Positional Plagiocephaly, Part 1:A Practical Guide to Evaluation
One of the more common conditions pediatricians diagnose is deformity of the skull. Deformational plagiocephaly may be caused by compressive forces in utero (eg, multiple births) or by constant pressure on one portion of the newborn’s malleable skull when the infant is kept in the same supine position for prolonged periods.
ABSTRACT: Deformational plagiocephaly may be caused by compressive forces in utero (eg, multiple births) or by constant pressure on one portion of the newborn’s malleable skull when the infant is kept in the same supine position for prolonged periods. Certain types of premature bony fusion (craniosynostosis), especially lambdoid synostosis, may be confused with deformational plagiocephaly. A thorough evaluation is critical to differentiating the conditions and includes the acquisition of the family and medical history, examination of the face and skull from multiple angles, and neck examination for torticollis. Plain radiographs can help identify the cause in uncertain cases. Additional imaging studies may be considered, but only after consultation with a craniofacial surgeon.
One of the more common conditions pediatricians diagnose is deformity of the skull. The term "plagiocephaly," from the Greek words plagio (oblique, slanted, or twisted) and kephale (head), simply describes an asymmetrical cranium. Although no human head is truly symmetrical, even small skull deformities in infants may cause concern among parents and physicians. Parental concerns often focus on the appearance of the child’s misshapen head and the possibility for developmental delay as a result of compression of the underlying brain. Research studies examining the association between plagiocephaly and developmental delay are inconclusive.
The number of infants with skull deformation has increased since the early 1990s when the American Academy of Pediatrics (AAP) proposed that infants be positioned on their backs to reduce the incidence of sudden infant death syndrome (SIDS).1 Along with encouraging parental compliance with the AAP’s Back to Sleep campaign, it is important to check all infants for skull deformity, and if identified, correctly diagnose the cause to ensure proper management.
Here a practical guide to the evaluation of the infant with an odd-shaped skull is provided that focuses on how to distinguish positional plagiocephaly from craniosynostosis. In a forthcoming article, we will review strategies to prevent skull deformation and treatment of infants with nonsynostotic plagiocephaly.
CAUSES OF SKULL DEFORMITY
Deformity of the skull in infants may develop from conditions such as craniosynostosis or from mechanical forces that put pressure on the malleable cranial bones. The normal newborn’s skull consists of several membranous bones that are joined by sutures (Figure 1). The fontanelles (intersections of 2 or more sutures) provide space between the developing bones, allowing for skull changes (called molding) during parturition and for rapid growth of the brain during infancy.2 Complete ossification of the fontanelles normally occurs by 20 to 24 months of age. The anterior fontanelle is the most prominent in the midline portion of the skull. It is the diamond-shaped area above the forehead at the confluence of the coronal and metopic sutures. A corresponding posterior fontanelle lies in the midline at the confluence of the lambdoid sutures. Paired anterolateral fontanelles lie on either side of the skull directly below the anterior fontanelle, and paired posterolateral fontanelles lie between the squamosal, parietal, and occipital bones.
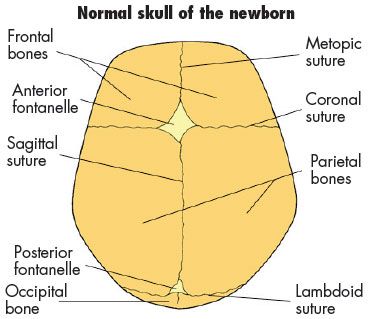
Figure 1 – The several membranous bones of the normal newborn’s skull are joined by sutures that are intersected by fontanelles. The fontanelles facilitate molding during childbirth and rapid growth of the brain during infancy. (Reprinted with permission from StayWell Custom Communications.)
The sutures normally fuse at different times in childhood and early adulthood.3 Premature fusion of 1 or more sutures (craniosynostosis) produces characteristic deformities of the skull that may be confused with deformational or positional plagiocephaly, in which the sutures remain patent but the bones are deformed.
Deformational plagiocephaly.
Deformity of the skull as a result of compressive forces in utero may be caused by multiple births or oligohydramnios, which may limit the ability of the fetus to reposition itself and avoid prolonged pressure in one area of the cranial vault. Ex utero deformational plagiocephaly is similarly a result of constant gravitational forces on the newborn’s malleable skull, such as when an infant is kept in the same supine position for prolonged periods (Figure 2) or with collapse of the over-expanded calvarium in the patient undergoing ventricular shunting for hydrocephalus.
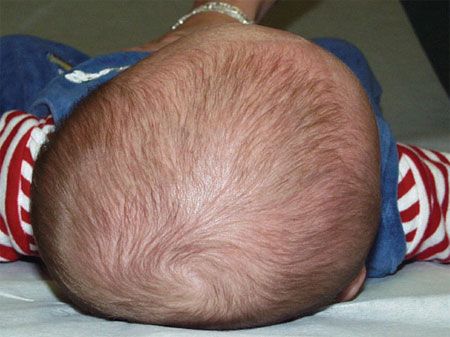
Figure 2 – The incidence of positional plagiocephaly has risen dramatically since the American Academy of Pediatrics recommended the supine sleep position. (Reprinted with permission from Losee JE et al.
Plast Reconstr Surg.
2005.
7
)
The reported incidence of positional plagiocephaly ranges from 5% to 48%.4 Its recognition and diagnosis have become more common since the AAP’s recommendation for supine sleep positioning. Although successful in reducing the incidence of SIDS, supine positioning increases the time newborns spend on their backs. The combination of a persistent sleep position and the newborn’s inability to control and lift the head allows for constant pressure in one area of the skull. The resulting deformity is often unilateral occipital flattening, with an ipsilateral anterior displacement of the craniofacial features.
Craniosynostosis. Intrinsic abnormality in the cranial skeleton can occur as part of a syndrome or as an isolated defect (nonsyndromic), with unknown cause. The prevalence of craniosynostosis may be around 1 per 1800 to 2200 births or higher.5 The deformity results from the inability of bone to be laid down along the suture, which prevents growth across the suture. Thus, the skull can grow only parallel, rather than perpendicular, to the suture. This growth restriction produces different head shapes depending on the suture involved.
Scaphocephaly. Premature fusion of the midline sagittal suture that extends the length of the skull from the anterior fontanelle to the posterior fontanelle is the most common type of craniosynostosis. Fusion of this suture produces a characteristically long and narrow "scaphocephalic" skull that appears pinched at each of the temple regions. The biparietal distance is narrowed, whereas in the normal skull, this area is typically the widest (Figure 3).
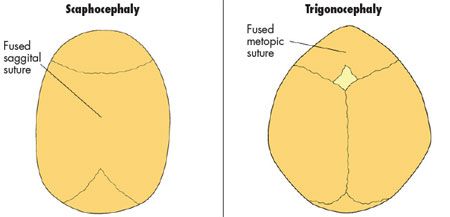
Figure 3 – In craniosynostosis, one or more of the sutures close prematurely. Several types of craniosynostosis exist. Two of the more common types are shown here. (Reprinted with permission from StayWell Custom Communications.)
Anterior plagiocephaly. The second most common site of involvement is the coronal suture. Two paired coronal sutures run inferolaterally from the anterior fontanelle. Unilateral coronal synostosis produces a characteristic asymmetrical drawn-up or windblown appearance to the orbit on the side of the fusion. The asymmetry is obvious on gross inspection. Plain anteroposterior radiographs show a characteristic "harlequin" deformity on account of the different orbital shapes (Figure 4).

Figure 4 – Anterior plagiocephaly is characterized by the "harlequin" deformity on plain anteroposterior radiograph on account of the different orbital shapes.
Trigonocephaly. The third most common site of fusion is the metopic suture, which extends from the anterior fontanelle to the nasion. The resultant growth pattern creates a triangle- shaped skull, in which the outer corners of the superior orbits appear pinched and a midline vertical ridge runs down the middle of the forehead (see Figure 3). A palpable or visible metopic ridge develops in the first year of life; however, the head shape itself remains normal. This can be a normal variant, and the metopic ridge may appear to be fused on imaging. Although in the absence of trigonocephaly, this likely represents normal fusion of the metopic suture.
Posterior plagiocephaly. Fusion of the lambdoid suture, a paired structure that runs inferolaterally from the posterior fontanelle, is the least common type of craniosynostosis. The resultant deformity primarily affects the posterior skull, causing hypertrophy just above the mastoid air cells; however, it may affect the anterior face as well. Lambdoid craniosynostosis is easily confused at first observation with deformational plagiocephaly.6 Distinguishing features of each condition are shown in Figure 5.
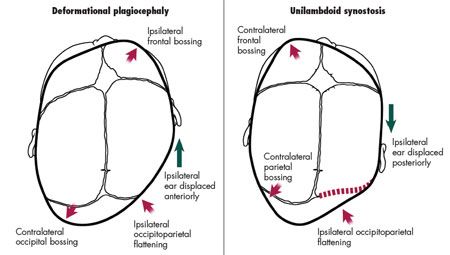
Figure 5 – Deformational plagiocephaly (left) can be easily confused with unilambdoid synostosis (right). The distinguishing features of each condition are shown here. (Illustration by Renee L. Cannon.)
EVALUATION
A thorough history and careful examination are critical in diagnosing positional plagiocephaly and differentiating it from craniosynostosis.
Family history. Because most of the more recognized craniofacial syndromes are transmitted in an autosomal dominant fashion, it is important to inquire about any relatives with craniofacial syndromes or isolated cranial anomalies. While the majority of cases of syndromic craniosynostosis involve multiple sutures, unilateral coronal craniosynostosis may be the most common hereditary form of single-suture fusion and is inherited in the autosomal dominant pattern. Various genetic syndromes that present with unilateral or bilateral synostosis are related to one of the genes for fibroblast growth factor receptor. Although the pathogenesis of isolated single-suture craniosynostosis remains elusive, genetic and environmental components are possible.
Medical history. The clinician should identify any prenatal factors that may contribute to skull deformity (eg, the method of delivery). Infants born vaginally may present with greater initial deformity than those born via caesarean delivery because of the smaller space of the birth canal. Skull asymmetry caused by molding during parturition decreases over time. In infants with postnatal premature fusion, the skull may appear symmetrical at birth but demonstrates deformity over weeks to months. The parents should be asked to quantify the amount of time the infant spends in a supine or prone position each day and the total time spent in car seats, bouncers, swings, and other devices that may allow for pressure against one area of the skull.
Physical examination. Perform a complete head-to-toe examination, focusing on the face and skull and examining the infant from anterior, posterior, and vertex views.
Anterior view. The infant may be placed in the parent’s lap, facing forward, while you evaluate the anterior craniofacial skeleton for symmetry. Assess head tilt as well as the appearance of the forehead, orbits, midface, and mandible. With typical unilateral deformational plagiocephaly, the ipsilateral forehead is displaced anteriorly, with the illusion of asymmetrical enlargement; the ipsilateral palpebral fissure is often vertically elongated; and the ipsilateral cheek is displaced anteriorly. All of these features create an illusion of asymmetrical enlargement.
From this angle, note any areas of bossing (or retrusion) in the forehead. Bossing may appear as an area of highlight (or lowlight) because it more easily reflects light. Also take note of the lateral supraorbital bar, because pinching on 1 or more sides may indicate suture fusion. Similarly, note any asymmetry of the orbit. A ridge may be palpable in the midline (metopic synostosis) or laterally (coronal synostosis).
Posterior view. Turn the infant to face the parent to evaluate the posterior head. From the back, note any localized alopecia, which is an early indicator of persistent pressure and possibly positional plagiocephaly. The mastoid skull base is typically symmetrical in positional plagiocephaly but enlarged in lambdoid synostosis. The characteristic occipital flatness is associated with anterior displacement of the ipsilateral ear; this is unlike lambdoid synostosis, in which the ear is displaced posteriorly. Lambdoid synostosis produces prominence above the mastoid bone and frequently a palpable ridge over the suture-features that are usually absent in positional plagiocephaly.4 These primary changes in the posterior cranial vault may produce a canting of the entire craniofacial complex, better seen from the front.
Vertex view. Place the infant supine with the head in your lap and the feet toward the parent to give a vertex perspective. This view is perhaps the most valuable and may also be achieved by looking down from above. The classic head shape in patients with positional plagiocephaly is a parallelogram. Infants generally choose one side of the head to sleep on. With persistent positioning, external pressure can produce occipital flattening and ipsilateral frontal bossing. Over time, the occipital flattening perpetuates itself because it becomes harder for the infant to roll off the flat area.
Measurement of head circumference is important to document absolute size and growth over time. It is less helpful for identifying plagiocephaly, either positional or synostotic, because in both types the absolute head circumference may be normal, despite the skull being misshapen.
Symmetry of cranial base. When examining the symmetry of the cranial base, gently place an index finger in each ear canal and note the position of the fingers relative to one another observed from above. In cases of positional plagiocephaly, the cranial base is shifted anteriorly on the affected side, and the 2 fingers do not lie opposite one another.
Neck examination. Examine and palpate the neck for masses, suppleness, range of motion, and head movement. Associated torticollis may be present in both positional plagiocephaly and craniosynostosis. It can be recognized in the anterior view by paying particular attention to head tilt and twist; often the head deviates toward the affected side and tilts away. Contralateral sternocleidomastoid muscle stiffness is caused by persistent intrauterine or postnatal positioning. Palpation of the contralateral sternocleidomastoid muscle may elicit tenderness and tightness. Tightness of the muscle produces changes in the craniofacial skeleton even in the absence of positional pressure or suture fusion. Stretching the contralateral sternocleidomastoid muscle is an important part of treatment of infants with associated torticollis of any cause.
Examination of parents. It is also important to examine the patient’s parents. Skull shape is often hereditary, and midline occipital flattening may be normal if it is present in one or both parents.
IMAGING
Radiologic studies are helpful in cases in which the cause of the deformity is uncertain. Many surgeons perform studies to document findings consistent with craniosynostosis before proceeding to operative correction. The simplest study to order in these circumstances is a plain radiograph of the head, with anteroposterior (AP) and lateral views. The findings from this study can help identify the presence or absence of a patent suture. A patent sagittal suture may be seen at the vertex of the skull on the AP view, while paired coronal (anterior) and lambdoid (posterior) sutures should be apparent on the lateral view.
CT scanning provides a better indication of the patency of the major sutures but introduces the infant to a larger dose of radiation. The CT data acquired from a single study may be reformatted into a 3-dimensional reconstruction that provides an excellent representation of the deformity and is useful in consultation with the family. Because of the higher dose of radiation, order CT scans judiciously and only after consultation with a craniofacial surgeon, because many studies can be avoided.
References:
REFERENCES:
1.
American Academy of Pediatrics AAP TaskForce on Infant Positioning and SIDS: Positioningand SIDS [published correction appears in
Pediatrics.
1992;90(pt 1):264].
Pediatrics.
1992;89(pt 1):1120-1126.
2.
Moore KL, Persaud TV.
The Developing Human:Clinically Oriented Embryology.
6th ed. Philadelphia:WB Saunders; 1998.
3.
Bradley JP, Levine JP, Blewett C, et al. Studies incranial suture biology: in vitro cranial suture fusion.
Cleft Palate Craniofac J.
1996;33:150-156.
4.
Persing J, James H, Swanson J, Kattwinkel J;American Academy of Pediatrics Committee onPractice and Ambulatory Medicine, Section on PlasticSurgery and Section on Neurological Surgery.Prevention and management of positional skull deformitiesin infants. American Academy of PediatricsCommittee on Practice and Ambulatory Medicine,Section on Plastic Surgery and Section on NeurologicalSurgery.
Pediatrics.
2003;112(1 pt 1):199-202.
5.
Kabbani H, Raghuveer TS. Craniosynostosis.
Am Fam Physician.
2004;15;69:2863-2870.
6.
Pollack IF, Losken HW, Fasick P. Diagnosis andmanagement of posterior plagiocephaly.
Pediatrics.
1997;99:180-185.
7.
Losee JE, Feldman E, Ketkar M, et al. Nonsynostoticoccipital plagiocephaly: radiographic diagnosisof the "sticky suture."
Plast Reconstr Surg.
2005;116:1860-1869.