Becker Nevus and Molluscum Contagiosum
A teenaged boy presented with this large, light brown pigmented macule that developed after he returned from a vacation with his family in Florida. He takes no medications and has been healthy.
Case 1:

A teenaged boy presented with this large, light brown pigmented macule that developed after he returned from a vacation with his family in Florida. He takes no medications and has been healthy.
What is this lesion?


Case 1: This is a Becker nevus, a disorder of pigmentation. These nevi most commonly occur on the shoulder or anterior chest. On occasion, a Becker nevus may occur after the patient has had excessive exposure to sunlight that may have resulted in a sunburn.
Examination reveals a large, light brown pigmented macule that usually has prominent perifollicular papules and coarse terminal hairs scattered over the pigmented area. The borders of the patches are well demarcated and irregular. Occasionally, acne develops within the pigmented area.
A Becker nevus is a pigmented, hairy nevus that may be associated with the hamartomatous development of smooth muscle fibers or sebaceous glands that may give the lesion a pebbly or thickened appearance. Histologically, the number of melanocytes is normal or slightly increased; the basal cells of the epidermis show increased pigmentation.
Becker nevi are benign; only in the rarest of instances have there been reports of the development of a malignant melanoma within a Becker nevus. One should also look for the rare association with hypoplasia of the underlying structures associated with the nevus (ie, breast hypoplasia). The predominance in males (6:1), the onset at puberty, and the hypertrichosis with associated sebaceous hyperplasia and occasional acne suggest that this is an androgen-mediated abnormality.
Laser therapy may be of benefit, but recurrences are common. The terminal hairs may be removed by any acceptable hair removal technique.
Case 2:

This young girl has molluscum. Her pediatrician diagnosed this condition several months ago, but despite therapy with a multitude of OTC products (as directed by friends, family, and concerned practitioners), the lesions have persisted. The patient's younger sister is affected as well.
How would you counsel the child's parents?
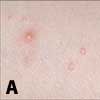

Case 2: This young girl had multiple 1- to 5-mm translucent/yellow papules with central umbilication scattered about her axilla and left lateral trunk (A). A number of these molluscum lesions had areas of "eczema" about them. A lesion on her left forearm (B) showed intense inflammation. The mother advised that the girl was "atopic," but said that her atopic eczema was under good control and that the only manifestation was the eczema on her forearms.
Molluscum contagiosum is a common condition. In a study from Australia, an enzyme-linked immunosorbent assay for molluscum contagiosum virus was used to determine the antibody status in 357 uninfected persons. Three percent of those between 6 months and 2 years had antibodies to the molluscum virus DNA; seropositivity increased to 39% in those 50 years and older.
The lesions of molluscum are encapsulated areas of "viral particles." Their spread is most often through skin-to-skin contact. Autoinoculation and infection of others can occur as a result of warm water exposure. This occurs either in the bathtub in the event of autoinoculation or through heated swimming pools and hot tubs in small "epidemics." I often see entire swim teams or clusters of patients from rural locations; it is clearly evident that the community pool is a common source for a molluscum outbreak.
In sexually active adolescents, mollusca are the result of skin-to-skin contact with sexual partners who have infectious papules over the genitalia and pubic skin. In fact in adolescents, such contact is almost certainly the source of molluscum contagiosum virus infection. In younger children, the development of molluscum does not suggest sexual abuse but rather inoculation from bathing or swimming, from playful contact with family members, or from an as yet unknown mechanism.
It is not unusual to see unexplained asymmetric patches of "eczema" that are unresponsive to topical corticosteroids as a manifestation of molluscum. The lesions of molluscum develop a dermatitis about them, which may extend for many centimeters in irregular patterns about a single lesion. The eczema, which is often unexplained and asymmetric, occurs most commonly in patients who are atopic; however, it is easily recognized as distinct from their usual pattern of eczema. I think this is a dermatitis that signals an inflammatory reaction to the molluscum contagiosum virus, and I often see this as a pre-clearance phenomenon. I try to avoid using topical corticosteroids with such eczema unless the itching is intense. I find that treating the small molluscum lesion in the eczematous patches produces spontaneous resolution of the "eczema."
Treatment of molluscum requires clinical judgment and compassion. The mollusca themselves will always disappear spontaneously if given enough time. The treatments themselves must be destructive and local. Curettage or cryotherapy is often effective; in younger persons, however, these procedures are often very traumatic--even when a topical anesthetic is used. Cantharadine, 10% potassium hydroxide, and silver nitrate paste have all been proposed as chemical destructive treatments. These are effective and cause minimal discomfort. All treatments, whether physical or chemical, should be applied to individual lesions, sparing surrounding tissue.
Patients should avoid bathing in warm water either by themselves or with siblings and take showers instead while they are infected. They should also avoid heated swimming pools while infected to avoid autoinoculation.
In patients with sexually transmitted molluscum, treatment is destructive. Cryotherapy is my most useful tool. I often instruct affected young adults to pierce the top of the lesions and try to extrude the central core using lateral pressure with the rounded end a popsicle stick or similar device if I miss any using cryotherapy or if a small number return.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.