How to talk to your teenaged patient about pregnancy and contraception
As teenagers become sexually active, are they fully educated on contraception and pregnancy?
How to talk to your teenaged patient about pregnancy and contraception | Image Credit: © JPC-PROD - © JPC-PROD - stock.adobe.com.

Here is some sobering news: Teenaged mothers are twice as likely to experience postpartum depression (PPD) as adults.1 For this population who are still maturing on a cognitive level and have not yet fully developed their basic coping skills, the impact of PPD can be crippling. Additionally, the stress that a pregnancy adds to this population group can lead to other increased mental health concerns, including severe depression and anxiety.2 Furthermore, parenthood is the leading reason why teenaged girls drop out of school, with more than half of teenaged mothers never graduating from high school.3
Although the national teen pregnancy rates for girls aged 15 to 17 years and 18 to 19 years (the number of pregnancies per 1000 females in the specified age group) have declined almost continuously for the past 30 years,4 the teen birth rate in the United States is still higher than in many developed countries, including Canada and the United Kingdom.5 At the same time, sexual intercourse among adolescents has become the norm: by age 19, approximately 70% of teenagers have had sexual intercourse at least once.6
For these and other reasons surrounding sexual health, initiating discussion of sexual activity, pregnancy, and contraception is a necessity for health care providers. According to the American Academy of Pediatrics (AAP), “Pediatricians [should] spend one-on-one time with adolescents starting at the 11- to 13-year-old checkups. The pediatrician will ask about sexual behaviors and, if indicated, talk with the young person about birth control and ways to prevent sexually transmitted infections [STIs].”7 The question is how to broach issues of pregnancy and contraception with this patient population to produce optimal outcomes.
Initiating the discussion
As the Nike ad says, just do it. Jessica Peck, DNP, APRN, CPNP-PC, CNE, CNL, FAANP, FAAN, clinical professor of nursing at Baylor University Louise Herrington School of Nursing in Dallas, Texas, says to simply start a discussion, honestly and plainly. “Having an established relationship with a primary care provider makes it easier to initiate conversation on both sides. As girls progress into the teen years, it’s important to give anticipatory guidance before any risk-taking behaviors occur.”
Additionally, with the current laws on abortion having changed dramatically, Peck notes, “It is critical to know your state laws and your scope of practice according to your education, training, licensure, and certification, and providers should adhere to those boundaries, referring when necessary.” She adds, “It’s important to emphasize regular well childcare, where questions about reproductive health are easier to ask in the context of health promotion.”
A recent paper published in Frontiers in Pediatrics8 discusses the actions that health care providers can take in the prevention of unplanned pregnancy. Study authors note it is crucial to be “empowering young adolescents to become more aware and capable of making informed decisions about their sexual life, health, and future.”8
The paper cites several factors contributing to adolescent pregnancy, including personal vulnerability, family context, lack of information, poor access to contraception, and religious and cultural background. “Adolescents, especially under the age of 16 or 17 years, lack a long-term vision of the consequences of their behavior and are driven by experimentation and emotions. Therefore, although they cognitively know about contraception and the risk of pregnancy, they may choose to ignore these aspects of their behavior as a kind of denial (‘it cannot happen to me’). This explains why, even in high-income countries with a good coverage of health care needs, some adolescents find themselves pregnant,” the authors state.8
What the discussion should include
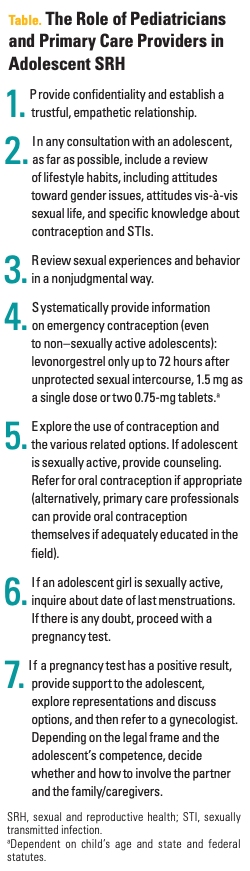
The authors developed several recommendations for health care providers in terms of discussing pregnancy and contraception with their teenaged patients and educating them about it (Table). “Key elements that impact on the quality and effectiveness of service provisions are, among others, easy access to health services, including sexual and reproductive health (SRH); confidential, respectful empathetic care; communication and counseling skills; [and] easy link with specialized colleagues and the community,” the investigators note.8
Birth control recommendations
When it comes to counseling teenagers on methods of birth control, the AAP continues to recommend long-acting reversible contraceptives (LARCs), which include contraceptive implants and intrauterine devices, as the most effective contraceptives to prevent pregnancy. They also recommend that teenagers who use LARCs should also use a condom “or other type of barrier protection during sexual activity to prevent sexually transmitted infections (STIs).”
Additionally, the AAP notes that hormonal contraceptives—combined oral contraception pills, progestin-only contraception pills, patches, injections, and vaginal rings—are more than 90% effective in preventing infection. They recommend use of a condom here as well to prevent STIs.
The progestin-only pill containing norgestrel (Opill) is the first nonprescription birth control approved by the FDA and is now being sold over the counter (OTC).
Finally, should a teenager decide they want to see their pregnancy through and become a parent, the AAP affirms that “all pregnant adolescents should be counseled in a nonjudgmental, developmentally appropriate manner about their full range of pregnancy options.”9
Click here for more from the May issue of Contemporary Pediatrics.
References:
1. Ladores S, Corcoran J. Investigating postpartum depression in the adolescent mother using 3 potential qualitative approaches. Clin Med Insights Pediatr. 2019;13:1179556519884042. doi:10.1177/1179556519884042
2. Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics. 2014;133(1):114-122. doi:10.1542/peds.2013-0927
3. Teen moms. American Society for the Positive Care of Children. 2024. Accessed March 26, 2024. https://americanspcc.org/teen-moms/
4. About teen pregnancy. CDC. November 15, 2021. Accessed March 26, 2024. https://www.cdc.gov/teenpregnancy/about/index.htm
5. About teen pregnancy and childbearing. US Department of Health and Human Services. Accessed March 27, 2024. https://opa.hhs.gov/adolescent-health/reproductive-health-and-teen-pregnancy/about-teen-pregnancy-and-childbearing
6. Lindner J. Sexually Active Teen Statistics: Market Report & Data. Gitnux. Updated December 20, 2023. Accessed March 27, 2024. https://gitnux.org/sexually-active-teen-statistics/
7. Ott MA, Alderman EM. Contraception explained: birth control options for teens & adolescents. HealthyChildren.org. Updated March 8, 2024. Accessed March 26, 2024. https://www.healthychildren.org/English/ages-stages/teen/dating-sex/Pages/Birth-Control-for-Sexually-Active-Teens.aspx
8. Martins MV, Karara N, Dembiński L, et al. Adolescent pregnancy: an important issue for paediatricians and primary care providers-a position paper from the European Academy of Paediatrics. Front Pediatr. 2023;11:1119500. doi:10.3389/fped.2023.1119500
9. American Academy of Pediatrics; Committee on Adolescence. Options counseling for the pregnant adolescent patient. Pediatrics. 2022;150(3):e2022058781. doi:10.1542/peds.2022-058781

Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.