Managing genital and pelvic pain in young patients
Part 2 in a series on emergencies in pediatric and adolescent gynecology.
Part 1 of this series on pediatric adolescent gynecologic emergencies focuses on cases about premenarchal bleeding, urethral prolapse, and the cause of a mysterious vaginal discharge. Read more
Monica Woll Rosen, MD, is a clinical assistant professor of obstetrics and gynecology at the University of Michigan Medical School in Ann Arbor. She specializes in pediatric and adolescent gynecology.
Elisabeth H. Quint, MD, is a clinical professor in obstetrics and gynecology at the University of Michigan Medical School in Ann Arbor. She is also fellowship director of the Pediatric and Adolescent Gynecology Fellowship and assistant dean for clinical faculty.
Young patients with gynecologic concerns may present to a general obstetrician-gynecologist as their first local contact. But prior to surgical intervention in a child, consultation with or referral to a pediatric and adolescent gynecologist in an academic medical center may be indicated. This review presents several cases of adolescents with genital and pelvic pain, with guidance for work-up and treatment.
Case 1
You are called to evaluate a 12-year-old girl who fell on the balance beam during a gymnastics class. Her legs landed on either side of the beam. She is unable to void and is in tremendous pain. She was given several doses of pain medication but she continues to experience severe pain (Figure 1). What is your next step?
Figure 1. A 12-year-old girl with vulvar hematoma Credit: Collection of Monica Woll Rosen, MD, University of Michigan

Discussion
This patient has extensive vulvar hematoma. Nonobstetric vulvar hematomas are rare, accounting for only 3.7% of all vulvar hematomas.1They can occur from blunt trauma due to a fall, foreign body insertion, sexual assault, saddle injury, or intercourse. The rich vascular supply from the pudendal vessel branches makes this site vulnerable to hematoma formation.1
A hematoma can be managed conservatively unless the hematoma is expanding, the skin is necrotic, or the patient is in too much pain.2 Ultrasound, CT, or MRI can be used to investigate the size, site, and expansion of the hematoma. Cases requiring surgical management involve an incision, evacuation of blood, and ligation of bleeding vessels.2
Because this patient’s hematoma prohibited her from voiding, she needed a Foley catheter placed. Her urine was evaluated for hematuria. Because of her extensive hematoma and continued pain despite medication, she required an exam under anesthesia to assess the extent of her injury, insertion of the Foley catheter, and incision and drainage of the hematoma.
Case 2
A 13-year-old girl presents to the emergency department with several days of worsening vulvar pain that is now severe. A few days ago, she developed a runny nose, fever, and sore throat. She otherwise has a negative review of systems. She is having trouble urinating because of the vulvar pain and has dysuria when she does urinate. Today she noticed a thick, yellow discharge in her underwear. On exam you notice several large painful ulcerations (Figure 2). What is the next step?
Aphthous or Lipshütz ulcers. Credit: Collection of Monica Woll Rosen, MD, University of Michigan

Discussion
Aphthous or Lipschütz ulcers are acute vulvar ulcers that occur mainly in non–sexually active girls and are thought to be viral in nature.3 They commonly appear during or following a prodromal viral illness.1 Although Epstein-Barr virus4 and cytomegalovirus5 have been associated with the ulcers, the causative virus often cannot be identified. There have been recent case reports of vulvar ulcers following a COVID-19 infection6 or after receiving the COVID-19 vaccine.7
A patient may have black, necrotic, shallow, or deep ulcers in the labia minora or majora.3 There can be overlying purulent discharge. When assessing any ulcers it is important to evaluate for underlying sexually transmitted infections, such as herpes simplex. Other considerations include Crohn disease with multiple tracks and ulceration or Behçet disease, which presents with recurrent vulvar ulcers in conjunction with recurring oral ulcers.3
Treatment for aphthous ulcers is supportive, as it is a self-limiting condition. Topical lidocaine gel can be used for pain control, and a topical clobetasol ointment can be used twice daily.8,9
If a patient is severely affected, an oral steroid taper may be considered, as well as an admission for intravenous pain control. If the patient cannot void because of dysuria, a Foley catheter should be placed.
Case 3
An 11-year-old girl presents after track practice with severe, unilateral right lower quadrant pain. Her last menstrual period was 3 weeks ago. The pain is sharp and radiates to her back. She has associated nausea and vomiting. On exam, she has rebound tenderness and guarding of her lower abdomen. On a pelvic ultrasound, she has a 6-cm simple cyst and a normal appendix. What do you do next?
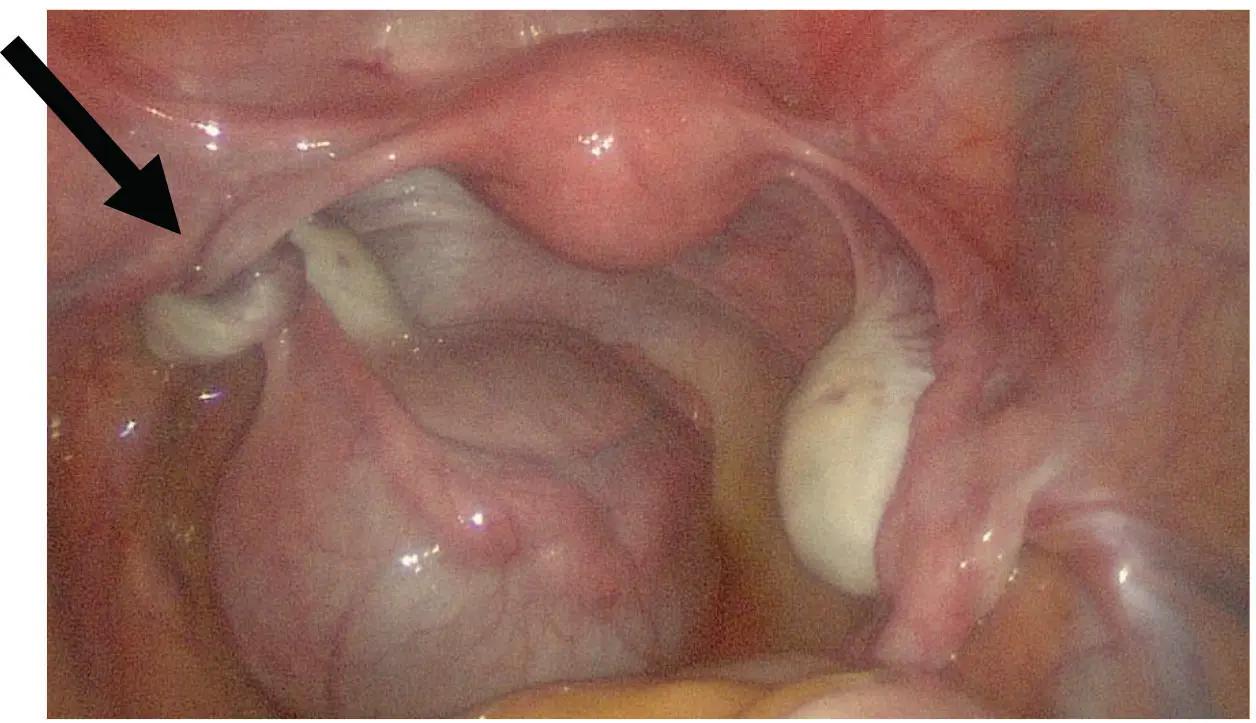
Figure 3. Ovarian torsion Arrow shows torsed infundibulopelvic ligament.
Credit: Collection of Monica Woll Rosen, MD, University
of Michigan
Discussion
This patient most likely is experiencing ovarian and/or tubal torsion (Figure 3). Ovarian torsion accounts for 2.7% of gynecologic emergencies.10 It occurs when the ovary twists on its attachments, which causes decreased blood flow and eventually leads to necrosis. Ovarian and paraovarian cysts, increased length of ovarian ligaments, and enlarged ovaries are risk factors for this condition. A patient is typically evaluated with an ultrasound to assess for a mass and blood flow to the ovary.
Ovarian torsion can be difficult to diagnose preoperatively—the differential includes appendicitis, hemorrhagic cyst, ovarian rupture, and other bowel etiologies. Absent Doppler flow to the ovary suggests torsion, but torsion may be present even with normal flow.
A recent study of 87 girls with suspected ovarian torsion found that a preoperative diagnosis was confirmed in 48% of postmenarchal patients.11 Treatment involves detorsion of the ovary when possible and cystectomy to prevent recurrence.12 There is limited indication for oophorectomy. Detorsion with cystectomy can almost always be done, regardless of ovarian size. There is insufficient evidence to dictate oophoropexy, although this may be considered, particularly in the case of recurrent torsion.
Case 4
A 14-year-old girl presents to the emergency department with significant abdominal pain. She is premenarchal but has had pelvic cramping for the past 6 to 9 months. She has Tanner stage V breasts and genitalia. On pelvic exam, there is a bulging hymen with a blue hue (Figure 4).
On rectal exam, there is a large anterior bulge immediately inside her rectal opening. On ultrasound, you see a large mass and have difficulty distinguishing the uterus or ovaries. What is your diagnosis?
Figure 4. Imperforate hymen

Discussion
This presentation and exam are consistent with an imperforate hymen, which occurs in 0.05% to 0.1% of girls.13 Abdominal pain at the time of expected menarche is the most common presenting symptom of this condition (54.2%), followed by urinary retention (20.3%) and dysuria (9.7%).14
Of note, this condition can and should potentially be diagnosed in the neonatal nursery, as maternal estrogen allows easy visualization of the vaginal introitus. If the neonate is asymptomatic and voiding without difficulty, surgical management can be deferred until puberty.
More typical is a missed diagnosis until after menarche. Surgical incision of the hymen is then indicated to relieve the backup of menstrual blood.
Traditionally, this procedure was performed using a cruciate incision, but many providers now use a circular incision to open the hymen. It is important to suture with interrupted stitches so as not to constrict the hymen. This heals very well and should not recur or cause stenosis. No postoperative dilation is needed. Hormonal suppression of menses may be considered until surgery can be performed. This condition, although urgent, is not emergent, particularly if the diagnosis is in question.
Caveat: Vaginal agenesis also can present with primary amenorrhea and occasional pain due to obstructed uterine remnants. However, there will usually be some hymenal remnants visible on exam and no bulge will be felt on rectal examination. Further imaging with ultrasound followed by MRI is the next step in distinguishing this condition. Other rare obstructing anomalies include a transverse vaginal septum or cervical agenesis.
Case 5
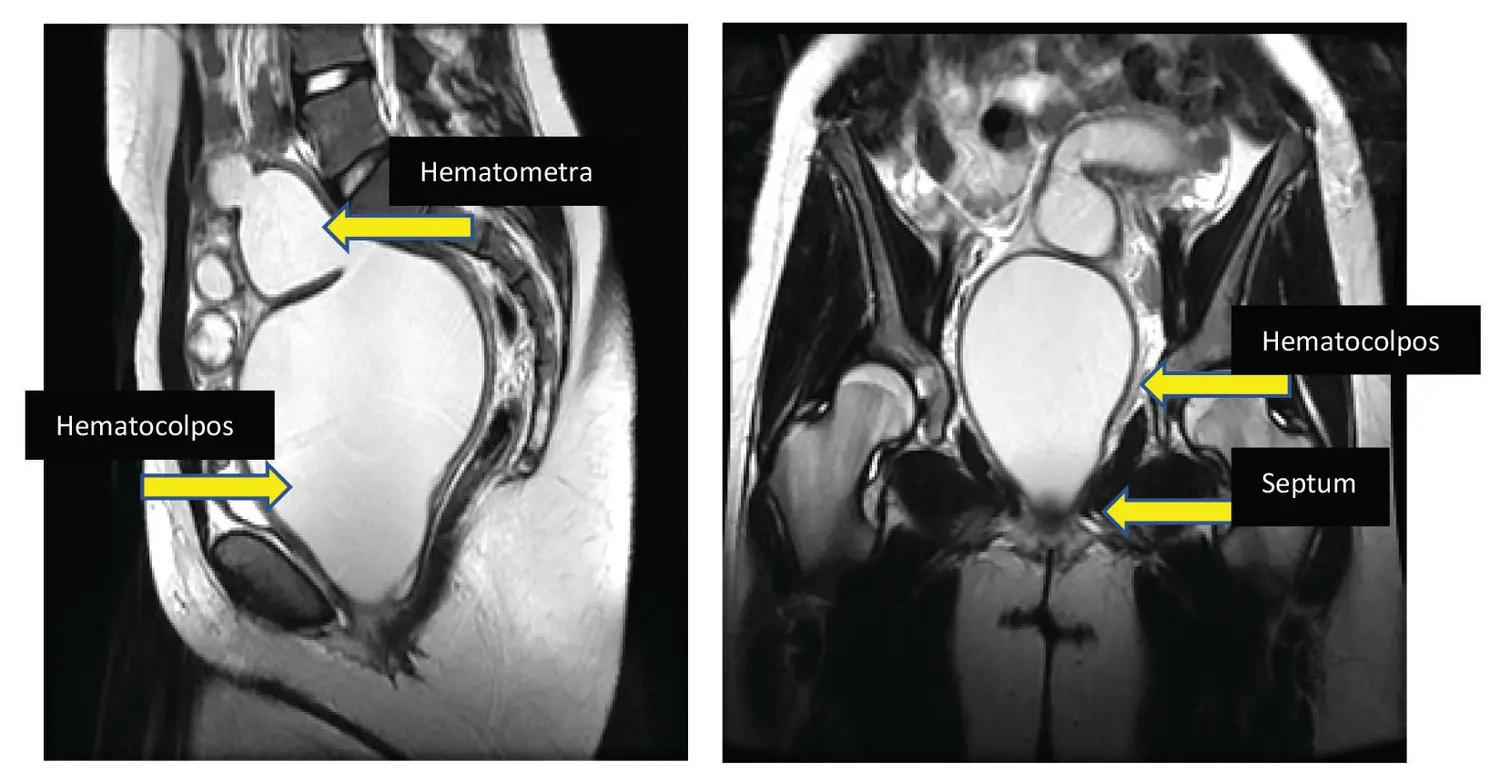
A 13-year-old girl presents with significant cyclical abdominal pain and amenorrhea. She has Tanner stage V breasts and genitalia. Her external genital exam is completely normal with an appropriate hymenal opening. There is no bulge on the perineum. A small cotton swab placed through the hymen stops at 4 cm. On rectal exam you feel a bulge anteriorly, approximately 4 cm into the rectal canal. Ultrasound reveals a large blood-filled cavity, so you obtain an MRI (Figure 5). What is your diagnosis?
Figure 5. MRI of a 13-year-old girl with transverse vaginal septum. Credit: Collection of Monica Woll Rosen, MD, University of Michigan
Discussion
This scenario is most consistent with a transverse vaginal septum. The septum can be located at different levels of the vagina, but external genitalia appear normal. Septa can vary in thickness, with whole segments of the vagina undeveloped.
Because cases of transverse septa are rare and difficult to repair, they should be managed at tertiary centers by experienced pediatric and adolescent gynecologists or other gynecological surgeons.
Surgery is usually performed vaginally, with assistance abdominally or laparoscopically. Surgery involves resection of the septum, which relieves the obstruction, followed by either a simple pull-through vaginoplasty or by using a skin or buccal graft to cover the defect.15
It is imperative that patients perform patient-led vaginal dilation after surgery. A recent study showed that of 21 patients who underwent transverse septum resections and had a postoperative complication of vaginal stenosis or scarring, 14 (56%) either did not dilate afterward or did not dilate correctly.14 Therefore, when a transverse septum is diagnosed, menstrual suppression is usually initiated until a patient is old enough to dilate on her own.
Conclusion
The cases above outline gynecological situations and emergencies that are unique to children and adolescents. Pediatric patients may need an exam under anesthesia to thoroughly evaluate anatomy or vaginal complaints. When uncertainties exist, and especially prior to surgical intervention in a child, consider consulting with a gynecologist experienced in pediatric and
adolescent gynecology.15
Originally published on our sister brand, Contemporary OB/GYN.
References:
1. Burnham A, Cooke-Barber J, Thacker S, Evans D, Carney D, Boswell W. Non-obstetric vulvar/paravaginal hematoma in an adolescent female with scleroderma: an opportunity for intimate partner violence intervention. HCA Healthcare Journal of Medicine. 2020;1(4):211-215. doi:10.36518/2689-0216.1043
2. Kim MS, Lee HJ, Joo E, Kang S, Lee MH, Kim HC. Management of non-obstetric traumatic vulvar haematoma: a retrospective review of 33 cases. J Obstet Gynaecol. 2021:1-4. doi:10.1080/01443615.2021.1960289
3. Vismara SA, Lava SAG, Kottanattu L, et al. Lipschütz’s acute vulvar ulcer: a systematic review. Eur J Pediatr. 2020;179(10):1559-1567. doi:10.1007/s00431-020-03647-y
4. Lorenzo CV, Robertson WS. Genital ulcerations as presenting symptom of infectious mononucleosis. J Am Board Fam Pract. 2005;18(1):67-68. doi:10.3122/jabfm.18.1.67
5. Martin JM, Godoy R, Calduch L, Villalon G, Jordá E. Lipschütz acute vulval ulcers associated with primary cytomegalovirus infection. Pediatr Dermatol. 2008;25(1):113-115. doi:10.1111/j.1525-1470.2007.00597.x
6. Krapf JM, Casey RK, Goldstein AT. Reactive non-sexually related acute genital ulcers associated with COVID-19. BMJ Case Rep. 2021;14(5):e242653. doi:10.1136/bcr-2021-242653
7. Wojcicki AV, O’Flynn, O’Brien KL. Vulvar aphthous ulcer in an adolescent after Pfizer-BioNTech (BNT162b2) COVID-19 vaccination. J Pediatr Adolesc Gynecol. 2022;35(2):167-170. doi:10.1016/j.jpag.2021.10.005
8. Rosman IS, Berk DR, Bayliss SJ, White AJ, Merritt DF. Acute genital ulcers in nonsexually active young girls: case series, review of the literature, and evaluation and management recommendations. Pediatr Dermatol. 2012;29(2):147-153. doi:10.1111/j.1525-1470.2011.01589.x
9. Bandow GD. Diagnosis and management of vulvar ulcers. Dermatol Clin. 2010;28(4):753-763. doi:10.1016/j.det.2010.08.008
10. Childress KJ, Dietrich JE. Pediatric ovarian torsion. Surg Clin North Am. 2017;97(1):209-221. doi:10.1016/j.suc.2016.08.008
11. Melcer Y, Maymon R, Pekar-Zlotin M, Pansky M, Smorgick N. Clinical and sonographic predictors of adnexal torsion in pediatric and adolescent patients. J Pediatr Surg. 2018;53(7):1396-1398. doi:10.1016/j.jpedsurg.2017.07.011
12. Dasgupta R, Renaud E, Goldin AB, et al. Ovarian torsion in pediatric and adolescent patients: a systematic review. J Pediatr Surg. 2018;53(7):1387-1391. doi:10.1016/j.jpedsurg.2017.10.053
13. Lee KH, Hong JS, Jung HJ, et al. Imperforate hymen: a comprehensive systematic review. J Clin Med. 2019;8(1):56. doi:10.3390/jcm8010056
14. Brander EPA, Vincent S, McQuillan SK. Transverse vaginal septum resection: technique, timing, and the utility of dilation. A scoping review of the literature. J Pediatr Adolesc Gynecol. 2022;35(1):65-72. doi:10.1016/j.jpag.2021.09.002
15. Wancura M, McCracken JM, Steen E, Cosgriff-Hernandez E, Keswani S, Hakim JCE. Emerging technologies in pediatric gynecology: new paradigms in women’s health care. Curr Opin Obstet Gynecol. 2019;31(5):309-316. doi:10.1097/GCO.0000000000000563
Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.
Meet the Board: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI
May 20th 2022Contemporary Pediatrics sat down with one of our newest editorial advisory board members: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI to discuss what led to her career in medicine and what she thinks the future holds for pediatrics.
Artificial intelligence improves congenital heart defect detection on prenatal ultrasounds
January 31st 2025AI-assisted software improves clinicians' detection of congenital heart defects in prenatal ultrasounds, enhancing accuracy, confidence, and speed, according to a study presented at SMFM's Annual Pregnancy Meeting.