Obesity in children and the impact of COVID-19
As we begin to emerge from the national lockdown due to the COVID-19 pandemic, many pediatricians may find that the already widespread problem of youth-onset obesity is worse than ever.
Social distancing, virtual school, more screen time, and less physical activity have all contributed to increased weight gain among youth.1 Moreover, the pandemic has magnified and exacerbated many of the preexisting racial and socioeconomic disparities in health care.2,3 Whether visits are in person or via telemedicine, the recognition, management, and treatment of obesity in youth by primary care providers is more important than ever.
Epidemiology
Adiposity is measured using body mass index (BMI) or weight (kg)/height (m2). Because of growth and development during childhood, BMI percentiles for age and sex as defined by the Centers for Disease Control and Prevention are used to estimate adiposity, with overweight defined as 85th to less than 95th percentile, obesity 95th percentile or greater, and extreme obesity, 120% of the 95th percentile or at least 35 kg/m2.4-6
Overweight and obesity disproportionately affect racial and ethnic minority groups, particularly Hispanic and non-Hispanic Black youth, and obesity prevalence is also associated with poverty.7 The latest data from the National Health and Nutrition Examination Survey show that from 1999-2000 to 2017-2018, obesity prevalence increased from 15.8% to 19.3% in children aged 6 to 11 years. Among adolescents aged 12 to 19 years, obesity rose from 16% to 20.9% and severe obesity went from 5.3% to 7.6%, the latter largely driven by increases in non-Hispanic Black and Mexican Americans.8 Of note, these numbers do not account for the disparities intensified during the pandemic, the results of which will become evident in the future.
Obesity prevalence data tell only part of the story because early-onset obesity increases future risk. The Early Childhood Longitudinal Study of 2014 illustrated that overweight 5-year-olds were 4 times as likely as normal-weight peers to become obese at 14 years, with a 9-year cumulative incidence of 31.8% vs 7.9%.9 Moreover, obesity during adolescence raises incident risk of severe obesity as an adult.10 Multiple studies have shown the relationship between obesity during adolescence and dyslipidemia, hypertension, and type 2 diabetes mellitus (T2DM) as an adult.11,12
Etiology and natural history
The etiology of pediatric obesity is multifold, a combination of genetics and environment. In addition to family history, the “thrifty gene hypothesis,” proposed by David Barker, states that undernutrition in utero causes adaptive metabolic changes in the fetus, such as insulin resistance, that do not match the postnatal extrauterine environment, which has excess calories with decreased physical activity.13,14 This concept of fetal origins of adult disease has been implicated in the association of intrauterine growth restriction and small for gestational age, with increased later cardiometabolic risk.15 Epigenetics has also been implicated, with DNA methylation changes and posttranslational histone modifications causing heritable genetic changes, potentially programming later diseases.16 Early hypernutrition can also be a risk factor, with rapid weight gain in the first 4 to 6 months of life associated with obesity later in childhood.17
In rare cases, genetic syndromes, such as Prader-Willi, Alstrom, and Bardet-Biedl syndromes, and monogenic mutations, such as MC4R, LEP, and POMC mutations, can cause severe obesity, usually characterized by obesity onset before age 5 years. Some syndromes involve intellectual disability and often involve hyperphagia. Endocrinologic causes such as hypothyroidism and Cushing Disease are also less common, and generally involve attenuated height or height velocity in addition to excess weight, in growing youth.18
Numerous environmental factors contribute to excess weight gain during childhood: dietary factors, such as consuming more sugar-sweetened beverages, eating larger portions, skipping meals, decreasing intake of fruits and vegetables (which can be related to food insecurity), and consuming more fast food. Other significant contributors include reduced physical activity, increased sedentary activity (even before the pandemic), and dysregulated sleep.
Assessment
Clinical assessment includes BMI measurement and a thorough physical exam. Genetic testing is recommended for youth with early-onset obesity before age 5 years.18 After recognition of excess weight for height, screening for comorbidities is critical, with referral to subspecialists as indicated. A detailed family history should also be obtained for these comorbidities.
Cardiovascular complications of obesity include hypertension and dyslipidemia. Blood pressure should be measured with the appropriate cuff size and assessed using percentiles specific for age, sex, and height. Fasting lipids are used to detect dyslipidemia. Typically, metabolic dyslipidemia includes a pattern of elevated triglycerides, decreased high-density lipoprotein cholesterol, and increased small dense low-density lipoprotein (LDL) particles. LDL cholesterol is of- ten normal or only slightly elevated.19 Headaches can be a symptom of hypertension but also of pseudotumor cerebri, a comorbidity diagnosed by fundoscopic exam.
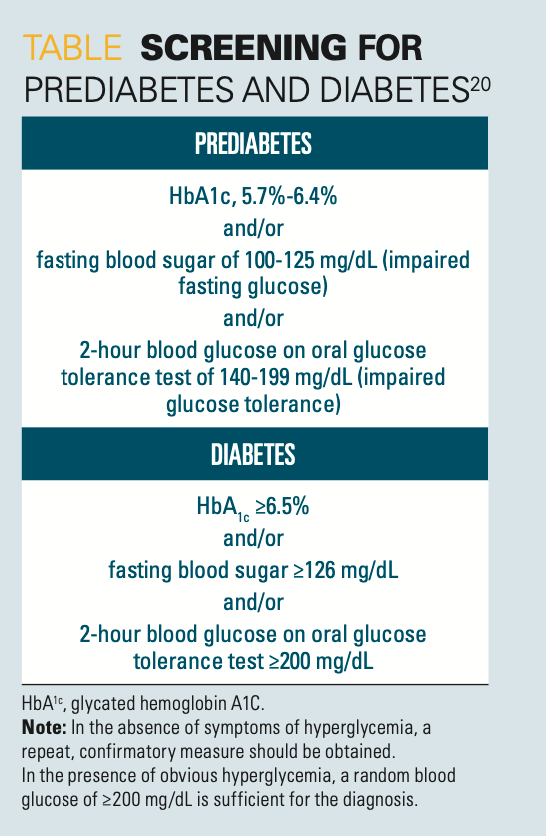
Endocrinologic complications include prediabetes, T2DM, and polycystic ovarian syndrome (PCOS). Diabetes can elicit a history of polyuria, polydipsia, and nocturia but can also be asymptomatic. Skin examination may demonstrate acanthosis nigricans, indicative of insulin resistance. Screening can be done using glycated hemoglobin A1c (HbA1c), fasting glucose, and/or oral glucose tolerance test, as described in the Table.20 Diabetes diagnosis or a prediabetes diagnosis should initiate a referral to a pediatric endocrinologist. Studies have indicated that youth-onset T2DM progresses faster than adult-onset T2DM and can present with complications at the time of diagnosis.21 Aggressive diabetes screening and treatment are indicated as per guidelines of the American Diabetes Association.22 A menstrual history, as well as history and physical examination for acne and hirsutism, should be obtained to screen for PCOS, which also increases cardiometabolic risk.23
Table
Nonalcoholic fatty liver disease (NAFLD), a chronic hepatic liver disease, is associated with increased adiposity and insulin resistance. It results from excess adipose deposition in the liver; in the United States, NAFLD has become the most common liver disease in youth. Pediatricians should screen for NAFLD in overweight and youth with obesity by measuring alanine transaminase and aspartate transaminase.24
Another significant comorbidity of pediatric obesity is obstructive sleep apnea. History obtained may include snoring, audible apnea, restless sleep, headaches, and daytime sleepiness. On physical examination, the child may have enlarged tonsils and adenoids. If sleep apnea is suspected, diagnostic polysomnography should be ordered. Depending on the situation, treatment can include tonsillectomy and/or adenoidectomy, as well as continuous positive airway pressure.25 Musculoskeletal disorders, such as Blount disease and slipped capital femoral epiphysis, may present with joint pain, and are associated with overweight/obesity because of the greater mechanical force placed on the joints.26 Physical examination may also indicate flatfeet, which can be treated with orthopedic shoe inserts.
Mental health concerns, such as depression and anxiety, are also significant potential comorbidities of obesity.27 Pediatric providers should specifically ask about symptoms of depression—hopelessness, trouble sleeping, lack of interest or motivation, and changes in appetite, as well as anxiety, spurred by loneliness, isolation, and uncertainty.28 This is especially important given the COVID-19 pandemic’s exacerbation of many social stressors affecting families, such as food insecurity, poverty, and racial disparities.29 The already strained pediatric mental health infrastructure has been further challenged by the pandemic, making mental health screening by primary care providers all the more important.28
Treatment
The mainstay of treatment for pediatric obesity involves behavior modification through increased physical activity, improved nutrition, and decreased sedentary activity. Intensive lifestyle modification is challenging, but can be effective if family-based and age/culturally appropriate, both very important.18, 30 Nutritional modifications include consuming less fast food, sugar-sweetened beverages, added sugars, and saturated fats and consuming more fruits, vegetables, whole grains, and fiber. Youth should avoid skipping meals, which often leads to overeating later in the day, as well as avoid snacking throughout the day. Eating slower and recognizing satiety cues is essential because many individuals eat when bored or emotionally upset. Decreasing portions is also important. The US Department of Agriculture’s MyPlate resources can help demonstrate appropriate amounts of various types of foods to make up one’s plate.31 Meeting with a pediatric nutritionist, if available, can be a significant resource for families.
Physical activity can help maintain weight loss as well as improve insulin sensitivity and dyslipidemia. Gradually increasing moderate to vigorous physical activity, with a minimum of 20 minutes/day and a goal of 60 minutes/day, is recommended.18 Setting specific, realistic goals can help avoid discouragement. Tracking progress and providing non–food-related rewards can also be helpful. Other goals include limiting sedentary activity and nonacademic screen time to 1 to 2 hours per day. The COVID-19 pandemic has caused the amount of time youth spend in front of screens to explode, with deleterious effects on sleep and mood. The provider should also encourage the child to get an age-appropriate amount of sleep on a reasonable day-night schedule.
If lifestyle modification does not result in adequate weight loss, pharmacotherapy is an option. Several new obesity medications have been US Food and Drug Administration approved for adults (eg, lorcaserin, phentermine plus topiramate, bupropion plus naltrexone) and are considered appropriate for individuals 16 years or older with a BMI of either 30 kg/m2 or higher or at least 27 kg/m2 with at least 1 obesity comorbidity.18 Until recently, only orlistat, a lipase inhibitor blocking fat absorption, had been approved for weight loss in children 12 to 16 years, but its use was limited because of its adverse effects (AEs) of oily spotting, flatulence, and abdominal pain. Recently, liraglutide, a receptor agonist of the incretin glucagon-like peptide-1 (GLP-1), was shown to effectively cause weight loss in conjunction with lifestyle modification in 12- to 18-year-olds.32 Contraindications include a history of pancreatitis, a family history of medullary thyroid cancer, or multiple endocrine neoplasia type 2. AEs include nausea, abdominal pain, vomiting, and diarrhea, which tend to improve with use. Liraglutide is given as a daily subcutaneous injection, and it increases endogenous insulin production, decreases gastric transit time, and suppresses appetite. Liraglutide was also recently approved for the treatment of youth-onset T2DM, at a lower dose than that used to treat obesity.33
For cases in which intensive lifestyle modification has not been effective, bariatric surgery may also be an option. Bariatric surgery has been called metabolic surgery, as its mechanism of action is thought to include alterations in appetite regulating hormones, such as ghrelin and GLP-1. However, given the unknown effects on growth and development, it is only recommended for youth under particular conditions:
- Tanner 4-5 pubertal development and having attained final or near-final height,
- BMI ≥40kg/m2 or BMI ≥35kg/m2 with significant, extreme comorbidities not adequately treated by lifestyle modification and/or pharmacologic treatment,
- Undergone psychological evaluation to rule out untreated underlying psychological disorder (although obesity-related psychological distress may be present) and ensure that the patient has a stable environment,
- Willingness to adhere to a healthy diet and physical activity, and
- Having access to an experienced bariatric surgeon at a pediatric bariatric surgery center of excellence capable of long-term follow-up for complications as well as nutritional deficiencies.18
Several different types of surgery have been done, including the Roux-en-Y gastric bypass (RYGB) surgery and increasingly, the less complex vertical sleeve gastrectomy (VSG), involving resection of 85% of the stomach, including the greater curvature and fundus. The VSG has decreased complications compared to the RYBG, and 3-year follow up data from the Teen-LABS study showed a mean BMI decrease of 28% in those receiving the RYBG and 26% in those receiving the VSG.34 This study also demonstrated 95% remission of T2DM at 3 years. Vitamin and mineral deficiencies are common post-operatively, with vitamin B12, B1, and folate deficiencies common in both. RYBG can also result in iron, copper, selenium, and zinc deficiencies, with decreased bone mineralization as well.18
The pandemic has magnified the problem of pediatric obesity and its complications. We have yet to truly understand the long-term effects of quarantine and isolation on a child’s mental and physical health. It will be critical to address the physical, mental, and social implications of pediatric obesity.
References
1. Kim ES, Kwon Y, Choe YH, Kim MJ. COVID-19-related school closing aggravate obesity and glucose intolerance in pediatric patients with obesity. Sci Rep. 2021;11(1):5494. doi:10.1038/s41598-021-84766-w
2. Jenssen BP, Kelly MK, Powell M, Bouchelle Z, Mayne SL, Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021;147(5):e2021050123. doi:10.1542/peds.2021-050123
3. Tester JM, Rosas LG, Leung CW. Food insecurity and pediatric obesity: a double whammy in the era of COVID-19. Curr Obes Rep. Dec 2020;9(4):442-450. doi:10.1007/s13679-020-00413-x
4. Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;(314):1-27. https://pubmed.ncbi.nlm.nih.gov/11183293/
5. Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(suppl 4):S193-228. doi:10.1542/peds.2007-2329D
6. Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689-1712. doi:10.1161/CIR.0b013e3182a5cfb3
7. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164-S192. doi:10.1542/peds.2007-2329C
8. Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and Hispanic origin-1999-2000 to 2017-2018. JAMA. 2020;324(12):1208-1210. doi:10.1001/jama.2020.14590
9. Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403-411. doi:10.1056/NEJMoa1309753
10. The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. Research Support, N.I.H., Extramural. JAMA. 2010;304(18):2042-2047. doi:10.1001/jama.2010.1635
11. Srinivasan SR, Elkasabani A, Dalferes ER Jr., Bao W, Berenson GS. Characteristics of young offspring of type 2 diabetic parents in a biracial (black-white) community-based sample: the Bogalusa Heart Study. Metabolism. 1998;47(8):998-1004. doi:10.1016/s0026-0495(98)90358-4
12. Bjerregaard LG, Jensen BW, Angquist L, Osler M, Sorensen TIA, Baker JL. Change in overweight from childhood to early adulthood and risk of type 2 diabetes. N Engl J Med. 2018;378(14):1302-1312. doi:10.1056/NEJMoa1713231
13. Barker DJ. The fetal and infant origins of disease. Eur J Clin Invest. 1995;25(7):457-463. doi:10.1111/j.1365-2362.1995.tb01730.x
14. Hales CN, Barker DJ. The thrifty phenotype hypothesis. Br Med Bull. 2001;60:5-20. doi:10.1093/bmb/60.1.5
15. Calkins K, Devaskar SU. Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care. 2011;41(6):158-76. doi:10.1016/j.cppeds.2011.01.001
16. Devaskar SU, Thamotharan M. Metabolic programming in the pathogenesis of insulin resistance. Rev Endocr Metab Disord. 2007;8(2):105-113. doi:10.1007/s11154-007-9050-4
17. Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr. 2003;77(6):1374-1378. doi:10.1093/ajcn/77.6.1374
18. Styne DM, Arslanian SA, Connor EL, et al. Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(3):709-757. doi:10.1210/jc.2016-2573
19. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213-256. doi:10.1542/peds.2009-2107C
20. American Diabetes A. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(suppl 1):S15-S33. doi:10.2337/dc21-S002
21.TODAY study group. A clinical trial to maintain glycemic control in youth with type 2 diabetes. Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't. N Engl J Med. 2012;366(24):2247-2256. doi:10.1056/NEJMoa1109333
22. American Diabetes A. 13. Children and adolescents: standards of medical dare in diabetes-2021. Diabetes Care. 2021;44(suppl 1):S180-S199. doi:10.2337/dc21-S013
23. Ibanez L, Oberfield SE, Witchel S, et al. An international consortium update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm Res Paediatr. 2017;88(6):371-395. doi:10.1159/000479371
24. Vos MB, Abrams SH, Barlow SE, et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the expert committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr. 2017;64(2):319-334. doi:10.1097/MPG.0000000000001482
25. Wise MS, Nichols CD, Grigg-Damberger MM, et al. Executive summary of respiratory indications for polysomnography in children: an evidence-based review. Sleep. 2011;34(3):389-398AW. doi:10.1093/sleep/34.3.389
26. Taylor ED, Theim KR, Mirch MC, et al. Orthopedic complications of overweight in children and adolescents. Pediatrics. 2006;117(6):2167-2174. doi:10.1542/peds.2005-1832
27. BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009;123(2):697-702. doi:10.1542/peds.2008-0687
28. Korioth T. Updated guidance focuses on mental health risks, needs during pandemic. AAP News. March 15, 2021. Accessed August 3, 2021. https://www.aappublications.org/news/2021/03/15/ebhguidance3-15-21
29. Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. BMI status and associations between affect, physical activity and anxiety among U.S. children during COVID-19. Pediatr Obes. 2021:e12786. doi:10.1111/ijpo.12786
30. McGovern L, Johnson JN, Paulo R, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93(12):4600-5. doi:10.1210/jc.2006-2409
31. U.S. Department of Agriculture. MyPlate. Accessed August 4, 2021. https://www.myplate.gov/
32. Kelly AS, Auerbach P, Barrientos-Perez M, et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N Engl J Med. 2020;382(22):2117-2128. doi:10.1056/NEJMoa1916038
33. Tamborlane WV, Barrientos-Perez M, Fainberg U, et al. Liraglutide in children and adolescents with type 2 diabetes. N Engl J Med. 2019;381(7):637-646. doi:10.1056/NEJMoa1903822
34. Inge TH, Courcoulas AP, Jenkins TM, et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374(2):113-123. doi:10.1056/NEJMoa1506699