A case of acute psychosis that will make your head spin
A 12-year-old previously healthy male was transferred to a children's hospital from a psychiatric unit for new onset psychosis and an abnormal electroencephalogram. What's the diagnosis?
The case
A 12-year-old previously healthy male was transferred to our institution (Children’s Hospital of New Jersey) from a psychiatric unit for new onset psychosis and an abnormal electroencephalogram (EEG). Less than 2 weeks prior to initial presentation, the patient had upper respiratory tract symptoms and was treated with antibiotics for bilateral acute otitis media. He then developed progressively worsening headaches, auditory and visual hallucinations, behavioral changes, and suicidal ideations. After multiple emergency department visits, the patient was admitted to an inpatient psychiatric unit and started on risperidone and benztropine. Despite psychiatric treatment, his symptoms persisted. A video EEG was done to rule out seizures and was abnormal, prompting transfer.
On admission to our facility, the patient was found to be sleepy and combative with extreme emotional lability. His mental status waxed and waned throughout his first week of admission, with periods of lucidity alternating with periods of slow, slurred speech, agitation, hyper sexuality, visual and auditory hallucinations, insomnia, and paranoia. Physical exam was unremarkable, without any focality on neurologic examination
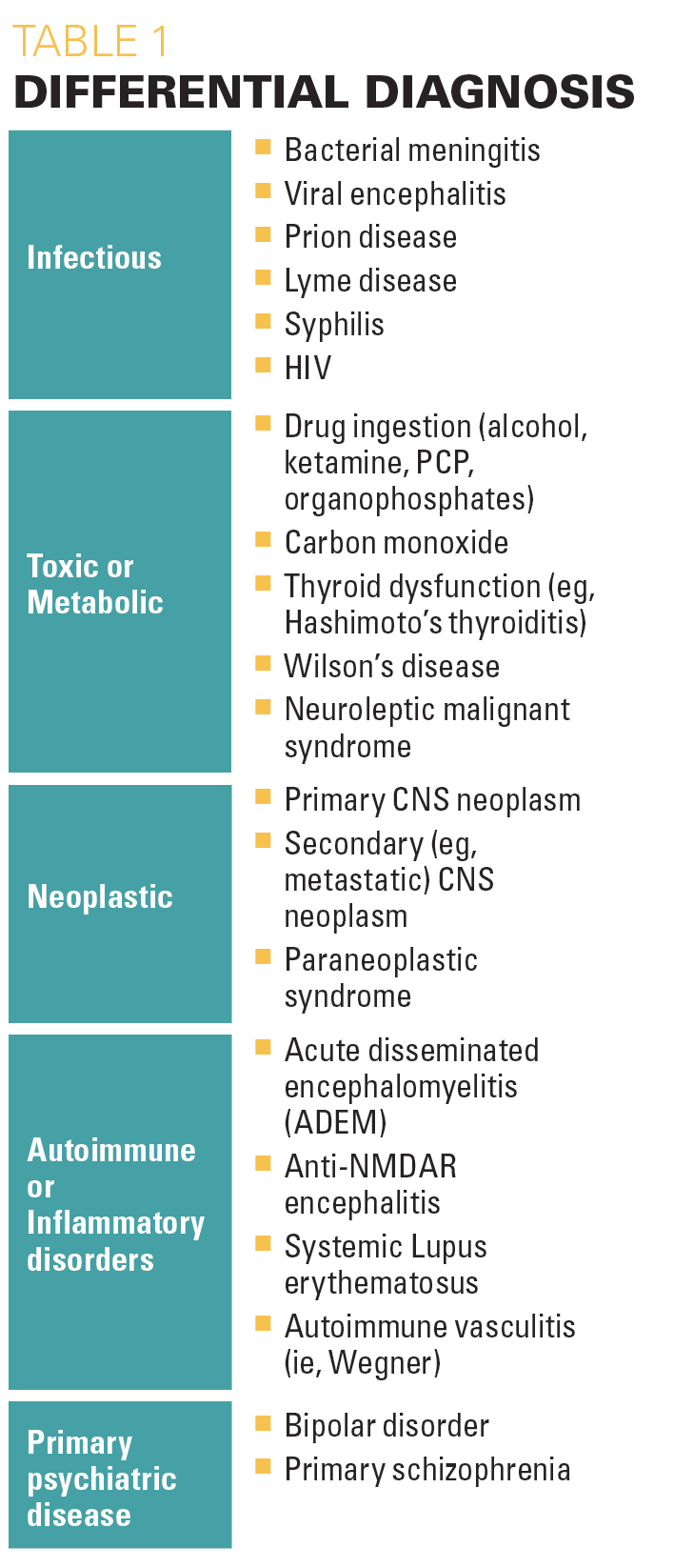
Differential Diagnosis
Due to acute onset neuropsychiatric symptoms of unknown etiology, the patient was initially admitted to the pediatric intensive care unit for close monitoring. Initial differential diagnosis was broad given the patient’s new-onset severe neuropsychiatric symptoms (Table 1). Bacterial or viral meningitis/encephalitis may present similarly, and upper respiratory symptoms may precede presentation, as was the case in our patient. However, these patients also typically present with fever and nuchal rigidity, neither of which were present in our patient. Other infectious etiologies include HIV, syphilis, Bartonella, and Lyme disease. Toxic ingestion, especially of alcohol, ketamine, phencyclidine, or organophosphates can cause new onset agitation; however, symptoms typically do not last as long as they did in our patient. Endocrine and metabolic derangements are also known to cause neuropsychosis. Neoplastic disorder, either primary or secondary, as well as paraneoplastic syndromes can present with focal neurologic signs and/or neuropsychiatric symptoms. Rheumatologic disorders, including lupus, may also present with psychiatric symptoms, though our patient had no other stigmata typical of lupus. Entities that cause inflammation of the central nervous system, such as autoimmune encephalitis (eg, anti-N-methyl-D-asparate receptor [NMDAR] encephalitis and acute disseminated encephalomyelitis) can present with a similar constellation of symptoms as our patient and must also be considered. Primary psychiatric disease should be a diagnosis of exclusion once all organic causes are ruled out or considered sooner if the patient has a known psychiatric history.
Table 1: Differential diagnosis
Examination and Testing
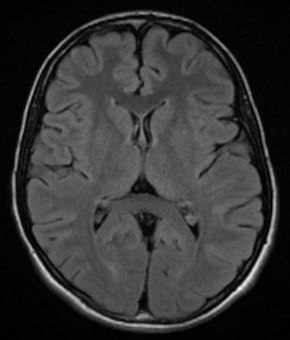
Video EEG at our institution did not demonstrate evidence of seizures. Head computed tomography (CT) on admission showed hypoattenuation in bilateral thalami, though more on the right side as compared to the left side. Magnetic resonance imaging (MRI), magnetic resonance angiogram, and magnetic resonance venography were done given concern for vasculitis and significant for hyperintensity flair in the medial thalami/massa intermedia. Urine toxicology screen was negative. A lumbar puncture showed a high opening pressure and cerebrospinal fluid (CSF) pleocytosis with white blood cells of 26, suggesting infectious versus autoimmune processes. Further infectious work-up, including a complete blood count, procalcitonin, meningitis/encephalitis panel, antistreptolysin O (ASO) titer, group A streptococcus direct DNA probe, rapid plasma regain (RPR), Epstein-Barr virus, Lyme disease titers, HIV, quantiferon gold, Bartonella antibodies, and herpes simplex virus (HSV) antibodies were all negative. Rheumatologic workup, including erythrocyte sedimentation rate, c-reactive protein, antinuclear antibody, anti-ds DNA, C3, C4, proteinase-3 antibody, myeloperoxide antibody, and centromere antibody were unrevealing. A comprehensive metabolic panel, lactic acid, ammonia, thyroid stimulating hormone (TSH), free T4, vitamin B1, ceruloplasmin, and copper studies did not demonstrate a toxic or metabolic cause. A CT abdomen and pelvis was done to rule out an oncologic process and was within normal limits. Alpha-fetoprotein was normal. An autoimmune and paraneoplastic panel was sent from the CSF, however results were not available during the patient’s hospital admission.
Diagnosis
Laboratory evaluation was largely unrevealing, except for slight CSF pleocytosis. This, along with the CT and MRI findings and the clinical picture of waxing and waning aggression, agitation, and insomnia was concerning for autoimmune encephalitis. One week after discharge, CSF studies returned positive for anti-NMDAR and anti-MOG antibodies.
Patient outcome
Given concern for anti-NMDAR encephalitis and known poorer prognosis with delay in treatment, our patient was presumptively treated with high-dose steroids and intravenous immune globulin (IVIG). He did not demonstrate improvement in his neuropsychiatric symptoms with this treatment, and continued to require daily lorazepam for agitation. The patient was subsequently treated with rituximab with clinical improvement.
Figure 1

Our patient was admitted for 16 days and discharged home with mild cognitive delays but no activity restrictions. After discharge, the patient had close follow-up with neurology and hematology/oncology, including a 2nd dose of rituximab and a repeat MRI that showed interval complete resolution of previously identified T2-weighted-fluid-attenuated inversion recovery hyperintensity within pulvinar region of bilateral thalami. He was given a 504 plan for additional time in academic activities, however reports not using it and is earning B’s in school.
Figure 2

In addition, the neuropsychiatric team evaluated the patient in order to delineate sequelae of neurocognitive deficits due to encephalitis. His first evaluation was approximately 3 months after discharge and showed weaknesses in sustained visual attention, auditory memory, and visual memory. There were also concerns regarding impulse control. The neuropsychiatric team conducted a follow up evaluation about 7 months later. Our patient demonstrated significant improvement, specifically in attention, concentration, and memory domains of the evaluation. He also exhibited improved self-control during testing.
Discussion
The NMDA is a glutamate-gated ion channel critical for multiple central nervous system (CNS) functions1,2 including processes underlying learning, memory and neuroplasticity.
Figure 3
Anti-NMDAR encephalitis is an autoimmune disorder with IgG antibodies against the NR1 and NR2 subunit of the NMDA receptor. The presenting symptoms of anti-NMDAR encephalitis are quite broad,3 but usually evolve in stages including a prodrome of fever, headaches and viral-like symptoms. Days to weeks after this prodromal phase begins the onset of psychiatric and behavioral problems,4 including personality and behavioral changes, autonomic and cognitive dysfunction, and finally neurologic decompensation leading to insomnia, seizures, altered levels of consciousness, and breathing or autonomic instability.5 In multiple studies, it was shown that the condition, when identified, affects predominantly females (up to 80% of females vs males). Age ranges from 18-35 years, with 40% of patients aged younger than 18 years.1
This disorder is a leading cause of encephalitis in young patients, with up to 4% of patients with encephalitis having NMDAR antibodies. In women aged older than 18 years, the majority will have the presence of an underlying tumor, such as teratoma of the ovary, however in children, this is uncommon.6
Diagnosis of anti-NMDAR encephalitis is made by identification of NMDAR antibodies in the CSF or serum. First line therapy is typically high dose corticosteroids. Second line therapy includes IVIG and/or plasma exchange. Other attempted therapies include rituximab, azathioprine, and cyclophosphamide. If a neoplasm is found, treatment includes surgical excision of neoplasm, if possible.
Anti-NMDAR encephalitis is the second leading cause of immune-mediated encephalitis, after acute disseminated encephalomyelitis.7 Despite the prevalence of the condition, anti-NMDAR encephalitis is an overlooked diagnosis.8 Timely diagnosis and treatment of anti-NMDAR encephalitis should be considered early on in patients presenting with new onset of altered mental status of unknown etiology. Anti-NMDAR encephalitis is a complex syndrome, with a severe disease course and broad differential diagnosis. Mortality can be up to 25%, whereas many other patients are left with cognitive deficits that may affect education, work, or social life. However, with early recognition and aggressive treatment, prognosis remains good with most cases (up to 75%) making a full recovery or only having mild disability,8 as was demonstrated in our patient.
Reference
1. Miya, Kazushi, Takahaski, Tukitoshi, and Mori, Hisashi. Anti-NMDAR autoimmune encephalitis. Brain & Development. 2014. 36: 645-652.
2. Blanke ML, VanDongen AMJ. Activation Mechanisms of the NMDA Receptor. In: Van Dongen AM, editor. Biology of the NMDA Receptor. Boca Raton (FL): CRC Press/Taylor & Francis; 2009. Chapter 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK5274/
3. Armangue, Thais MD, Petit-Pedrol, Mar, BS, and Dalmau, Josep, MD, PhD. Autoimmune Encephalitis in Children. J Child Neurol. 2012; 27 (11): 1460-1669.
4. Barry, Helen, et al. “Anti-NMDA Receptor Encephalitis: an Important Differential Diagnosis in Psychosis.” British Journal of Psychiatry, vol. 199, no. 6, 2011, pp. 508–509., doi:10.1192/bjp.bp.111.092197.
5. Day, Gregory S., et al. “Anti-NMDA-Receptor Encephalitis: Case Report and Literature Review of an Under-Recognized Condition.” Journal of General Internal Medicine, vol. 26, no. 7, 2011, pp. 811–816., doi:10.1007/s11606-011-1641-9.
6. Armangue, Thaís, et al. “Pediatric Anti-N-Methyl-D-Aspartate Receptor Encephalitis—Clinical Analysis and Novel Findings in a Series of 20 Patients.” The Journal of Pediatrics, vol. 162, no. 4, 2013, doi:10.1016/j.jpeds.2012.10.011.
7. Finke, Carsten, et al. “Cognitive Deficits Following Anti-NMDA Receptor Encephalitis.” Journal of Neurology, Neurosurgery & Psychiatry, vol. 83, no. 2, 2011, pp. 195–198., doi:10.1136/jnnp-2011-300411.
8. Kelley, Patel, Marin, Corrigan, Mitsias, Griffith. Autoimmune Encephalitis: Pathophysiology and Imaging Review of an Overlooked Diagnosis. Am J Neuroradiolology. 2017; 38: 1070-78.
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.