Mental health is a part of checkups
Experts highlight the importance of mental health screening at well-child visits.
Mental health is a part of checkups | Image Credit: © LIGHTFIELD STUDIOS - © LIGHTFIELD STUDIOS - stock.adobe.com.

Background and magnitude of mental health problems
Because of their longitudinal relationships with children and families, pediatricians have the opportunity to ask and learn about the mental and emotional health of a child from infancy through childhood and adolescence. The pediatrician can partner with the child and family for promotion, prevention, early identification, and intervention when indicated.
The spectrum of mental health concerns in pediatrics is broad. Nineteen percent of children and adolescents in the United States have impaired mental health functioning and do not meet criteria for a disorder. Thirteen percent of school-age children and 10% of children in preschool with normal functioning have parents with concerns. Approximately 20% of children and adolescents have a mental health disorder. The whole range, from concerns to functional issues to mental health disorders, is seen in pediatric practice. 1-3
Of the children and youth who do have a mental health disorder, only approximately 20% receive care. The mental health system focuses on those with severe impairment, in which there is little support for prevention or services to children with emerging or mild/moderate conditions. Child mental health workforce shortages are significant. All these are forces are leading families to seek help in primary care.
The COVID-19 pandemic highlighted a mental health crisis for children and adolescents that had been worsening prior to the pandemic. Suicide has been the leading cause of death for 10- to 24-year-olds since before the pandemic. Factors affecting children and adolescents include disruption of childcare/school, social isolation, loss of peer interactions, loss and grief, and parental/caregiver stress and well-being.4
Responding to mental health concerns in primary care settings
To respond to this crisis, the American Academy of Pediatrics (AAP) has developed the Mental Health Competencies for Pediatric Practice with 2 categories: clinical skills and practice enhancements.1,5 To implement mental health screening effectively, the competencies are essential. Incorporating these competencies into practice enables pediatricians to eliminate the false dichotomy of physical health and mental health in routine care, and to be able to support healthy mental and emotional development, identify concerns early, and partner in interventions. These competencies deserve emphasis during residency training and can be developed further through continuing medical education and lifelong learning.
Clinical skills include:
Promotion and primary prevention. Promote healthy lifestyles and stress management by taking a routine, age-appropriate psychosocial history.
Secondary prevention. Identify and evaluate risk factors and emerging symptoms by using appropriate tools for screening and conducting referral/linkage to community resources.
Assessment. Recognize mental health emergencies/severe impairments that need urgent specialty care by interpreting screening results for brief intervention and assessing need for full diagnostic evaluations. Diagnose children and adolescents with common conditions such as attention-deficit/hyperactivity disorder, anxiety disorders, depression, and substance use.
Treatment. Develop fundamental communication skills (common factors) by using common elements to initiate care. Develop a care plan with the medical home team or in collaboration with mental health specialists, and achieve proficiency in selecting, prescribing, and monitoring appropriate medications for use in pediatric care. Develop crisis and safety plans by making warm hand offs and comanaging patients.
Practice enhancements include:
Developing more collaborative and consultative relationships. For example, identifying a psychiatrist and developmental-behavioral pediatrician to consult with may be beneficial.
Shifting the practice team culture. Encourage staff to embrace mental health care as integral to pediatric practice and enable all staff to understand the impact of trauma on child well-being.
Developing enhanced systems. This includes cultivating a broad environment of respect, agency, confidentiality, safety, and trauma- and resilience-informed care. Systems of care should involve preparing to identify and manage suicide risk and mental health emergencies. This can be done through use of a registry, protocols, and tracking for those with positive psychosocial assessments. Additional strategies to develop enhanced systems include standardized communication for comanagement and coding and billing tools.
Conducting regular data analysis for practice improvement.
Setting the stage to address mental health effectively
Mental and emotional development is influenced by factors that include social drivers of health (eg, food and housing security, community environment, structural racism), caregiver well-being and mental health, and the child’s social and emotional development. To enable families to engage in addressing mental health, it is often necessary to ensure that basic needs are met first through linkage to resources.
Every family has strengths and risks that can affect health. These are part of the interaction in every encounter with the primary care clinician (PCC), whether they are intentionally elicited or not. In practice, the emergence of social/emotional concerns as the visit is ending is a major pain point, often leading to a rushed and inadequate response and disruption of the schedule. Integrating social/emotional screening at the beginning of the visit as part of routine care proactively considers strengths and concerns and enhances visit satisfaction for both the family and the PCC.
Bright Futures has long recommended eliciting family strengths and risks at each visit. Screening has value for promotion, prevention, and early identification. There is also a recommendation for behavioral/social/emotional screening, which is expedited by previsit completion and review of the screen.6 The recommendation is to use age-appropriate validated tools for mental health and functioning, and to use validated questions to ask about social drivers of health (eg, household, family-social well-being, parent-personal well-being, and parent-child relationship).
Screening for mental health problems using validated tools
Screening is always followed by discussion and engagement with the patient and family (observing adolescent confidentiality), as well as collaboration on a plan of care if a concern is identified. Discussion of screening and next steps is an opportunity to elicit and reinforce strengths and protective factors and continue building relationships with caregivers. If a screen demonstrates a concern, a secondary/targeted screen may be indicated.7
Selection of age-appropriate screening tools is best achieved by review and decision-making by the practice team. Questions to consider include: What can the tool tell us? What do we want to know for each age range? What do we not want to be surprised by? Practical questions include: Is the tool conducive to use in clinic flow? What is the length of the tool? Is the tool available in the languages of the communities who come to our practice?
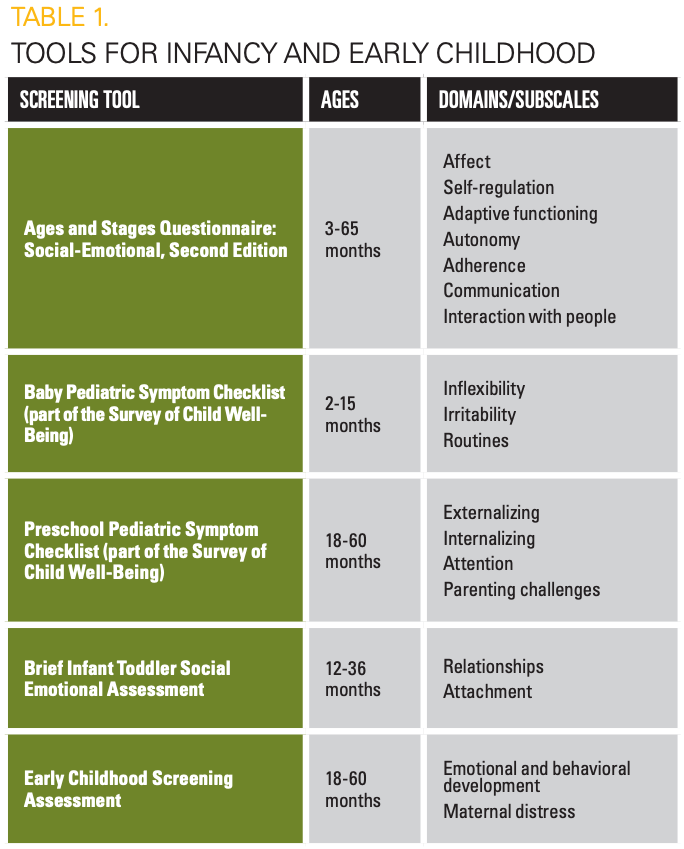
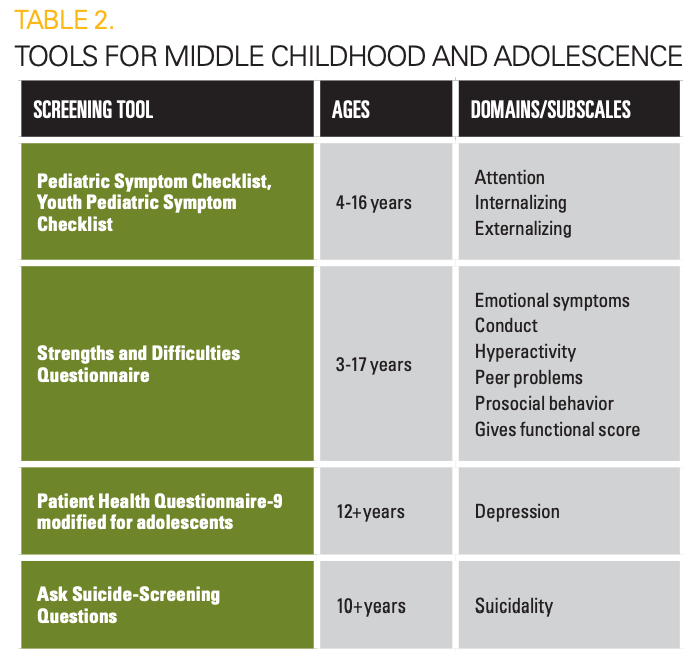
Validated tools with scoring criteria to assess social and emotional well-being have been used successfully in primary care and are listed in Tables 1 and 2.
Engaging staff and families in mental health screening
Another important step for the practice team is to develop a script for how the tool will be introduced to the family/patient. Familiarity with the use of this script is important for both front office and clinical staff. The goal is to use a standardized, respectful, culturally appropriate message about the reason for screening, and to share effective ways to open the conversation with a family. Engaging families in the screening includes indicating that these questions are asked of all patients and families in recognition of their being an integral part of health. Having a script assists with the comfort of staff who introduce the screens and communicates the practice’s openness to discussion of concerns that families may have.
A screening completed and reviewed by the PCC prior to entering the exam room can help focus the visit and serve as a template for discussion based on the family’s priorities. This results in the visit being more efficient and valuable for the family. It is important to acknowledge completion of the screen and discuss responses, even if the screen does not have an at-risk score. The conversation is an opportunity to engage both the family and the patient, and to build trust.
Each practice may want to consider the best method of administering screenings to their own patient population. Some practices find that sending electronic questionnaires before the visit is efficient and appreciated by parents, whereas other practices administer screenings on electronic tablets after arrival at the office or use paper versions and clipboards. Having screenings available in multiple languages and having interpreters available to review them is important for many patient populations. Occasionally, parents may benefit from assistance from an office staff member to complete screenings, such as when literacy is a challenge.
As noted above, screening plays an important role in promotion, prevention, and intervention. Family engagement is central to communicate the “why” of screening and to partner with the parent/caregiver as experts on their child/adolescent, and to partner in planning. When a screen does not show risk, the role of the PCC is to reinforce strengths and reiterate openness to discussion if concerns arise. When a screen does show risk, a brief intervention using common factors communication skills is the next step. Common factors communication skills use components of interventions common to diverse therapies, coming from family therapy, cognitive therapy, and motivational interviewing. Using common factors is a brief and effective way to identify the family’s perspective and preferences and make plans for next steps. The HEL2P3 mnemonic guides the process:
H—Hope: Express hope in addressing the concern
E—Express empathy
L2—Language, loyalty: Restate the concern in the language used by the family and assure loyalty to work together
P3—Permission, partnership, plan: Ask permission to ask more questions, commit to partnership in addressing, and develop a plan
Finally, coding correctly for screening activities can support sustainment in the practice. Many payers reimburse for Current Procedural Terminology code 96127, which can be used for screenings in Tables 1 and 2.This can be used on the same date in addition to codes a practice may already be using for developmental screening (96110) and maternal depression screening (96161), recognizing that social-emotional screening is distinct from these areas.
Following up on positive mental health screenings: Next steps
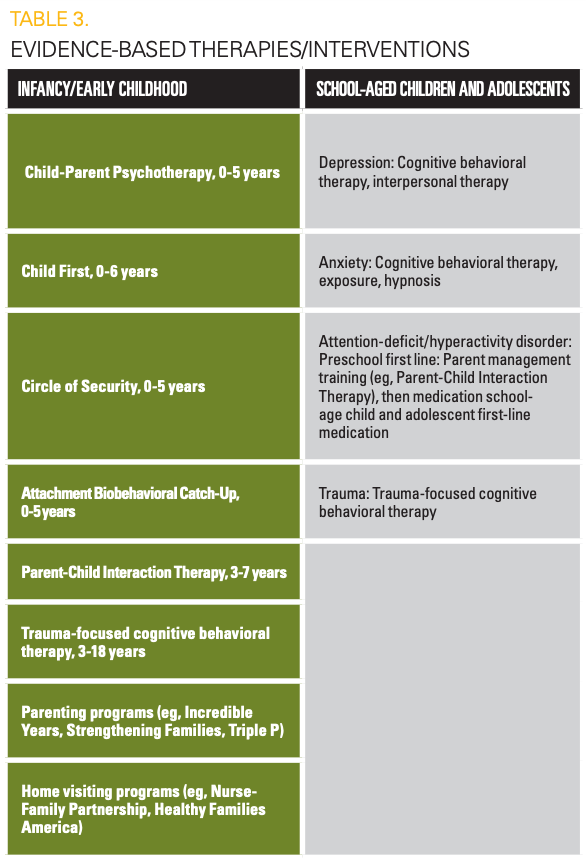
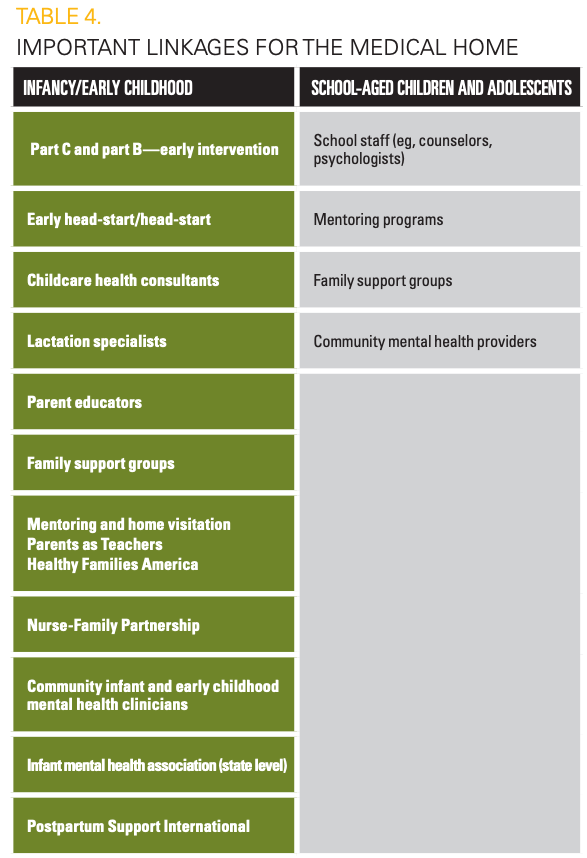
The plan may include using secondary screens to clarify diagnosis, either in the same visit or in follow-up. If the plan includes linkage/referral to a resource, prioritizing a warm hand off is ideal. Practice readiness requires outreach to build collaborative relationships with community partners (Tables 3 and 4). This process begins before implementation of screening and is an ongoing activity for the practice.
In addition to promotion, prevention, and early identification, the PCC may do further assessment and management themselves, or in consultation or comanagement with a mental health clinician. Such consultative and collaborative relationships have been enhanced by the development of child psychiatry access programs nationally (www.nncpap.com), and by integration of mental health clinicians as members of the medical home team. Further evaluation often requires additional time beyond the initial visit when a positive screening result is identified. This can be done by scheduling a follow-up visit specifically to focus on social-emotional concerns. Telehealth can be a good option for social-emotional follow-up visits. As further evaluation and discussion with families often requires substantial time, using time-based coding can facilitate appropriate reimbursement and enable sustainment of the comprehensive approach needed to address mental health problems effectively.
In their relationships with children and families, it is the role of the pediatrician to engage patients and families in eliciting strengths and risks, screening, assessing when risks are identified, and partnering with families in management. However, pediatricians do not do this alone. The care team always includes the parent/caregiver, child/adolescent, and the pediatrician, and can include a mental health specialist, a developmental-behavioral pediatrician, a pediatric subspecialist, an early intervention coordinator, a teacher, and/or a school psychologist. The challenge for the team is to standardize communication and feedback, particularly with nonmedical partners, and to assess outcomes for children and families.
For more from the March mental health issue of Contemporary Pediatrics, click here.
References:
1. Foy JM, Green CM, Earls MF; Committee on Psychosocial Aspects of Child and Family Health, Mental Health Leadership Work Group. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757. doi:10.1542/peds.2019-2757
2. Bitsko RH, Claussen AH, Lichstein J, et al. Mental health surveillance among children - United States, 2013-2019. MMWR Suppl. 2022;71(2):1-42. doi:10.15585/mmwr.su7102a1
3. Swanson SA, Eyllon M, Sheu YH, Miller M. Firearm access and adolescent suicide risk: toward a clearer understanding of effect size. Inj Prev. Published online May 14, 2020. doi:10.1136/injuryprev-2019-043605
4. Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142-1150. doi:10.1001/jamapediatrics.2021.2482
5. Green CM, Foy JM, Earls MF; Committee on Psychosocial Aspects of Child and Family Health, Mental Health Leadership Work Group. Achieving the pediatric mental health competencies. Pediatrics. 2019;144(5):e20192758. doi:10.1542/peds.2019-2758
6. Weitzman C, Wegner L; Section on Developmental and Behavioral Pediatrics. Promoting optimal development: screening for behavioral and emotional problems. Pediatrics. 2015;135(2):384-395. doi:10.1542/peds.2014-3716
7. Mental health care in pediatric practice. American Academy of Pediatrics. Accessed February 8, 2024. https://downloads.aap.org/AAP/PDF/Algorithm_Integration_of_Mental_Health_Care_Into_Pediatric_Practice.pdf