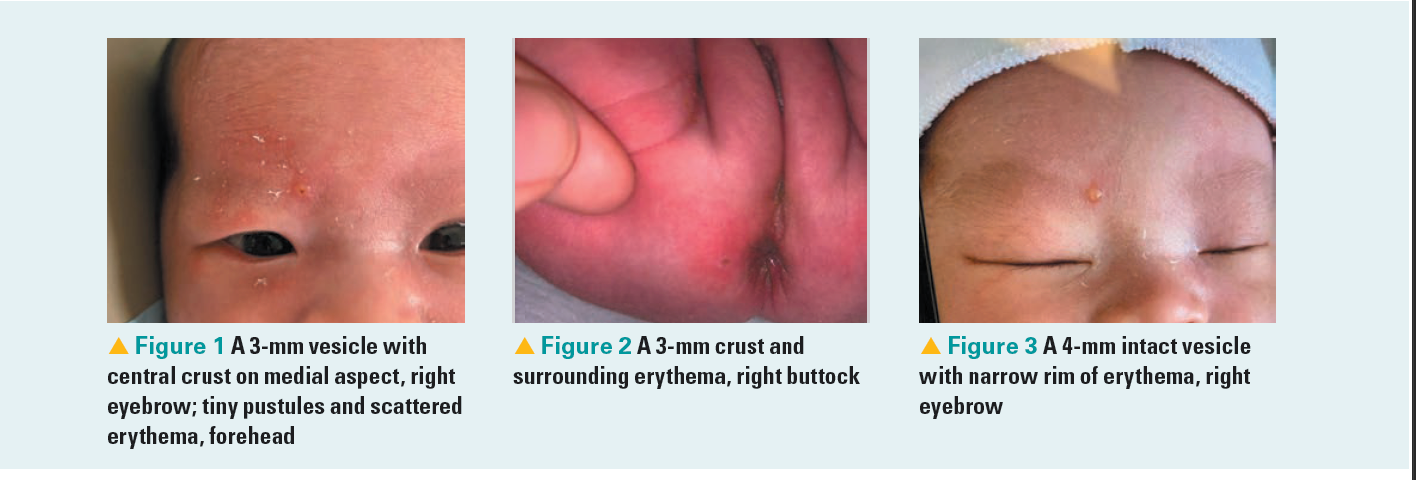
Figures 1 to 3
Physical examination
In the pediatric emergency department, the infant appeared well. Her temperature was 37.3° C, heart rate was 156 beats per minute, respiratory rate was 33 breaths per minute, and her oxygen saturation level was 100% on room air. She weighed 3.3 kilograms. Physical examination was significant for a ruptured 3-mm vesicle with a central crust on the medial aspect of the right eyebrow (Figure 1) with some tiny pustules and scattered erythema and scale on the forehead, nasal bridge, and eyelids with the right side lesions more prominent than the left. She also had a 3-mm crust with a narrow scaly border and surrounding erythema on the right buttock (Figure 2). Her parents brought a photo of the right eyebrow lesion from 2 days before it ruptured that showed a 4-mm intact vesicle with a narrow rim of erythema (Figure 3). The patient had normal tone, normal strength, and open, flat anterior and posterior fontanelles. There was no appreciable hepatosplenomegaly, lymphadenopathy, or rash noted elsewhere.
Differential diagnosis
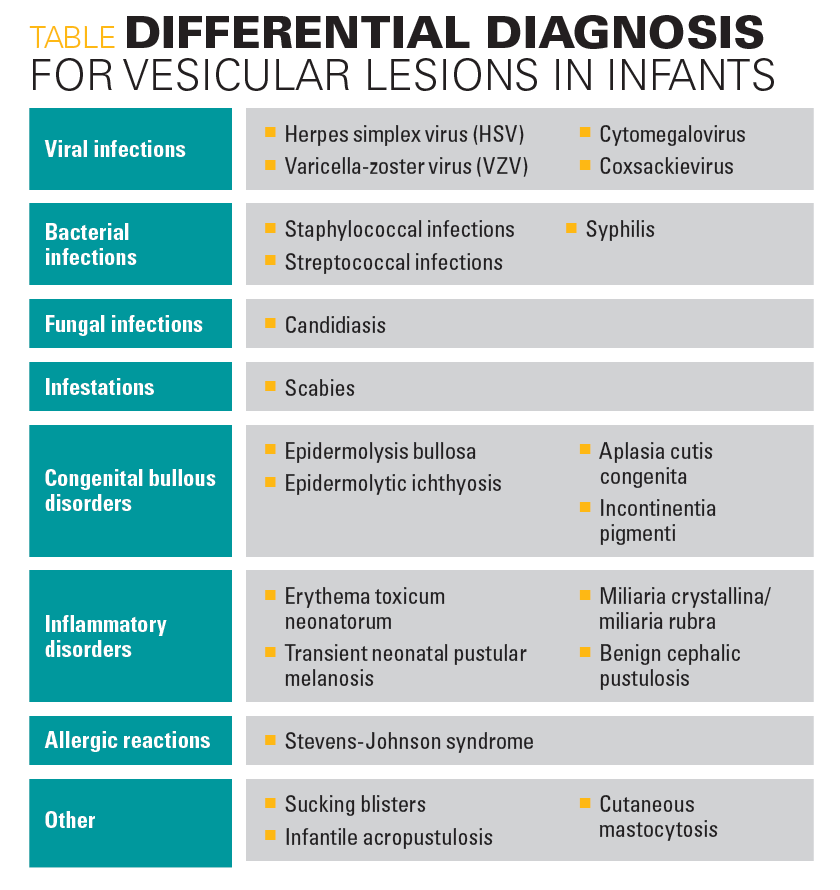
Given her age and presentation, HSV infection was the leading and most concerning diagnosis in the differential diagnosis, but varicella and staphylococcal infections were also considered. A differential diagnosis for vesicular lesions in infants is shown on Table 1 and includes infectious etiologies and well as congenital and neonatal bullous disorders.
Table
Laboratory studies
A complete neonatal sepsis rule-out was performed given the infant’s age. Laboratory studies revealed an unremarkable complete blood cell count in addition to differential, comprehensive metabolic panel, C-reactive protein, procalcitonin, and urinalysis. A lumbar puncture produced blood-tinged fluid on the second attempt, and initial cerebrospinal fluid (CSF) studies showed 416 white blood cells per microliter and 605,000 red blood cells per microliter, with 4% neutrophils, 83% lymphocytes, 1% reactive lymphocytes, and 12% monocytoid cells. The laboratory was unable to run protein and glucose studies on the CSF. No organisms were seen on CSF Gram stain. Cultures from blood, urine, and CSF were sent in addition to multiplex polymerase chain reaction (PCR) testing with a respiratory pathogen PCR panel from the nasopharynx and a CSF meningitis/encephalitis panel. The patient was started on empiric intravenous ampicillin, gentamicin, and acyclovir and admitted to the neonatal intensive care unit (NICU) for further treatment.
Diagnosis
Shortly after admission, the infant’s CSF meningitis/encephalitis panel resulted positive for varicella-zoster virus (VZV) and her respiratory pathogen PCR panel resulted positive for coronavirus (not SARS-CoV-2). Pediatric infectious diseases (ID) was consulted, given the presence of varicella infection in a newborn with no clear history of exposure. The ID consult recommended HSV and VZV PCR tests from the patient’s blood, CSF, and a skin lesion, as well as HSV PCR tests from her conjunctiva, nares, oropharynx, and rectum. All HSV PCR tests resulted negative. Notably, the patient’s PCR test results were positive for VZV in the skin lesion and blood but not in the CSF. As the CSF VZV PCR test was negative, the VZV result from the CSF meningitis/encephalitis panel was thought to be representative of sampling from the blood introduced from the traumatic lumbar puncture. Nevertheless, the infant was found to have positive VZV PCR testing from multiple sources (ie, skin lesion, blood).
Discussion
Varicella, commonly known as chickenpox, is caused by a primary VZV infection. It most often affects children unimmunized against the disease, with the highest incidence in children aged between 1 and 9 years.1-3 It usually results in mild to moderate illness in otherwise healthy individuals, but tends to be more severe in infants, teenagers, and adults compared with school-aged children.4-6 Asymptomatic cases are rare.5 Some presentations of varicella can be severe and life-threatening, especially in cases of vertical transmission (ie, either fetal infection after the development of maternal varicella or neonatal infection around the time of delivery) and in immunocompromised individuals.5-7 Possible complications include bacterial superinfection of skin lesions, pneumonia, and central nervous system involvement.5 The risk of hospital admission or dying from varicella in infants is higher than that in children.4,8-10
Varicella presents with a pruritic rash with vesicles in different stages of development, often accompanied by fever, malaise, and decreased appetite.5 The rash tends to be more prominent on the face and trunk than on the extremities.1 VZV is transmitted via airborne droplets or vesicular fluid.5,6 It is thought to multiply in regional lymph nodes, then to spread to the viscera.1 The incubation period for varicella varies between 10 to 21 days. Individuals with varicella are contagious from 1 to 2 days before the onset of rash until all of the lesions have crusted over, which is typically at least 5 days after the onset of rash.5-7
Varicella can be diagnosed clinically by the presentation of a characteristic rash. In cases that require laboratory confirmation, the diagnostic method of choice for varicella is a VZV DNA PCR test from vesicular fluid or a scab—vesicles contain large amounts of virus and PCR is more sensitive than a viral culture or a direct fluorescent antibody assay.1,5,6,11
In otherwise healthy children, treatment for varicella is supportive care to address fever and pruritus and to maintain adequate hydration.1 Varicella in a newborn does not universally require antiviral treatment, and there is no consensus by experts in the literature about management.9 However, the decision to treat is determined by host characteristics, illness severity, and initial response to therapy.5,10 The antiviral treatment of choice is acyclovir, which prevents viral DNA synthesis by inhibiting the viral DNA polymerase and is most effective if administered intravenously within 72 hours of disease.1,7,12 Blumental et al recently recommended acyclovir treatment for all patients less than 1 month of age with clinical signs of varicella.7
Both of the infant’s parents reported having a childhood illness consistent with varicella and tested positive for VZV immunoglobulin G. As the patient’s mother tested positive, it is likely that maternal transfer of antibody contributed to a less severe course of varicella (though this is confounded by the fact that the infant was started empirically on intravenous acyclovir upon admission).9,10 Given varicella’s incubation period, we presume the patient was exposed to VZV during the first week of life. Though no clear source of infection was ultimately identified, it is most likely that the infant was exposed in her pediatric clinic, as she was seen in clinic on days of life 3, 5, 6, and 14 for weight and jaundice checks and a routine 2-week well care visit.
Treatment and patient outcome
The day after admission, the infant developed additional vesicular lesions on her trunk and extremities. Given the patient’s positive CSF meningitis/encephalitis panel—despite the history of a traumatic lumbar puncture and the negative dedicated VZV PCR from the CSF—ID recommended a plan to treat for at least 7 days while continuing to monitor the infant. Intravenous acyclovir was continued, but antibiotics were discontinued by 48 hours as there was less concern for bacterial infection and negative cultures. Amplitude-integrated electroencephalography was unremarkable. The patient had 1 isolated temperature to 38.0°C that resolved without medication. She was continued on intravenous acyclovir for 1 week until hospital discharge. At that time, all cultures were negative for bacterial infection and the infant’s vesicular lesions had scabbed over.
This case highlights the importance of providers including varicella in the differential diagnosis of vesicular lesions in infants, as often its consideration is overshadowed by the concern for possible HSV. Continuing to administer routine varicella vaccinations is also important from a public health perspective, in order to maintain herd immunity in populations.
References
1. Heininger U, Seward JF. Varicella. Lancet. 2006;368(9544):1365-1376. doi:10.1016/S0140-6736(06)69561-5
2. Gershon AA, Breuer J, Cohen JI, et al. Varicella zoster virus infection. Nat Rev Dis Primers. 2015;1:15016. doi:10.1038/nrdp.2015.16
3. Kennedy PGE, Gershon AA. Clinical Features of Varicella-Zoster Virus Infection. Viruses. 2018;10(11). doi:10.3390/v10110609
4. Meyer PA, Seward JF, Jumaan AO, Wharton M. Varicella mortality: Trends before vaccine licensure in the United States, 1970-1994. J Infect Dis. 2000;182(2):383-390. doi:10.1086/315714
5. Varicella-zoster virus infections. Red Book: 2018 Report of the Committee on Infectious Diseases. 31st ed. Itasca, IL: American Academy of Pediatrics; 2018:869-883.
6. Sauerbrei A, Wutzler P. Neonatal varicella. J Perinatol. 2001;21(8):545-549. doi:10.1038/sj.jp.7210599
7. Blumental S, Lepage P. Management of varicella in neonates and infants. BMJ Paediatr Open. 2019;3(1):e000433-2019-000433. eCollection 2019. doi:10.1136/bmjpo-2019-000433
8. Galil K, Brown C, Lin F, Seward J. Hospitalizations for varicella in the United States, 1988 to 1999. Pediatr Infect Dis J. 2002;21(10):931-935. doi:10.1097/00006454-200210000-00009
9. Lecuyer A, Levy C, Gaudelus J, et al. Hospitalization of newborns and young infants for chickenpox in France. Eur J Pediatr. 2010;169(10):1293-1297. doi:10.1007/s00431-010-1212-9
10. Gowin E, Wysocki J, Michalak M, Januszkiewicz-Lewandowska D. Too young to be vaccinated: Hospitalizations caused by varicella among children in the first year of life. Int J Infect Dis. 2017;62:52-55. doi:10.1016/j.ijid.2017.07.009
11. Sauerbrei A. Diagnosis, antiviral therapy, and prophylaxis of varicella-zoster virus infections. Eur J Clin Microbiol Infect Dis. 2016;35(5):723-734. doi:10.1007/s10096-016-2605-0
12. Whitley RJ. The use of antiviral drugs during the neonatal period. Clin Perinatol. 2012;39(1):69-81. doi:10.1016/j.clp.2011.12.004
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.