Kisses for Conor
Sudden unexplained death in childhood (SUDC)-it happened to my family.
Dr Bowen and Conor

Dr Bowen, her husband Dave and daughter Tessa

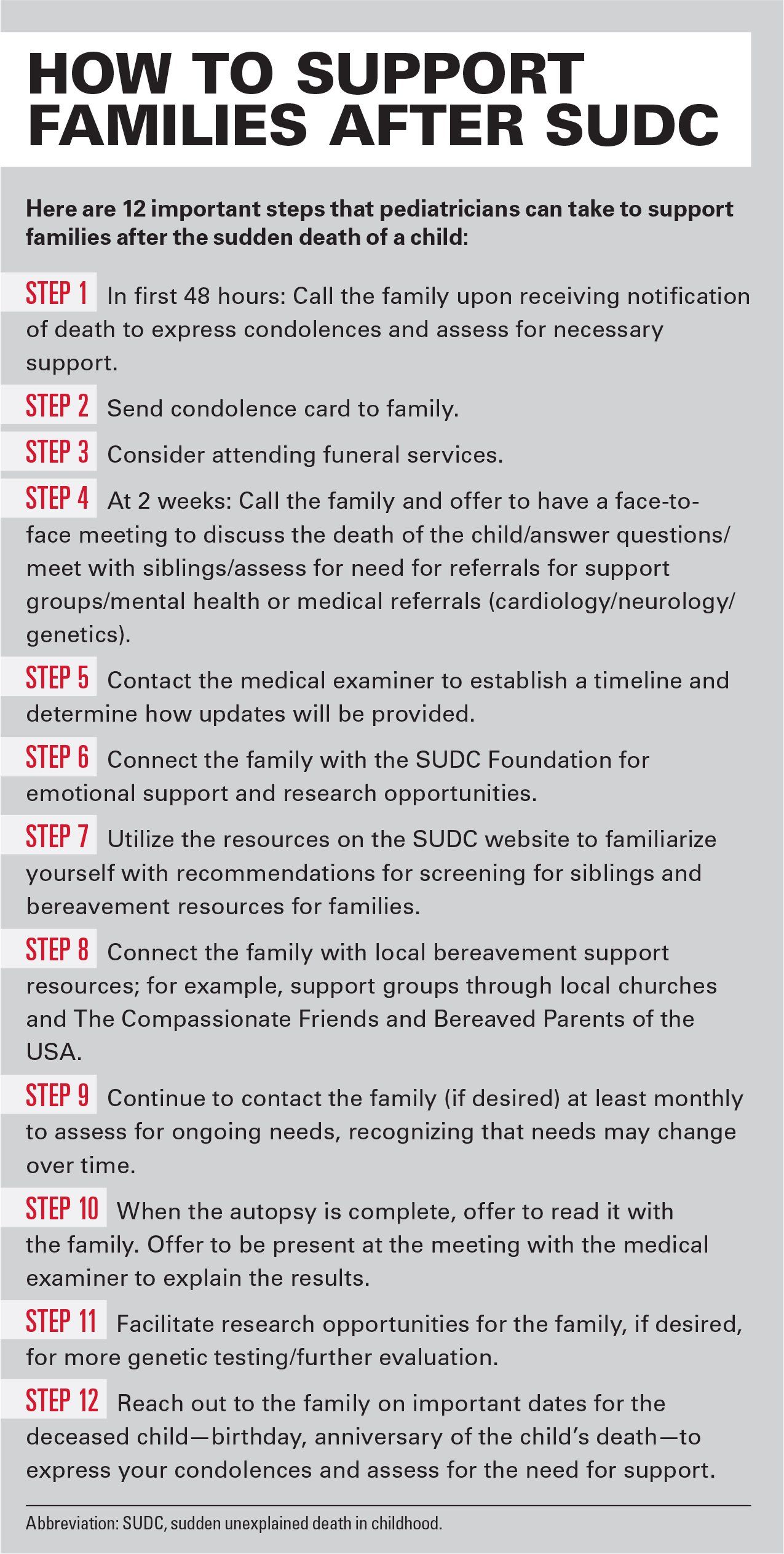
How to support families after SUDC
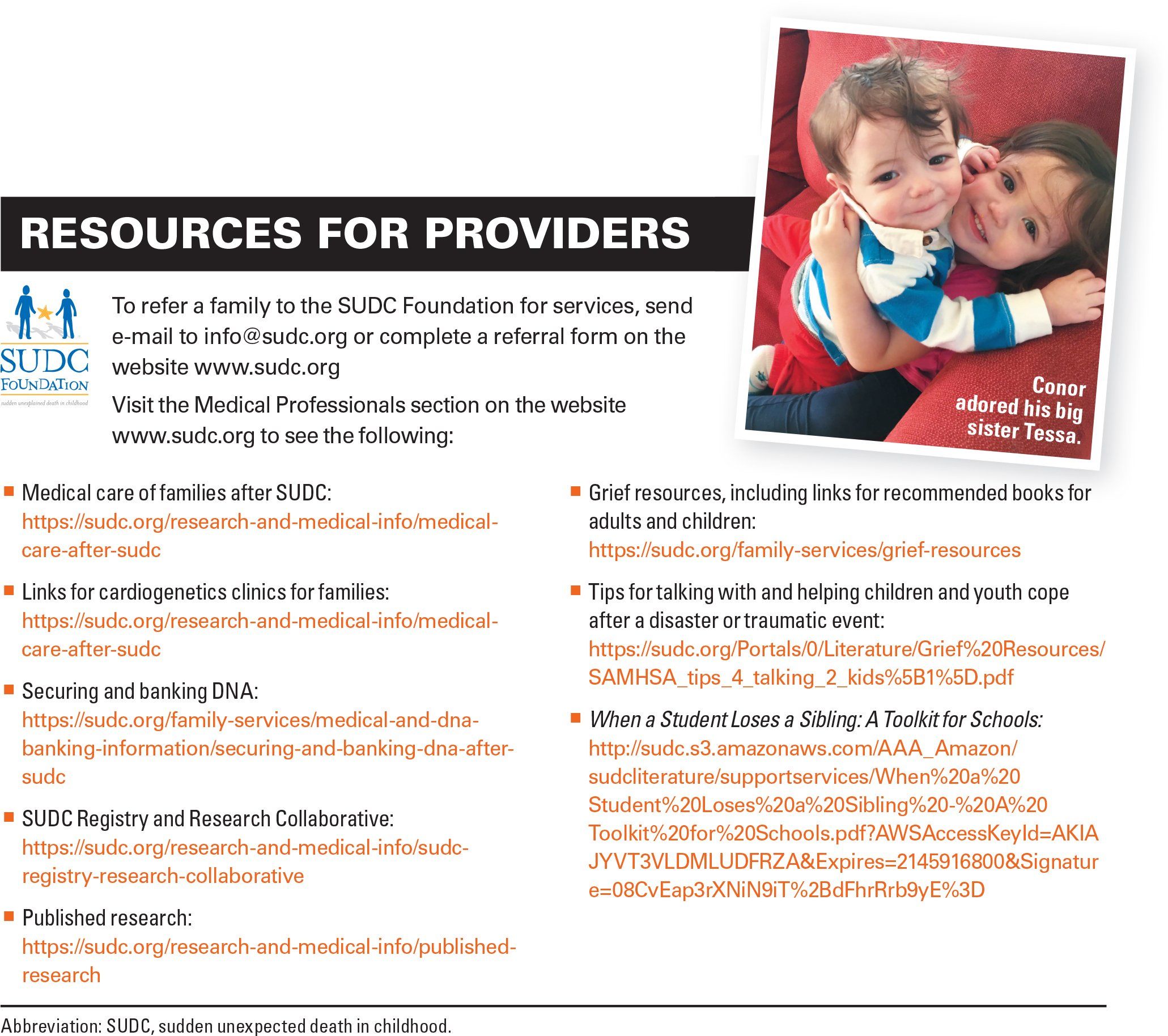
Resources for providers
I am a pediatrician mom. I became a pediatrician before I became a mom, but I have always considered myself a mom first and a pediatrician second. However, the reality is that the 2 are intrinsically linked. This was never more apparent to me than in the last 2 years.
I have 3 children. My daughter Tessa is 4 years old; my daughter Isabelle is 9 months old; and 2 years ago, my healthy, happy son Conor died suddenly and unexpectedly at the age of 17 months. As a mom, my life was shattered. How could I live without my baby? How did my healthy child go to sleep for a nap and just not wake up?
As a pediatrician, the questions continued to build. I felt betrayed by my medical training. I had told parents a million times, “You don’t need to wake your child up. If there’s a problem, they will give you a sign.” In medical school, one of the first things they teach you is the ability to walk into a room and make the determination of sick or not sick. While Conor had a fever the morning he died, he did not look sick.
Our saddest day
On October 25, 2016, Conor woke with a fever of 102°F and a slight runny nose but was otherwise happy and content. I gave him a dose of ibuprofen and fed him his breakfast, which he happily ate while watching Elmo. My husband and I set up our game plan. He would stay with Conor for the morning, bring him to my office around 11:30 so his ears could be checked, and then I would spend the afternoon with him.
When I called my husband to check in at 9:30, Conor was fever free and happily chasing his sister around the living room. My husband put him down for a nap around 10:30, and less than an hour later, when he went to get him ready to go, he was unresponsive. He called 911 and started CPR, but Conor’s heartbeat never returned.
I can remember the exact location I was when I received the call that EMS was taking Conor to the hospital. I can remember the loss of feeling in my body and the feeling that he was gone. I try not to remember how he looked in the emergency department (ED) and the sight of them trying to resuscitate him. What I will always remember is the kindness and compassion of everyone in that ED. They brought us to a separate room where we could spend time with Conor and hold him. Family members were able to come in and hold Conor and say their goodbyes. The ED staff made calls to our churches for us and offered to call family members. They brought us food and water; they held our hands; they cried with us. They made a beautiful memory box with Conor’s handprints, footprints, and a lock of hair. They wrapped him in a blanket and, when it was time to say goodbye, promised that they would take good care of him. Most importantly, they said his name to us when they talked about him.
As we lay that night in shock, the questions kept coming. What could have happened? In the weeks that followed, many of my colleagues speculated about myocarditis or an arrhythmia, but the vast majority said they had never seen anything like this. However, it does occur. We are not the only ones.
According to the Centers for Disease Control and Prevention (CDC), 445 children succumbed to sudden unexplained death in 2016, of which 236 were children aged 1 to 4 years, making it the fifth leading category of death for this age group.1 Yet, it is a topic that is completely lacking in our pediatric curriculum. We learn about sudden infant death syndrome (SIDS), but this is not SIDS. Rather, SUDC is the sudden and unexpected death of a child aged 12 months or older that remains unexplained after a thorough death investigation is concluded.
The SUDC Foundation
We were fortunate to hear about the SUDC Foundation from another family in our town who had undergone a similar loss 9 years before us. Sadly, the majority of the families within the SUDC Foundation are referred through their own research.
There are 800 families within the SUDC Foundation, which is a staggering number. As physicians, we need to know that this nonprofit foundation exists and be able to connect families to it. Becoming a part of the SUDC Foundation meant that my family could receive support from other families who truly understood what we were experiencing. The SUDC Foundation guides families through the emotional trauma, but also helps navigate the process of the autopsy and communication with the medical examiners.
Families within the SUDC community have an opportunity to participate in a research study (SUDC Registry and Research Collaborative), which provides a thorough case review by a multidisciplinary team, neuroimaging, neuropathology and genetic testing (whole exome sequencing) of both parents and the deceased child. These services are provided at no cost to the family. For our family, the lack of knowledge of what happened to Conor also impacted the care of our daughters, Tessa and Isabelle. We did not want to overmedicalize them, but we were unsure what would constitute appropriate follow-up care. Should we see a neurologist or a cardiologist, or both? Should we do genetic testing? The SUDC website has a section on providing care for SUDC families that helps to address these questions and can connect families with providers who specialize in sudden pediatric death.
There has been limited research into SUDC, but there is evidence of an increased rate in febrile seizures among the SUDC population and, similar to SIDS, an increased incidence of death during sleep. However, there are more questions than answers. One major limitation of the current research is the variability in death investigations. In an attempt to standardize the death investigation process, the National Association of Medical Examiners has been involved in a collaboration with the American Academy of Pediatrics to establish national guidelines for the investigation of sudden unexpected pediatric deaths that will be published later this year.
How awareness will help
In order to attain more research and more multidisciplinary collaborations, there needs to be an increased awareness among the medical community, particularly pediatricians, that SUDC is an entity. You may see only one SUDC family in your entire medical career; however, if you can help them navigate this tortuous path, they will remember you forever. As the child’s pediatrician, you are the one they have a connection with, and yet, when your child dies, you are given the phone number of the medical examiner to contact if you would like to discuss your child’s death investigation.
Early communication with the medical examiners can be very useful in order to help provide families with realistic expectations of their timeline. In some states, in the case of a sudden pediatric death, the death investigation can take up to 6 months to be complete. Calls to the medical examiner to seek updates can be important for families but may also feel daunting. Even with my medical knowledge, I dreaded calling the medical examiner to discuss the results of Conor’s autopsy for the simple reason that I would have to say the words, “I’m calling to discuss my son’s death.” I had never read an autopsy before I read Conor’s. Although I had many colleagues offer to read it with me, ultimately it was something I chose to do alone. It is incredibly painful to read about your vibrant, beautiful child in the clinical terms of the autopsy. Providing families with that opportunity for support, regardless of whether they choose it, is very significant.
When your child dies, many hospitals provide the family with a list of bereavement support groups and resources. As I stated before, our ED staff was incredible, but even in the most supportive environments, when your child has just died, any papers that are handed to you feel insignificant at the time. You can’t think. You feel like your entire body is working at 150% capacity just to help you to breathe. After some time has passed, bereavement support can be a lifeline for many families. Pediatricians should be aware of their local resources and should feel comfortable in helping connect families to provide support for both parents and siblings.
Many families feel an outpouring of support in the days and weeks that follow the death of their child, but then feel that, as the months pass, the support fades. You may provide the family with contacts initially, but it may be months before they feel ready to pursue them. Making a call to check in with the family 3 months and 6 months after their child’s death will not be a reminder of the pain of their child’s death. They deal with that pain every second of every day. When you call, it will show them that their child is remembered.
Conor’s legacy
Conor was a beautiful child in every way. He was always smiling and always laughing. You could not help but fall in love with him. He was so full of life and of love. He started blowing kisses at 9 months of age and it quickly became his trademark move. He particularly loved his sister and, despite being the younger sibling, was the first to comfort her if she was upset. Even at his young age, my husband and I used to say we knew he was going to do amazing things. It is so heartbreaking that we will never see him play sports, fall in love, get married, have children, and reach many other milestones, but we know that he can still make a difference in his death.
In memory of his tremendous capacity for love and affinity for blowing kisses, we have been spreading acts of kindness-our “Kisses for Conor” campaign. I was recently named to the Board of Directors of the SUDC Foundation with a commitment to increase medical awareness of SUDC. Currently, the majority of advocacy efforts and funding for the SUDC Foundation comes from affected families. Although it is incredibly inspiring that so many families are turning their tragedies into hope with education and working toward a deeper understanding of SUDC, I believe it is time for the medical community to take a more active role in these efforts.
We cannot ignore the fact that 400 healthy children die every year without any known medical reason, and to date there has been no targeted federal funding to investigate this. My hope is that this article will raise awareness of SUDC, foster future research and collaborations across disciplines, and impel physicians to think ahead about the tools needed to provide adequate support to grieving parents.
To learn more about Conor Bowen and his life and legacy, visit www.kissesforconor.com
References:
1. Sudden Unexplained Death in Childhood (SUDC) Foundation. SUDC Facts/Statistics. Available at: https://sudc.org/sudc-facts/statistics. Accessed October 10, 2018.