Juvenile Nasopharyngeal Angiofibroma
Sixteen-year-old boy referred to pediatric emergency department (ED) by his primary care physician with a history of headache, blurred vision, and mild proptosis of right eye. Vision: 20/200 OD (right eye) and 20/25 OS (left eye).


HISTORY
Sixteen-year-old boy referred to pediatric emergency department (ED) by his primary care physician with a history of headache, blurred vision, and mild proptosis of right eye. Vision: 20/200 OD (right eye) and 20/25 OS (left eye). The patient's vision had been tested 6 months earlier during routine physical examination; vision at that time: 20/40 OD and 20/25 OS.
A week before presentation, patient noticed that his right eye "felt a little bigger" than the left. His primary physician prescribed tobramycin ophthalmic eye drops and oral pseudoephedrine. Two days before presentation in the ED, the patient had a frontal headache and blurring of vision; his right eye had increased in size. He denied any double vision, weight loss, or facial anhidrosis.
No history of trauma; fever; ocular itchiness, redness, or discharge; rash; or travel. Patient did not smoke, abuse any substances, or drink alcohol. Not sexually active.

PHYSICAL EXAMINATION
Vital signs: temperature, 99.1?251-186?F (37.3?251-186?C); respiratory rate, 18 breaths/ min; heart rate, 86 beats/min; blood pressure, 110/80 mm Hg.
Well-looking adolescent with no obvious distress, discomfort, or pain. Alert and oriented with normal speech and articulation. Right eye had significant proptosis with partial ptosis. Extraocular movements limited; restriction more significant on right lateral gaze and on downward and medial movements. Function of other cranial nerves intact. Conjunctivae and sclerae normal; no redness, discharge, or tearing. The right side of face and cheek slightly swollen. Right pupil measured approximately 5 mm in diameter; the left measured 3 mm. No light reflex in the right eye, but consensual light reflex was present. Vision was similar to the primary care provider's findings. No other noteworthy findings.
WHATS YOUR DIAGNOSIS?
LABORATORY FINDINGS
Complete blood cell count, 13.6 3 109/L, with 77% neutrophils and 17.3% lymphocytes. Hemoglobin, 14.7 g/dL. Serum electrolyte concentrations and urinalysis results, normal.
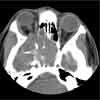
IMAGING STUDIES
CT scans of the orbits and brain as shown.
The biopsy-confirmed diagnosis was juvenile nasopharyngeal angiofibroma (JNA) that extended into the right orbit, ethmoid sinus, sphenoid sinus, right pterygoid process, and right middle cranial fossa.
JNA is a benign tumor that usually affects adolescent males (7 to 19 years).1 It is rare in persons older than 25 years.This highly vascular tumor originates from the pterygopalatine fossa and extends through the sphenopalatine foramen to involve the sphenoid sinus.
JNA usually presents as nasal obstruction,headache, facial swelling, and epistaxis (which is mostly unilateral and recurrent). The tumor can also cause anosmia, hyposmia, otalgia, serous otitis media from eustachian tube blockage, and impaired hearing. Orbital mass and proptosis occur in 10% to 15% of cases.1
Radiologic findings that characterize JNA are:
•Tumor location in the nasopharynx.
•Anterior bowing of the posterior wall of the maxillary sinus.
•Widening of the pterygopalatine fossa.
•Erosion of the pterygoid process.
CT scans provide good-quality images of bone changes. However, MRI is superior to CT in demonstrating the difference between tumor and fluid retention in the paranasal sinuses, as well as any extension of the intracranial mass, tumor vascularity, and soft tissue margins.2 Typical radiologic findings combined with characteristic clinical manifestations allow initial diagnosis.3
DIFFERENTIAL DIAGNOSIS
Diagnostic considerations include orbital cellulitis or abscess, orbital cavernous hemangioma, and orbital tumor.
Orbital cellulitis may occur as an extension of periorbital cellulitis or infected ethmoid sinusitis or from adjacent facial infection. Pain is mainly retro-orbital; it is aggravated by ocular movement and is associated with edema and erythema of the lid, proptosis, conjunctival inflammation, chemosis, and loss of visual acuity. Affected patients tend to be quite ill, toxic-appearing, and lethargic. Aggressive intravenous antimicrobial treatment and monitoring of CNS involvement are vital.
CT is required to rule out any involvement of subperiosteal bone or abscess formation. Urgent referral for ophthalmologic consultation is warranted if any subperiosteal or orbital abscess is present.
Orbital cavernous hemangiomas are benign intraorbital tumors that develop in children and adults. These slow-growing vascular tumors can present with painless and progressive proptosis. Most are unilateral. Diminished visual acuity, diplopia, decreased extraocular muscle movement, and papillary dysfunction can occur.4
Orbital tumors include neuroblastoma--the most common lesion to metastasize to the orbit in children. These usually present with an acute onset of proptosis (unilateral or bilateral), ptosis, and eyelid ecchymoses.
Retinoblastoma is a relatively uncommon tumor of childhood. Those younger than 5 years are usually affected (in 95% of pediatric cases).5 Presenting symptoms in older patients include leukocoria, decreased visual acuity, pain, floaters, and strabismus. The most common presenting signs in young children are leukocoria (60%) and strabismus (22%).6 Most retinoblastomas are unilateral.
Pseudotumor of the orbit may be unilateral or bilateral. This condition usually presents with headache, orbital pain, proptosis, eyelid edema or erythema, decreased or restricted eye movement, and diplopia.
OUTCOME OF THIS CASE
This patient was referred to a tertiary center. There, the feeding vessels of the lesion were embolized; this was followed by radiation. The tumor decreased in size and the patient's vision in the right eye is now 20/60.
References:
REFERENCES:
1.
Tewfik TL, Al Garni MA. Juvenile nasopharyngeal angiofibroma. Available at:
http://www.emedicine.com/ENT/topic470.htm
. Accessed January 12, 2007.
2.
Szymanska A.Computed tomography and magnetic resonance imaging in diagnosis and evaluation of the juvenile nasopharyngeal angiofibroma.
Pol J Radiol.
2004;69:53-58.
3.
Tewfik TL, Tan AK, al Noury K, et al. Juvenile nasopharyngeal angiofibroma.
J Otolaryngol.
1999;28:145-151.
4.
Olitsky SE, Nelson LB. Disorders of the eye. In: Behrman RE, Kliegman RM, Jenson HB, eds.
Nelson Textbook of Pediatrics.
16th ed.Philadelphia: WB Saunders; 2000:1935.
5.
Shields CL, Shields JA, Shah P. Retinoblastoma in older children.
Ophthalmology.
1991;98:395-399.
6.
Zitelli BJ, Davis HW, eds.
Atlas of Pediatric Physical Diagnosis.
3rd ed. Philadelphia: Mosby-Wolfe; 1997:594-595, 711-712.