Failure to thrive: Early intervention mitigates long-term deficits
Outpatient pediatric providers have an essential role in the ongoing monitoring and care of a child with failure to thrive (FTT). Here’s how routine growth assessments help to identify FTT and determine effective multidisciplinary treatment.
Joyee G Vachani, MD, MED

Figure
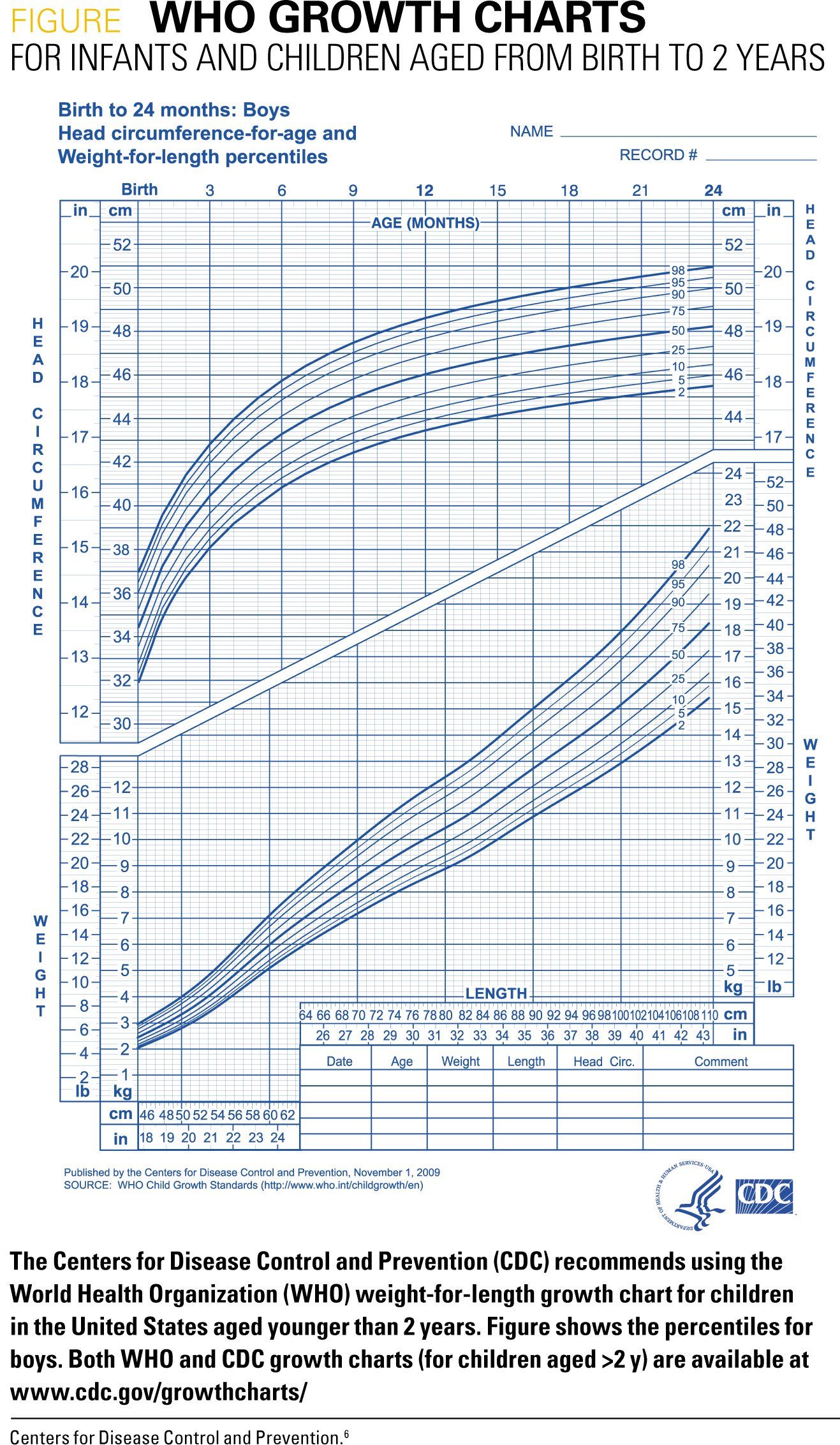
Table 1
ICD-10 codes for failure to thrive
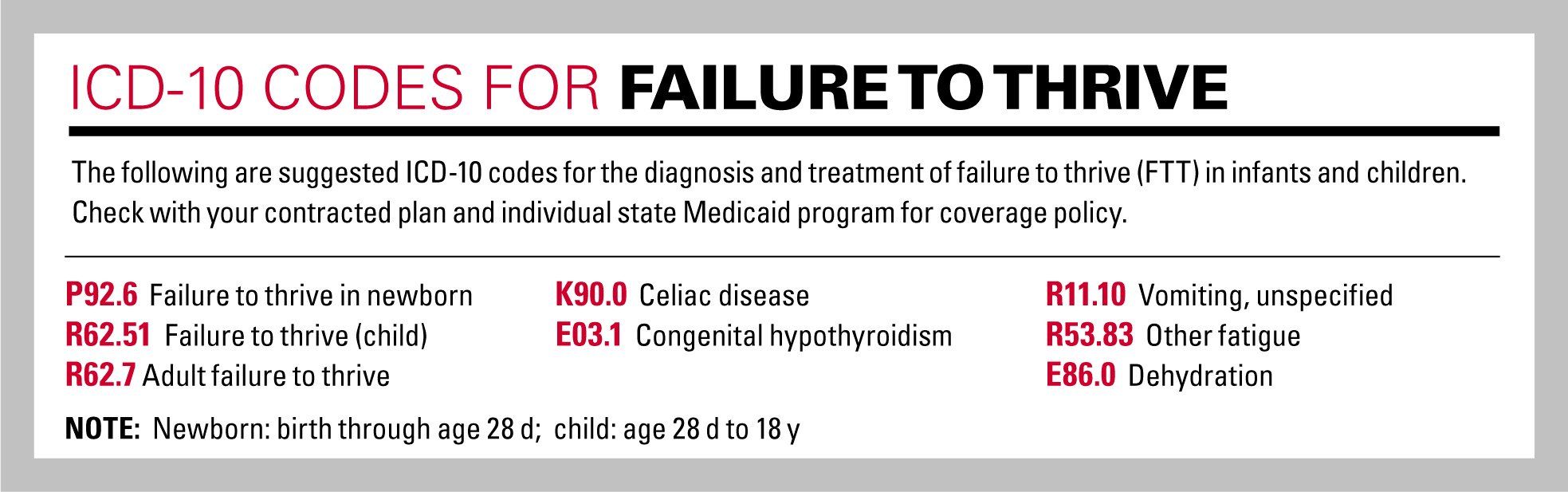
Table 2
The term “failure to thrive “(FTT) first appeared in the literature more than 80 years ago, and although it continues to be widely used, it has no precise definition. Recent terms to describe FTT include undernutrition, malnutrition, and faltered growth. In 2017, guidelines by the National Institute for Healthcare and Excellence in the United Kingdom were published to aid in recognizing, assessing, and monitoring of “faltering growth” in infants and children in the United Kingdom.1 With a lack of any other formal practice recommendations, however, clinical practice is variable, with an overuse of resources, including unnecessary laboratory testing, subspecialist referrals, and hospitalization.2-4
Historically, FTT has been classified as organic and nonorganic, but it is now recognized that only a small minority of children with FTT have an underlying organic cause. Instead, FTT often has a multifactorial etiology involving a complex interaction between medical, nutritional, emotional, and social issues. Although this range of contributing factors can pose a diagnostic challenge, the evaluation and coordination of a management plan for FTT can often be done successfully by providers across the continuum of pediatric care when guided by findings from a detailed history and thorough physical examination.
With a focus on promoting high-value care for patients, this article presents a practical, systematic approach that pediatric providers can use for the differential diagnosis and management of FTT.
Identifying FTT
Failure to thrive has classically been identified when a child’s weight drops off the standardized weight curve before and to a greater extent than the length/height (Figure).5 Its recognition depends on reliable serial measurements for growth assessment. Individuals gathering data must be properly trained and use appropriate equipment with a standardized technique. Stature (length/height) should be measured with the child lying supine on a length board for children aged 0 to 2 years and using a stadiometer for older children. Weight should be determined using a digital scale, and head circumference also should be measured in children aged younger than 3 years.
Data should be recorded and plotted on a standardized growth chart for age and gender or using another appropriate chart when special circumstances exist (eg. premature birth, genetic syndrome). The Centers for Disease Control and Prevention (CDC) recommends using the World Health Organization’s weight-for-length growth chart for children aged younger than 2 years and the CDC body mass index (BMI) growth chart for older children.6
Diagnostic evaluation
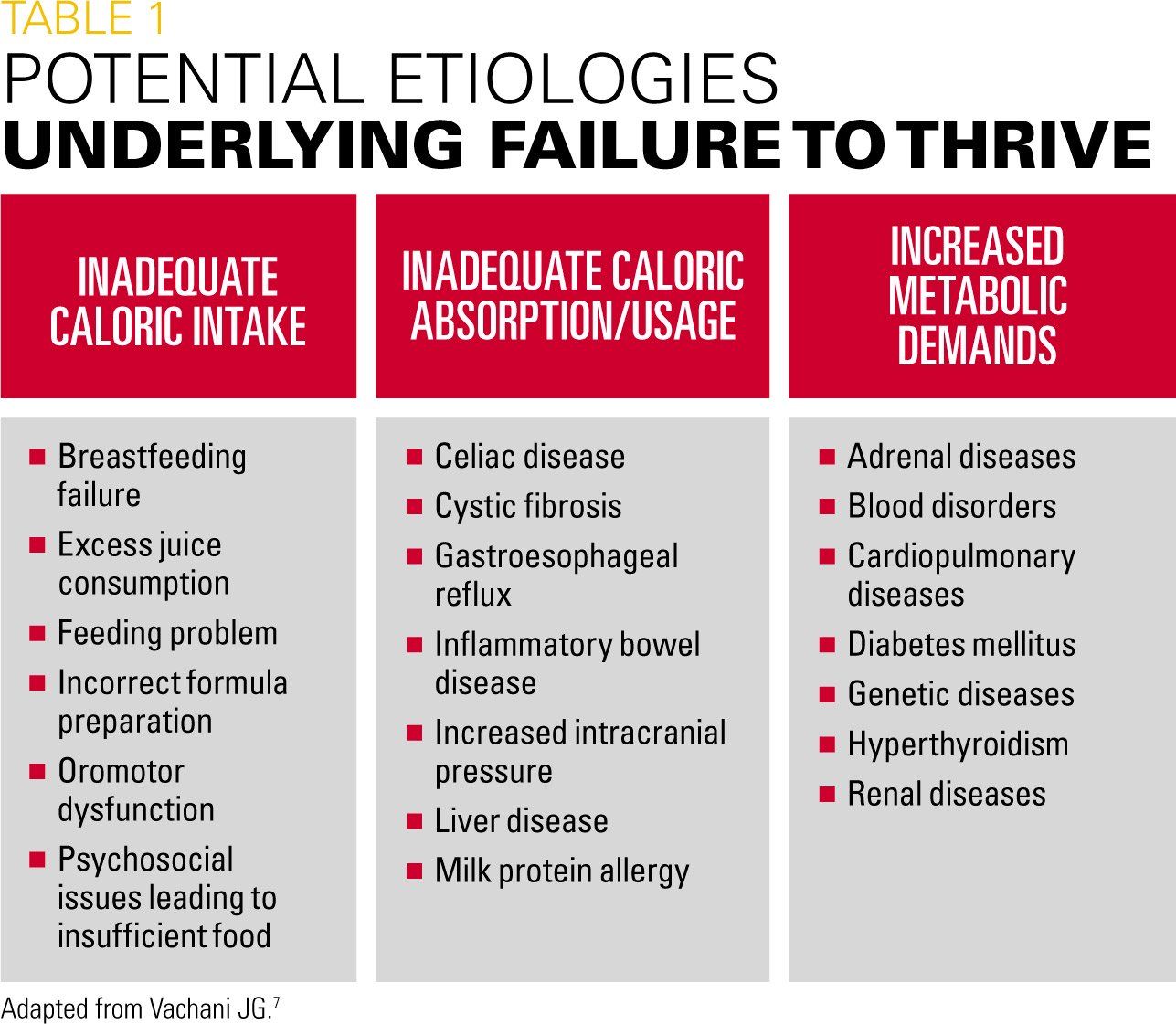
Diagnostic evaluation is key in determining underlying cause(s) for FTT and appropriate management. Pediatric providers should initiate the diagnostic evaluation for FTT by taking a detailed feeding/eating history and performing a clinical, developmental, and social assessment that aims to identify issues that can lead to undernutrition. These etiologies can then be categorized as inadequate caloric intake, inadequate caloric absorption/usage, and/or increased metabolic demands (Table 1).7
History and physical examination
A dietary history may be obtained through a 24-hour recall provided by the parent/caregiver. Whenever possible, providers should enlist the help of a dietitian who can conduct a more formal assessment including calorie counts.
The patient history should identify types of foods and calories consumed along with frequency of meals and snacks. It also should include questions to determine the child’s behavior at feedings/meal times and parental reactions and ideas about nutrition. Some common issues underlying inadequate calories include excessive intake of juice or other beverages that provide poor nutrition and limit appetite for other foods, and improper formula preparation. Mothers who are breastfeeding should be asked about their diet and use of medications, alcohol, or other substances that can affect milk production and let-down.
Psychosocial issues should be investigated to determine if the child is not being provided with adequate food because of neglect/abuse or as a consequence of parental economic, intellectual, or mental health problems.
A good history also can help identify clues of an underlying medical cause for FTT by asking about symptoms of gastrointestinal illnesses-vomiting, reflux, diarrhea, constipation, blood or mucus in the stool; respiratory signs-breathing difficulty, chronic cough, snoring; or recurrent infections. In addition, a thorough family history should be obtained to understand the stature and growth pattern of siblings, parents, and grandparents as well as identifying illnesses such as food allergies, genetic diseases, inflammatory bowel disease, celiac disease, asthma, and cystic fibrosis.The physical examination should include looking for physical impediments to feeding and swallowing, such as cleft lip/palate, oral abscesses, or enlarged tonsils/adenoids; dysmorphic features indicative of a genetic disorder; abdominal distention or organomegaly; neurologic signs of developmental delay; and bruises or other evidence of trauma and abuse. Observation of the parent-child interaction in general and during feeding is also a key part of the physical examination.
Diagnostic testing
Laboratory testing in the workup of a child with FTT only rarely adds useful information unless the assessments are indicated based on the clinical findings.3 If a medical cause is suspected, then testing should be guided by clinical assessment. Examples of targeted studies to consider only when a thorough history and physical suggest a specific diagnosis include transglutaminase antibodies if celiac disease is suspected; a sweat chloride test for cystic fibrosis; stool analysis for suspected malabsorption or infestations; and thyroid function tests for hypothyroidism.
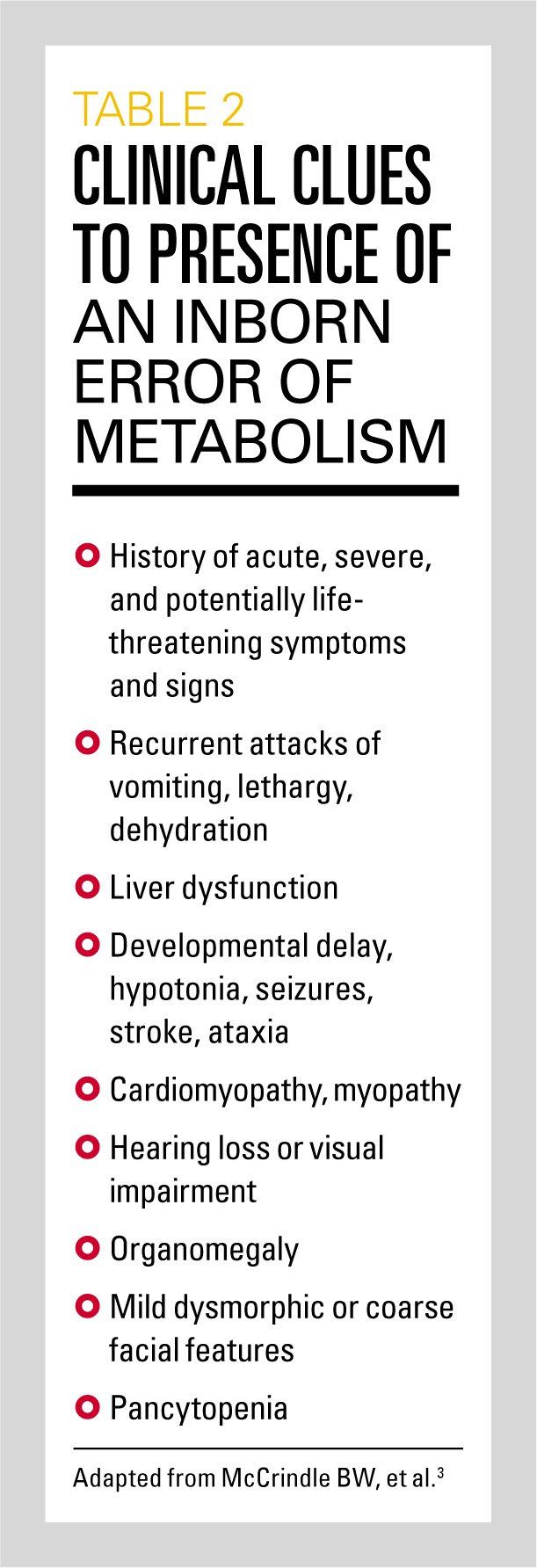
Inborn errors of metabolism are often considered for children with FTT, but it is an unlikely diagnosis in most children with mild-to-moderate FTT.8 Anthropometric criteria for classifying malnutrition in pediatric patients as mild, moderate, or severe were described in a consensus statement from the Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition.9 Before pursuing a more comprehensive investigation for an inborn error of metabolism, clinicians should look for relevant clues in the history and physical (Table 28). If any of these clues are not present, an inborn error of metabolism is less likely.
Management
Management for FTT integrates creation of a nutritional plan and attention to the causes for undernutrition. Ideally multifactorial management includes a multidisciplinary team with a pediatric provider, dietitian, social worker, and other services as indicated.
The nutritional plan targets provision of sufficient calories, protein, and micronutrients, including iron and zinc. The following formula can be used to determine the daily caloric intake (kcal/kg) required for catch-up growth:
Ideal body weight in kg (50th percentile weight/height) X
[kcal/kg/d (Dietary Reference Intake)] current weight (kg)
Strategies for achieving the target weight depend on the child’s age and problems underlying FTT and may involve giving supplementary formula to breastfed infants and seeking lactation support for the mother; supplementation with energy dense formula for formula-fed babies; and dietary fortification with energy-dense foods or nutritional supplements in toddlers and older children.
Ideally, the required nutrition can be provided orally, but tube feeding should be considered if the child is unable to obtain the desired intake through the oral diet alone. Delivery through a nasogastric tube is preferred over a gastrostomy tube unless it is anticipated that the duration will exceed 6 months or if the child is not tolerating the tube feeding after a trial. Decisions on providing continuous versus bolus feeding are individualized.
When a child is very malnourished, caloric intake should be increased gradually as aggressive nourishment can lead to refeeding syndrome, a dangerous complication related to electrolyte and fluid shifts. A child with severe FTT/malnutrition is at risk for refeeding syndrome and should be admitted to the hospital for close clinical monitoring.
Follow-up
Parents should be instructed to keep a log of dietary intake and bring the child in for frequent weight checks to monitor progress. Although it is reasonable to expect that early intervention for FTT should mitigate long-term deficits associated with malnutrition, there is a paucity of longitudinal data in this area and findings from available studies are equivocal. Therefore, follow-up of children with FTT should also include attention to their intellectual and emotional development and referrals as needed to resources that can optimize their outcomes.
Hospitalization
Children with FTT should be admitted to the hospital if outpatient management fails. In addition, hospitalization is indicated when there is concern about abuse; if close observation of the parent-child interaction is deemed necessary; and for children with severe FTT or malnutrition, moderate or severe dehydration or electrolyte disturbances; or serious infection. The inpatient setting allows for coordinated delivery of multidisciplinary care, including appropriate educational counseling and social support services for parents.
When hospitalization is deemed appropriate, significant cost savings may be accrued by avoiding nonurgent weekend admissions. One recent study analyzed data from more than 20,000 children aged younger than 2 years with FTT and calculated that converting one-half of Friday admissions to Monday would save more than $500,000 over a 1-year period.10
Hospitalized children may be discharged once diagnostic testing and consultations are complete and they show consistent weight gain. A plan for continuing care and follow-up also must be in place and parents must demonstrate understanding of the management recommendations.
Summary
The role of the outpatient pediatric provider is fundamental to the ongoing monitoring and care of a child with FTT. Routine growth assessments allow providers to identify FTT, and by using history-taking and physical examination skills alone, providers can often determine its etiology in a timely, cost-effective manner.
Specific diagnostic findings guide the need for further evaluation and appropriate management, and multidisciplinary treatment is often needed as FTT tends to be multifactorial. A standardized approach to care of children with FTT would allow pediatric providers to optimize the care for these patients.
References:
1. National Institute for Health and Care Excellence. Faltering growth: recognition and management of faltering growth in children. NICE guideline. Available at: https://www.nice.org.uk/guidance/ng75/resources/faltering-growth-recognition-and-management-of-faltering-growth-in-children-pdf-1837635907525. Published September 27, 2017. Accessed March 19, 2018.
2. Adedoyin O, Gottlieb B, Frank R, et al. Evaluation of failure to thrive: diagnostic yield of testing for renal tubular acidosis. Pediatrics. 2003;112(6 pt 1):e463.
3. Sills RH. Failure to thrive. Am J Dis Child. 1978;132(10):967-969.
4. Berwick DM, Levy JC, Kleinerman R. Failure to thrive: diagnostic yield of hospitalisation. Arch Dis Child. 1982;57(5):347-351.
5. Al Nofal A, Schwenk WF. Growth failure in children: a symptom or a disease? Nutr Clin Pract. 2013;28(6):651-658.
6. Centers for Disease Control and Prevention. National Center for Health Statistics. Growth charts. Available at: https://www.cdc.gov/growthcharts/. Updated September 9, 2010. Accessed March 19, 2018.
7. Vachani JG. Failure to thrive. In: American Academy of Pediatrics Section on Hospital Medicine; Gershel JC, Rauch DA, eds. Caring for the Hospitalized Child: A Handbook of Inpatient Pediatrics. 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017:569-576.
8. Ficicioglu C, An Haack K. Failure to thrive: when to suspect inborn errors of metabolism. Pediatrics. 2009;124(3):972-979.
9. Becker P, Carney LN, Corkins MR, et al; Academy of Nutrition and Dietetics: American Society for Parenteral and Enteral Nutrition. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). Nutr Clin Pract. 2015;30(1):147-161.
10. Thompson RT, Bennett WE Jr, Finnell SM, Downs SM, Carroll AE. Increased length of stay and costs associated with weekend admissions for failure to thrive. Pediatrics. 2013;131(3):e805-e810.
Artificial intelligence improves congenital heart defect detection on prenatal ultrasounds
January 31st 2025AI-assisted software improves clinicians' detection of congenital heart defects in prenatal ultrasounds, enhancing accuracy, confidence, and speed, according to a study presented at SMFM's Annual Pregnancy Meeting.