Pediatric urgent care vs the medical home
To answer the question of which after-hours care is best, pediatric practices and urgent care providers must partner to put children’s welfare first.
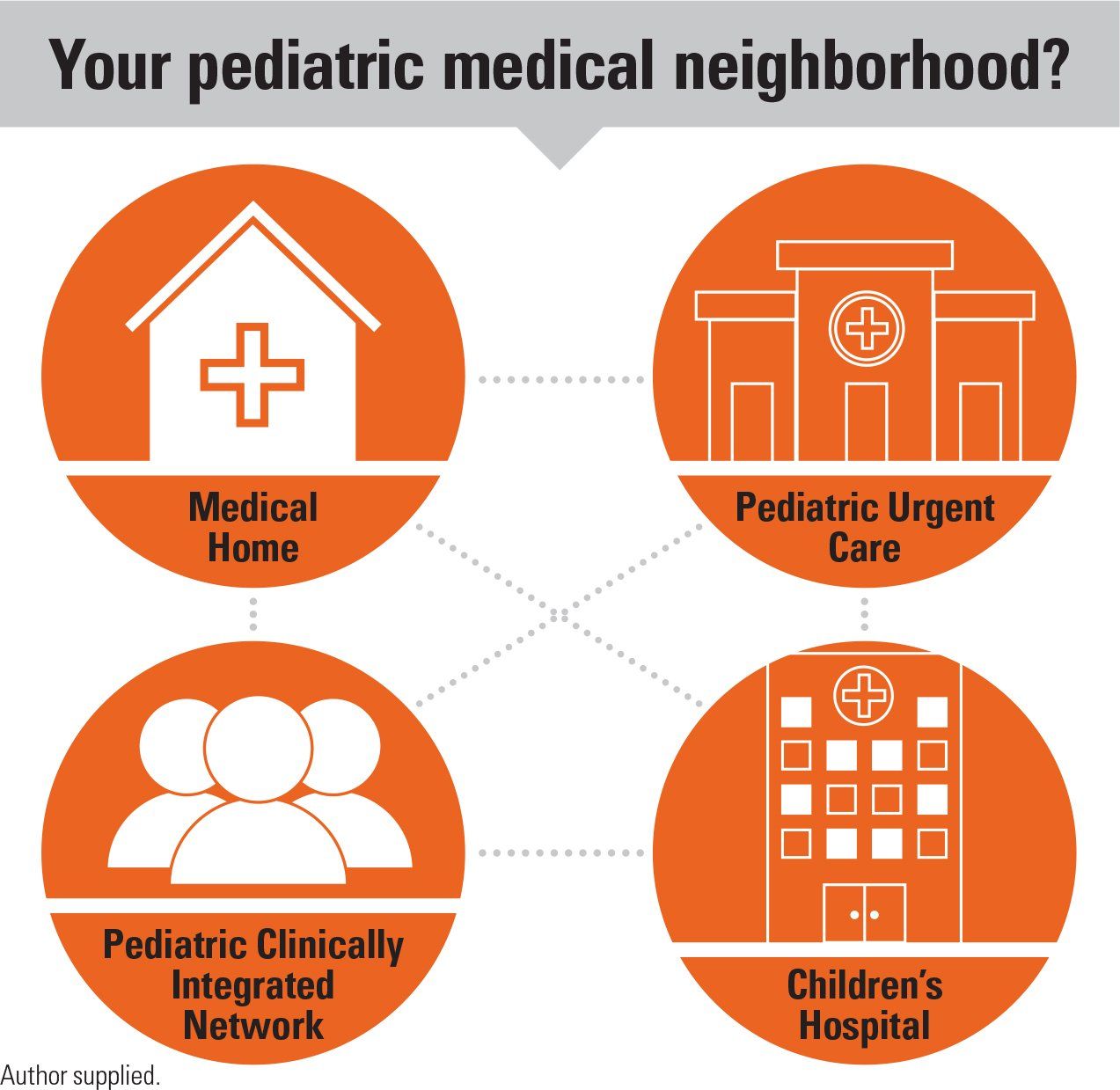
Your pediatric medical neighborhood?
Today’s parents want convenience for everything. The generation often referred to as “millennials” are well connected, intelligent consumers accustomed to finding the most convenient way to limit the stressors in life and offer “uber” efficiency.
For these same parents, access for their child’s healthcare is similar and they will choose convenience first. Faced with even minor barriers to engaging the pediatrician, these parents will often drive to the local urgent care, minute clinic, or even utilize a random provider online via direct-to-consumer telemedicine. Unfortunately, although these offerings are “quick,” their child doesn’t always get the pediatric expertise they need.
Pediatricians around the country commonly share anecdotes of children receiving unnecessary antibiotics or steroids, or cases of a missed, more serious illness. Parents, on the other hand, often struggle to recognize the difference in quality until they must go back to the clinic or to the pediatric urgent care that same evening.
Primary care pediatricians and pediatric urgent cares often believe they are working in competition with each other rather than cooperating. Pediatricians are being financially hurt by the explosion of “convenient” care clinics and rightfully need to be concerned. Pediatric urgent cares, which make up a very small percentage of these offerings, argue that children need after-hours care that is frequently not available from the pediatrician or that millennial parents are demanding this convenience.
Collaborate for services
Ironically, we think all pediatricians would unanimously agree that children should be seen by a trained pediatric provider. Pediatricians generally believe that parents should first choose to reach out to their pediatrician for guidance and, if not available, then seek the care of trained pediatric expertise when needed outside the medical home.1-4
So why don’t we foster greater collaboration across the landscape of pediatrics? What are the keys to supporting the local pediatric network and keeping kids in the medical home or the pediatric medical neighborhood?
Pediatricians must adapt. Phone trees, long delays, front-desk barriers, and lack of after-hours access still limit many practices.5 The millennial parent sees any minor barrier as a major issue when reaching out to the office. These parents seek online or electronic means to reach their physician and often use Dr. Google before they call. Extended hours will help, but more hours must be balanced with physician burnout and overhead cost to the practice.
Asking more and more of your pediatricians may not be the answer. Pediatricians need to explore simplifying answering services, same-day scheduling, and improving triage access and the benefits of virtual care. Telemedicine can offer improved efficiency and access to manage triage, simple visits, and behavioral or developmental follow-up appointments. Access to the trusted pediatrician is vital for the medical home to survive.
Be partners in quality care
Pediatricians must also seek local partners. Demand for immediate care and the need for urgent and emergency care cannot be universally handled by the primary care office. Parents should seek their pediatrician’s advice on where to take their child when office care is unavailable. The guidance of a trusted pediatrician will enable parents to drive past the closest “care” to reach the best pediatric care.
Pediatric urgent cares can and should be a crucial partner for the primary care pediatrician. The urgent care is able to accept referrals, discuss cases, offer advice, provide expert pediatric care, and ensure the medical home receives communication about the care. This is crucial. The same is true of the local pediatric emergency department (ED).
Parents need guidance on when and where to take their child when they are ill or injured. Dr. Google and Alexa are woefully inadequate. Pediatricians have limits to the care they can offer in person, on the phone, or via telemedicine. Pediatric urgent and emergent care should be collaborative.
No pediatrician is eager to see a patient go to a retail clinic or random provider, or refers the family to the Internet to seek care. Collectively, pediatricians must collaborate to meet the needs of parents, children, and the field of pediatrics. We should foster local networks of pediatric care that are built upon cooperation and not competition. Ensuring that children get the best care from a trained pediatric provider will enable us all to meet the mission we embarked upon when we chose pediatrics.
References:
1. Conners GP, Kressly SJ, Perrin JM, et al; Committee on Practice and Ambulatory Medicine, Committee on Pediatric Emergency Medicine, Section on Telehealth Care, Section on Emergency Medicine, Subcommittee on Urgent Care, Task Force on Pediatric Practice Change. Nonemergency acute care: when it’s not the medical home. Pediatrics. 2017;139(5):e20170629.
2. Patient Centered Primary Care Collaborative. Medical neighborhood. Available at: https://www.pcpcc.org/content/medical-neighborhood. Accessed March 5, 2019.
3. Laughlin JJ, Simon GR, Baker C, et al; American Academy of Pediatrics Committee on Practice and Ambulatory Medicine. AAP principles concerning retail-based clinics. Pediatrics. 2014;133(3):e794-e797.
4. Committee on Pediatric Emergency Medicine. Pediatric care recommendations for freestanding urgent care facilities. Pediatrics. 2014;133(5):950-953.
5. Sobo EJ, Seid M, Reyes Gelhard L. Parent-identified barriers to pediatric health care: a process-oriented model. Health Serv Res. 2006;41(1):148-172.