Bruise-like marks on a healthy teenage male’s back
A 15-year-old male first noticed the marks on his back during a recent vertical growth spurt. On exam there are multiple horizontal violaceous linear striae on his back. He is otherwise healthy and denies any history of back injury or exposure to topical or systemic steroids. What's the diagnosis?
The case
You are asked to evaluate a healthy 15-year-old boy with transverse bruise-like marks on his back (Figure 1).
Figure 1

A 15-year-old male first noticed the marks on his back during a recent vertical growth spurt. On exam there are multiple horizontal violaceous linear striae on his back. He is otherwise healthy and denies any history of back injury or exposure to topical or systemic steroids.
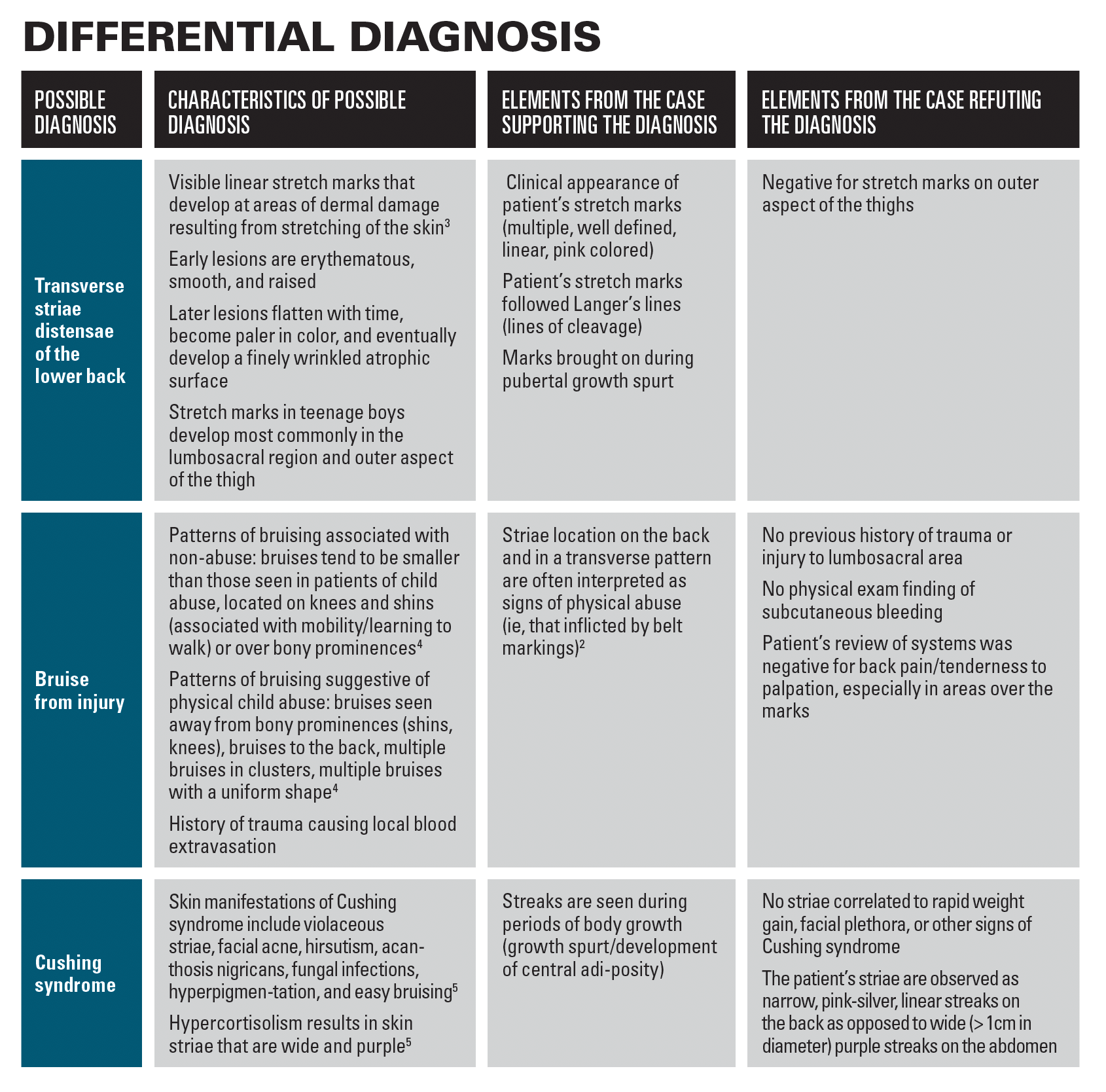
Differential diagnosis for bruises on lower back
The differential diagnosis includes striae distensae in addition to bruising from skin injury. There are various triggers for striae distensae including both topical and oral steroid usage, obesity, excessive marijuana use, and rapid weight gain or loss.1 Another less common cause of striae in adolescents is Cushing syndrome, which is often associated with metabolic weight gain, high blood pressure, and Cushingoid facies.2
Diagnosis: Transverse striae distensae (also known as stretch marks)
Differential diagnosis
Discussion
Striae distensae during adolescence are a common physiological change associated with rapid pubertal growth spurts. These pink-silver thin streaks are seen in up to 35% of girls and 15% of boys between 9–16 years of age.6 In females, the marks commonly occur on the breasts, thighs, shoulders, and buttocks.7 In males, the marks tend to be on the back, thighs, and calves.7 Recent studies on patient demographics have found that striae distensae in adolescents are often associated with tall stature, childhood obesity, and a family history of striae distensae.7,8 These striae initially appear as violaceous, flat plaques called striae rubra that progress over the course of months into permanent pink and hypopigmented scar-like depressions called striae alba.7
Although the exact pathogenesis remains unknown, striae distensae of adolescence result from dermal breaks in connective tissue following physical stress and skin stretching.9 Pubertal growth spurts are a common time for physiologic skin stretching in teenage boys. It is also thought that reduced levels of the genes encoding collagen and fibronectin result in a thinning of the connective tissue and atrophic appearing striae.2 Histological analysis of striae reveals collagen fibers stacked horizontally in straight bundles whereas in normal skin, collagen is arranged randomly into wavy and thick collagen fibers.9
Management
In general, treatment of striae distensae is not necessary in otherwise healthy adolescent males. Lesions often stop progressing at the end of pubertal growth spurts in healthy teenagers who have normal body surface area. Lesions also tend to pale in color and shrink once the growth spurt is complete. Thus, management typically begins with reassurance and patient education of the benign nature of the course. In patients with risk factors for striae distensae, such as obesity with high body mass index (BMI), a healthy diet and exercise regimen is a good place to start for further management.
Although not a necessity in adolescent males with striae likely to improve after puberty, patients interested in improving the cosmetic appearance of striae can opt for initial therapy with 0.1% topical retinoic acid. Laser therapy, more specifically pulse-dye laser, has also been shown to work as initial therapy for inflammatory marks in the striae rubra stage.9 Other interventions including phototherapy, chemical peels, cocoa butter, and vitamin supplements are of limited evidence in the current literature.
Of note, striae located on the lower back are commonly mistaken for bruises from child abuse, as mentioned in the differential diagnosis. Patients are often referred to social services due to this misdiagnosis. This highlights the importance of raising awareness among providers regarding the appearance of these benign striae.
Patient Outcome
This patient was diagnosed with striae distensae based on clinical and physical exam findings. No further lab workup was necessary. We suggested observation of the patient’s back and regular sunscreen use. The patient felt that no further treatment was needed at this time.
References
1. Salter SA, Kimball AB. Striae gravidarum. Clin Dermatol. 2006; 24(2), 97-100. doi:10.1016./j.clindermatol.2005.10.008
2. Elshimy N, Gandhi A. A teenager with lumbar striae distensae (when a bruise is not a bruise). Case Reports. 2013;bcr2013201962. doi:10.1136/bcr-2012-201962
3. Lokhande AJ, Mysore V. Striae distensae treatment review and update. Indian Dermatol Online J. 2019;10(4):380-395. doi:10.4103/idoj.IDOJ¬¬_336_18
4. Maguire S, Mann MK, Sibert J, Kemp A. (2005). Are there patterns of bruising in childhood which are diagnostic or suggestive of abuse? A systematic review. Arch Dis Child. 2005;90(2): 182-186. doi:10.1136/adc.2003.044065
5. Stratakis CA. Skin manifestations of Cushing’s syndrome. Rev Endocr Metab Disord., 2016;17(3), 283-286. doi:10.1007/s11154-016-9399-3
6. Lause M, Kamboj A, Faith EF. Dermatologic manifestations of endocrine disorders. Transl Pediatr. 2017;6(4), 300-312. doi:10.21037/tp.2017.09.08
7. Al‐Himdani S, Ud-Din S, Gilmore S, Bayat A. "Striae distensae: a comprehensive review and evidence‐based evaluation of prophylaxis and treatment." Br J
8. Boozalis E, Grossberg, AL, Puttgen KB, Heath CR, Cohen BA. Demographic characteristics of teenage boys with horizontal striae distensae of the lower back. Pediatr Dermatol. 2018;35(1) (2018): 59-63. doi:10.1111/pde.13329
9. Burk CJ, Pandrangi B, Alvarez Connelly E. Picture of the Month—Quiz Case. Arch Pediatr Adolesc Med. 2008;162(3):277 doi:10.1001/archpediatrics.2007.61-a
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.