Prediabetes: How to identify children at risk
Children who are overweight or obese are potentially at risk for developing diabetes, but there’s more to identifying prediabetes than just obesity.
Philip Zeitler, MD, PhD

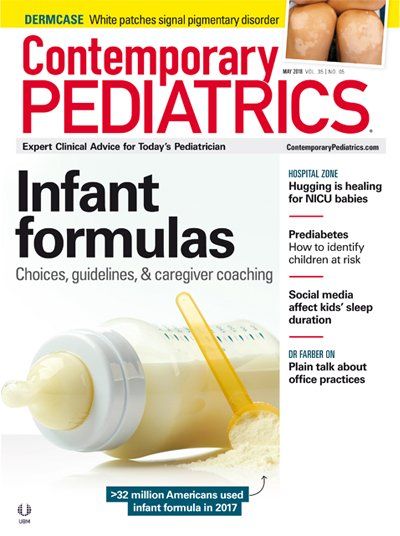
Table 1
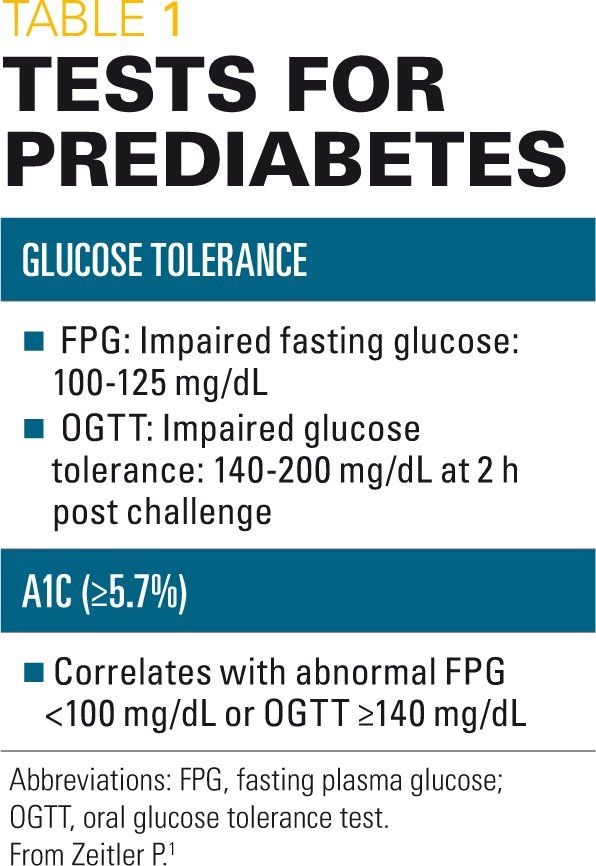
ICD-10 codes for diagnosing diabetes
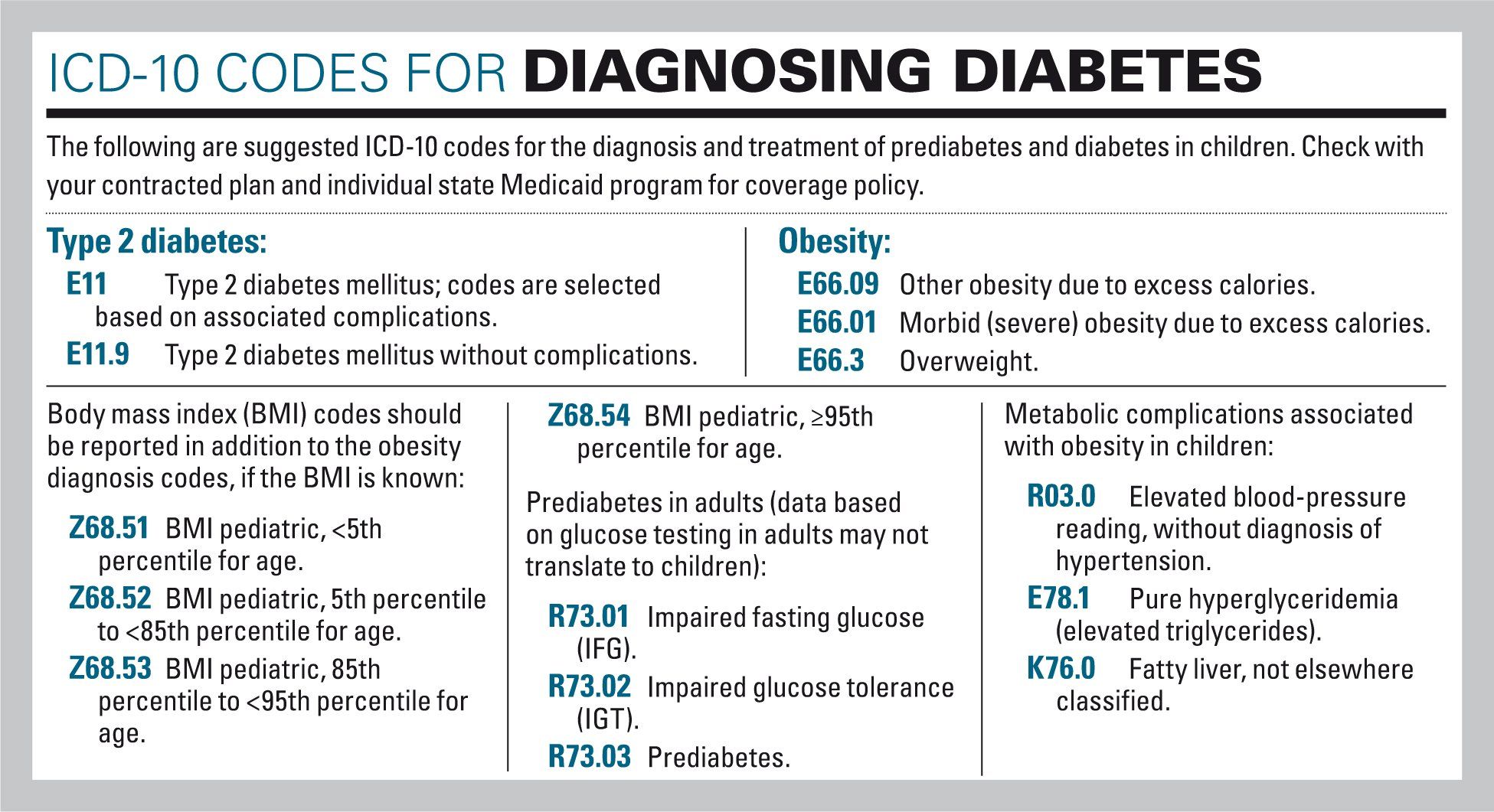
Table 2
Table 3
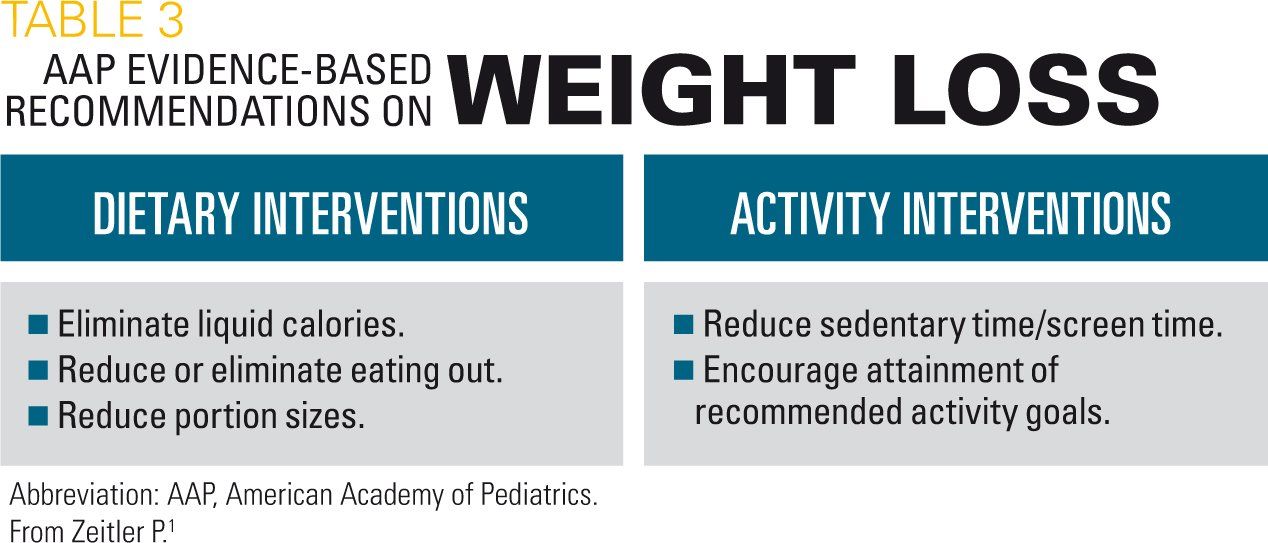
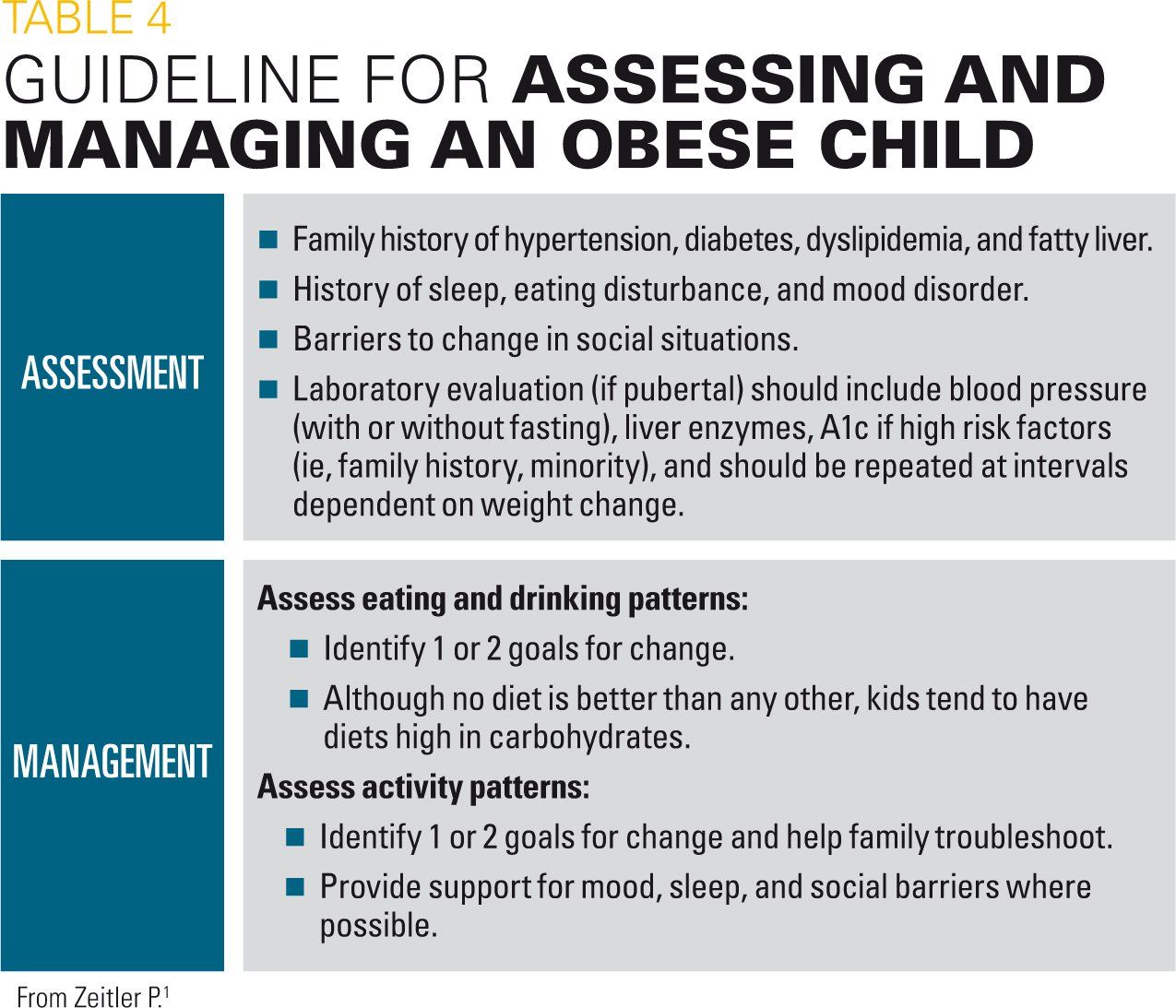
Table 4
Select resources for pediatricians

As the number of young persons developing type 2 increases, so has the awareness of clinicians on the importance of identifying children at risk to help prevent the deleterious effects of diabetes once established. Studies in adults with type 2 diabetes have identified specific risk factors for disease development, and a great deal of focus has been on identifying prediabetes in an attempt to improve prevention.
For both children and adults, obesity remains one of the key risk factors for developing type 2 diabetes. Children who are overweight or obese, therefore, are seen as potentially at risk of developing diabetes.
To date, little data are available on how to assess children at risk of developing type 2 diabetes. Assessment, therefore, has relied on data derived from adult studies and extrapolated to children. As such, the evidence base on which assessing risk of diabetes in children is limited at best and should be looked at with some caution.
This was an underlying message in a talk presented at the 2017 American Academy of Pediatrics (AAP) National Conference by Philip Zeitler, MD, PhD, professor of Pediatrics and Clinical Science and section head, Endocrinology, University of Colorado School of Medicine Anschutz Medical Campus, Aurora, Colorado, titled “Not yet diabetes: Assessing and managing children at risk.”1 In his presentation, Zeitler emphasized that although type 2 diabetes is on the rise in adolescents, it is still rare and not the main complication that clinicians should be focusing on when they see a child who is obese.
“Glucose is not the most common problem in obese kids; in fact, it is pretty darn rare,” Zeitler said, emphasizing that other disorders associated with obesity such as elevated triglycerides, fatty liver, and high blood pressure are much more common. “People should be thinking about these other more common conditions and not get too lost looking for prediabetes,” he said.
In his talk, Zeitler spoke about ways to assess and manage prediabetes in children while underscoring this main message that diabetes is not the most important potential disease risk for obese children and of the need to address obesity in all children regardless of their potential diabetes risk. To help clinicians get a better footing as to the real problem of prediabetes in children, he opened his talk by defining what prediabetes is and the limits of its utility in children.
Prediabetes is a concept, not a thing
Zeitler began with a brief overview of the pathophysiology of prediabetes, citing a number of studies in children that looked at impairments in glucose homeostasis in overweight children.
Overall, he underscored the difficulty of establishing prediabetes in children based on measures such as fasting plasma glucose (FPG) and the oral glucose tolerance test (OGTT) to assess risk factors predictive of impaired fasting glucose (IFG) or impaired glucose tolerance (IGT)-the intermediate phase between normal glucose tolerance and type 2 diabetes identified as prediabetes in adults. For example, some data suggest that impairments in insulin resistance and declining β-cell function may indicate children at heightened risk of developing type 2 diabetes, but these data are based on glucose testing measured against the specific cutoff threshold of less than 140 mg/dL established as defining prediabetes in adults.
This cutoff point, he cautioned, is defined in adults only and does not necessarily translate to children.
Compounding the difficulty of identifying prediabetes is the evolving criteria for diabetes itself. Zeitler reminded the audience that diabetes is defined by an increased risk for microvascular complications. Initially, he said, diabetes was based on a correlation of fasting glucose with increased incidence of retinopathy. In 1979, this correlation was based on a random or OGTT of greater than 200 mg/dL or FPG test of greater than 140 mg/dL, and in 1997 this changed to a FPG of greater than 126 mg/dL and the same OGTT. In 2009, the hemoglobin A1c test became standardized with a cutoff point of greater than 6.5 indicative of diabetes.
“Prediabetes is even more squishy than diabetes,” said Zeitler. “Diabetes is based on future cardiovascular risk, but prediabetes is based on the future risk of diabetes.”
Emphasizing that all the measures currently used to define diabetes are based solely on data derived from studies on adults, Zeitler underscored the need to recognize that prediabetes risk may not be the same for children. “The future risk of diabetes is not the same if you use the same criteria in children,” he said, highlighting as well that a “high-normal” glucose and A1c may be normal in puberty.
For example, he said that although the data suggest that adults with an A1c between 5.7% and 6.5% have increased risk for development of future diabetes, he highlighted data showing that an A1c of less than 6% in children actually indicates a nearly 0% chance of progressing to diabetes in a reasonable amount of time.
This is important because many children with elevated A1c or glucose levels are likely to spontaneously regress without any intervention because of changes in insulin resistance in puberty. (This is described more fully in the section “Management of prediabetes" below.)
All said, Zeitler questioned whether prediabetes is a useful concept when applied to children because of the high regression rate in children without any intervention. More useful, he suggested and emphasized, is recognition of the other more common metabolic complications associated with obesity in children, including high blood pressure, elevated triglycerides, and fatty liver.
Assessment of children at risk
Despite his reservation on the utility of using a diagnosis of prediabetes in children, Zeitler spent time addressing a main question that many clinicians have when considering how to assess the diabetes risk in children. That is: What is the best measure to use for this assessment? Table 1 lists the current measures used.
Saying there is a lot of noise in the literature about which test is better, Zeitler said that none of these current tests can be considered standard in children as they were developed to diagnose prediabetes in adults. “All the approaches we use for screening children for prediabetes are flawed in that they were extrapolated from adults,” he said.
With that understanding, he nonetheless noted that both a glucose tolerance test and A1c test can be used, as some people advocate, but he cautioned that such an approach is expensive “for what turns out to be a pretty rare disorder.”
Instead, Zeitler recommended using the A1c test, citing it as an imperfect but efficient test for evaluating high-risk kids. Table 2 lists several practical benefits of the A1c test over glucose tolerance testing. However, he also cautioned that, similar to measurement of glucose tolerance, the use of A1c is limited in that it will identify prediabetes in some kids but not others. “Both glucose tolerance testing and the A1c will identify overlapping but not identical populations,” he said, emphasizing the heterogeneity of children at risk of developing diabetes. Other disadvantages of the A1c test for which clinicians should be aware are listed in Table 2.
As to the value of measuring insulin, Zeitler recommended against it, saying it is a waste of time outside the research setting as it doesn’t provide any additional information about insulin resistance that is not already found on other labs. In addition, he cited problems with the test itself because it is not standardized and may measure insulin metabolites of uncertain significance, making it unreliable as a measure of insulin resistance. Also, he emphasized that the results of the test can be misleading as often insulin levels fall right before the onset of diabetes.
“I think there is a misunderstanding among pediatricians that they should be measuring insulin levels,” he said, “but it doesn’t tell you anything you need to know.”
Management of prediabetes
As to how to manage children at risk of developing diabetes, Zeitler emphasized one thing only: lose weight. “There is no magic to treating this,” he said. “It is weight loss.” The basic recipe to do this is to reduce caloric intake and increase caloric expenditure. Zeitler cited recommendations by an expert committee of the American Academy of Pediatrics (AAP) on the prevention, assessment, and treatment of overweight or obese children (Table 4).
Regarding the use of metformin, Zeitler emphatically discouraged its use, saying that there is no clear evidence for pharmacologic treatment of prediabetes in children. “A lot of people think they are supposed to [prescribe metformin], but there is no evidence supporting its use in kids,” he said.
Although some small studies suggest a minor benefit of metformin either alone or in conjunction with lifestyle interventions in select children, Zeitler underscored that the true benefit of metformin or any pharmacologic treatment of prediabetes in children needs to be weighed against the fact that most kids with high glucose or A1c levels will have spontaneous regression back to normal levels without any intervention.
“Progression rates of prediabetes are much different in children than in adults,” he said. “About 60% of kids with prediabetes will reverse on their own, so why would you start them on a drug?”
Unfortunately, Zeitler said, conducting a study to test the true benefit of metformin in children is almost impossible given this high incidence of spontaneous regression that would require a very large sample population.
Simple guide
To help pediatricians approach assessment and management of a child they suspect may have prediabetes, Zeitler offered a simple guide (Table 5). He underscored the need to avoid being too “glucose centric” and to recognize that prediabetes is frequently a transient disorder in children that may not require intervention. In addition, he stressed the importance of recognizing and evaluating the more common abnormalities associated with obesity, such as hypertension, hepatic steatosis, sleep disturbances, mood disorders, and other complications. Finally, he stressed the need to address obesity in all children through lifestyle intervention.
References:
1. Zeitler P. Not yet diabetes: Assessing and managing children at risk (F4019). Presented at: American Academy of Pediatrics National Conference and Exhibition; September 19, 2017; Chicago, IL.