Hypopigmented lesions in a teenaged girl
A healthy 14-year-old girl with a progressive asymptomatic rash on her arms, legs, trunk, and face presents for evaluation. She was treated for eczema with minimal improvement.
Figure 1

Figure 2
The case
A healthy 14-year-old girl with a progressive asymptomatic rash on her arms, legs, trunk, and face presents for evaluation (Figure 1). She was treated for eczema with minimal improvement.
Diagnosis: Hypopigmented fungoides
Etiology, epidemiology, and clinical presentation
Cutaneous lymphomas are a diverse group of neoplasms that develop as an abnormal proliferation of either T- or B-lymphocytes. Mycosis fungoides (MF) is the most common cutaneous T-cell lymphoma (CTCL) and accounts for 54% of cases.1 In adults, hypopigmented MF (HMF) is a rare variant typically presenting in dark-skinned individuals and in those of Asian descent.
Mean age of onset is 55 to 60 years with a slight male predominance.2 Whereas CTCL is rare in the pediatric population, by some estimates representing 0.5% to 5% of total diagnoses, atypical variants predominate.3 In a review of 46 cases of MF presenting before age 16 years, 91% were ultimately diagnosed with the hypopigmented variant.4
Hypopigmented MF presents with hypopigmented macules and patches. Lesions often occur on the head, neck, upper extremities, trunk, and buttocks. Erythema, scale, and papules within these macules and patches are variable. Cases have been reported in both the first and second decades of life. Histopathologically, pediatric HMF typically displays a predominantly T-suppressor CD8+ phenotype, which has a clinically benign course. This is in direct contrast to the CD4+ more clinically aggressive variant of HMF commonly diagnosed in adults.5-7
Differential diagnosis
Diffuse hypopigmentation can occur as a result of a variety of inflammatory diagnoses as well as more rare disease processes. Postinflammatory hypopigmentation is particularly common following eczematous eruptions (eg, contact and atopic dermatitis). History would include an itchy antecedent rash with improvement with therapies including daily moisturizers, topical corticosteroids, and/or calcineurin inhibitors.
Hypopigmentation is the hallmark of pityriasis alba, which manifests as minimally scaly patches on the face of children and likewise responds to eczema regimens. Pityriasis versicolor, pityriasis lichenoides chronica, and disorders of pigmentation such as progressive macular hypomelanosis and vitiligo also may be considered in appropriate clinical scenarios.1,2,5,8,9
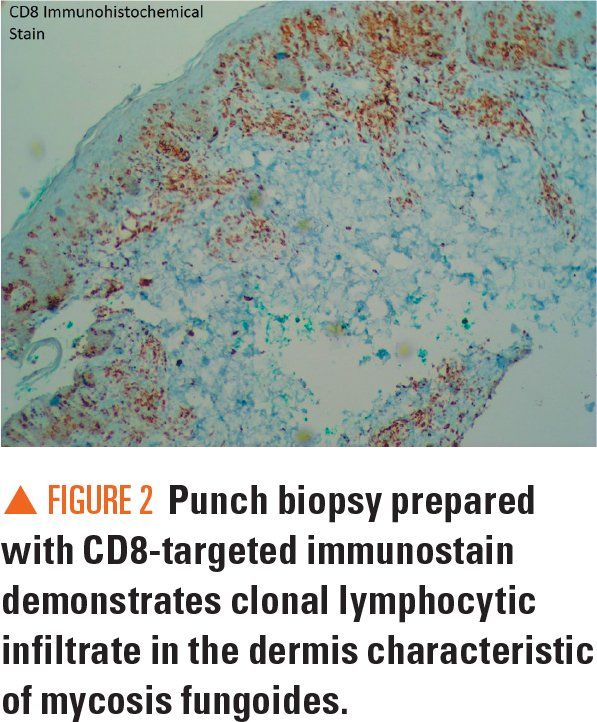
Ultimately, the diagnosis of HMF requires skin biopsy and clinicopathologic correlation. Typical histologic features of HMF include focal parakeratosis, migration of atypical T-lymphocytes into the epidermis (ie, epidermotropism), and a lymphocytic interstitial infiltrate with mild atypia of the papillary dermis. Immunohistochemical stains and T-cell gene rearrangement analyses are typically used to confirm the diagnosis.5-7,10,11 Histopathologic changes can require repeat skin biopsies at follow-up visits to confirm the diagnosis.10,12
Discussion and treatment
Mycosis fungoides is the most commonly diagnosed primary cutaneous lymphoma in children.2 According to the World Health Organization and the European Organization for Research and Treatment of Cancer classification system of primary cutaneous lymphomas, MF is categorized as an indolent lymphoma.5 Pediatric patients with HMF often present with limited cutaneous disease (stage IA or IB), have a good prognosis, and do not experience disease progression for years or even decades.13
Because of low overall incidence and clinical presentations that mimic a variety of benign skin conditions, the diagnosis of pediatric HMF is often delayed. Furthermore, there may be reluctance among physicians to perform skin biopsies on young patients.5 Prompt diagnosis requires an adequate level of clinical suspicion, particularly for those patients with darker skin tones presenting with unusual or progressive hypopigmented lesions, with or without pruritus, that are resistant to standard therapies. Clinical evaluation should then include a lesional skin biopsy.8,14
The most successful treatment modality across multiple series of pediatric patients with HMF has been ultraviolet light therapy, either with narrow band ultraviolet B (nbUVB) or UVA with or without psoralen photosensitization. The nbUVB therapy results in clearance within 2 to 3 years in a majority of patients.4 Other management options include observation, topical corticosteroids, and topical calcineurin inhibitors.
Patient outcome
The patient’s skin biopsy showed a prominent atypical intraepidermal lymphoid infiltrate that was primarily CD8+ on immunohistochemistry stains (Figure 2). Her T-cell gene rearrangement studies were positive for beta and gamma gene rearrangements. Taken together, the clinical presentation and pathology results were diagnostic of CD8+ HMF and nbUVB therapy was recommended. However, the patient lived at a distance and was lost to follow-up.
References:
1. Willemze R. Cutaneous T-cell lymphoma. In: Bolognia JL, Jorizzo JL, Rapini RP, et al. Dermatology. 2nd ed. London: Mosby Elsevier, 2008:1867.
2. Gameiro A, Gouveia M, Tellechea Ã, Morena A. Childhood hypopigmented mycosis fungoides: a commonly delayed diagnosis. BMJ Case Rep. 2014;2014:bcr2014208306.
3. Reiter O, Ben Amitai D, Amitay-Laish I, Israeli M, Pavlovsky L, Hodak E. Pediatric mycosis fungoides: a study of the human leukocyte antigen system among Israeli Jewish patients. Arch Dermatol Res. 2017;309(10):851-856.
4. Heng YK, Koh MJ, Giam YC, Tang MB, Chong WS, Tan SH. Pediatric mycosis fungoides in Singapore: a series of 46 children. Pediatr Dermatol. 2014;31(4):477-482.
5. Patraquim C, Gomes MM, Garcez C, et al. Childhood hypopigmented mycosis fungoides: a rare diagnosis. Case Rep Pediatr. 2016;2016:8564389.
6. Diwan H, Ivan D. CD8-positive mycosis fungoides and primary cutaneous aggressive epidermotropic CD8-positive cytotoxic T-cell lymphoma. J Cutan Pathol. 2009;36(3):390-392.
7. Whittam LR, Calonje E, Orchard G, Fraser-Andrews EA, Woolford A, Russell-Jones R. CD8-positive juvenile onset mycosis fungoides: an immunohistochemical and genotypic analysis of six cases. Br J Dermatol. 2000;143(6):1199-1204.
8. Virmani P, Levin L, Myskowski PL, et al. Clinical outcome and prognosis of young patients with mycosis fungoides. Pediatr Dermatol. 2017;34(5):547-553.
9. Cervini AB, Torres-Huamani AN, Sanchez-La-Rosa C, et al. Mycosis fungoides: experience in a pediatric hospital [article in English, Spanish]. Actas Dermosifiliogr. 2017;108(6):564-570.
10. Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88(6):954-960.
11. El-Shabrawi-Caelen L, Cerroni L, Medeiros LJ, McCalmont TH. Hypopigmented mycosis fungoides: frequent expression of a CD8+ T-cell phenotype. Am J Surg Pathol. 2002;26(4):450-457.
12. Song SX, Willemze R, Swerdlow SH, Kinney MC, Said JW. Mycosis fungoides: report of the 2011 Society for Hematopathology/European Association for Haematopathology workshop. Am J Clin Pathol. 2013;139(4):466-490.
13. Laws PM, Shear NH, Pope E. Childhood mycosis fungoides: experience of 28 patients and response to phototherapy. Pediatr Dermatol. 2014;31(4):459-464.
14. Criscione VD, Weinstock MA. Incidence of cutaneous T-cell lymphoma in the United States, 1973-2002. Arch Dermatol. 2007;143(7)854-859.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.