The history of vaccination
Sharing how vaccinations first began and were implemented can be a useful tool in educating families of their importance.
Thousands of years ago, when variola (smallpox) virus emerged, it caused illness and deaths among humans across the globe. Although the earliest evidence of skin lesions resembling those of smallpox is found on faces of mummies in Egypt (1570-1085 BCE), the earliest written description of a disease resembling smallpox appeared in China in the fourth century.
Although the technique of variolation (deliberate inoculation of an uninfected person with the smallpox virus to prevent smallpox disease) had been practiced in China, India, parts of Africa and the Middle East before it was introduced into England and North America in the 1720s, it was Edward Jenner, a country doctor in Great Britain, who, by creating the smallpox vaccine, pioneered the modern day concept of vaccination.1 On May 14, 1796, Jenner took fluid from a cowpox blister on the hand of Sarah Nelmes, a dairy maid who had fresh cowpox lesions on her hands and scratched it onto the skin of 8-year-old James Phipps, who had never had cowpox or smallpox. James contracted cowpox; when his fever subsided, Jenner inoculated him with live smallpox, and the child never contracted smallpox.2 The use of vaccination spread rapidly in England; however, the United States was slower in its implementation of the vaccination. Nevertheless, severe smallpox outbreaks in the 1700s helped the public accept vaccination.3
In the early 1950s, an estimated 50 million smallpox cases occurred every year throughout the world. The disease killed about 300 million people worldwide in the 20th century.4 The risk of related death was reported to be 30%.5 Thanks to the success of the vaccine, the last natural outbreak of smallpox in the United States occurred in 1949, according to the Centers for Disease Control and Prevention (CDC). On May 8, 1980, the 33rd World Health Assembly declared the world free of smallpox.6 No cases have occurred since.
Almost 100 years after Jenner, French physician Louis Pasteur pioneered vaccine science by illustrating the phenomenon of attenuation. He demonstrated that disease could be prevented by infecting humans with weakened germs.7 His subsequent work on anthrax and rabies confirmed his hypothesis.7,8 In 1885, he used a vaccine to successfully prevent rabies in a child who had been bitten by a rabid dog, starting the era of modern immunization.9
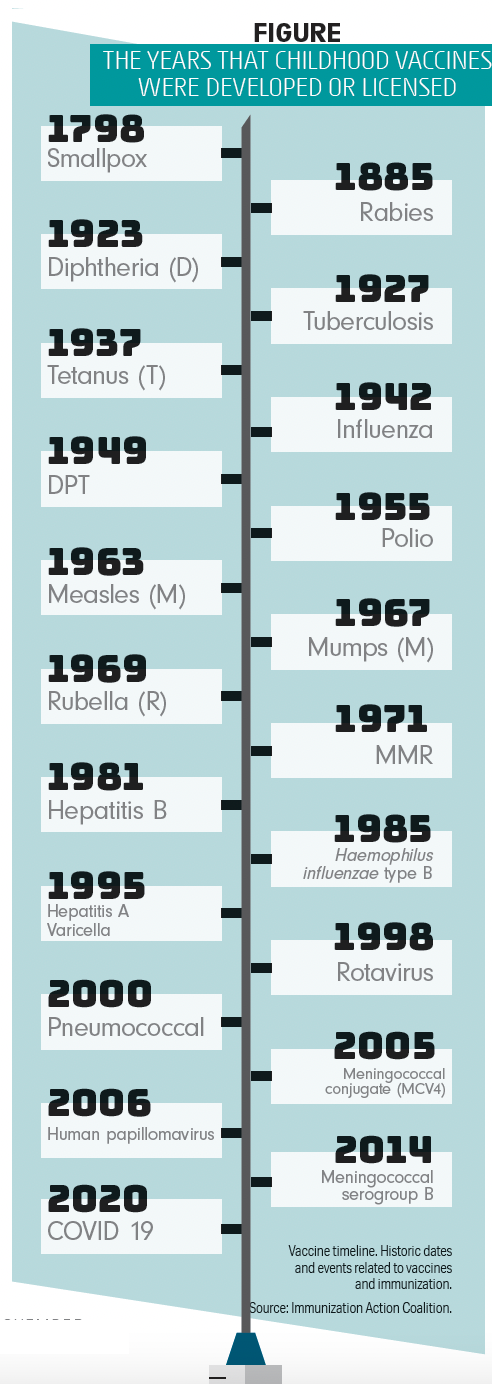
Figure
At its peak in the 1940s and 1950s, poliomyelitis (polio) killed and paralyzed more than half a million people worldwide every year. During the epidemic in the northeastern United States in 1916, more than 27,000 people were reported to have been paralyzed and 6000 died.10 The development of vaccines against polio (the formalin-inactivated poliovirus vaccine [IPV] by Jonas Salk in 1953 and the live-attenuated oral poliovirus vaccine [OPV] by Albert Sabin in 1956) was adopted throughout the United States in 1955 and 1961, respectively.10 Following use of the vaccine, the US incidence of paralytic polio decreased from 13.9 cases per 100,000 in 1954 to 0.8 cases per 100,000 in 1961.11 Because of the polio vaccination, reported cases of wild poliovirus decreased by over 99% since 1988, from an estimated 350,000 cases then to 33 reported cases in 2018, according to the World Health Organization. The polio vaccine saved millions of children worldwide from polio, and according to the CDC, polio was eliminated from the United States in 1979. It was clear that people at risk of infection were those who had never been vaccinated or had not received the recommended doses of the vaccine.
During the 1920s, 100,000 to 200,000 cases of diphtheria (140-150 cases per 100,000) and 13,000 to 15,000 deaths were reported each year.12 These figures dropped dramatically after implementation of a universal childhood vaccination program including diphtheria toxoid beginning in the late 1940s. From 1996 through 2018, 14 cases of diphtheria—an average of less than 1 case per year—were reported in the United States.12
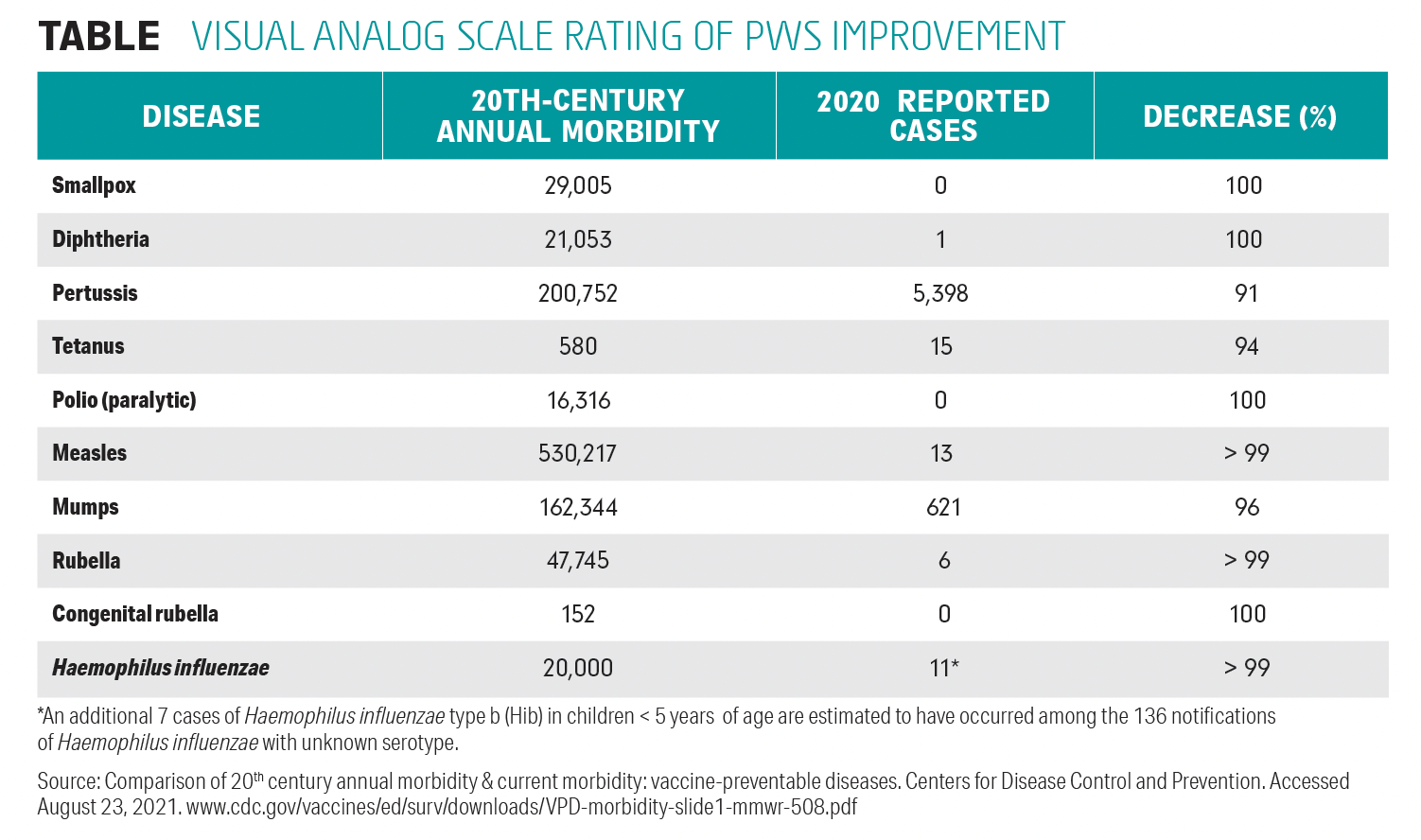
Table
In 1912, measles became a nationally notifiable disease in the United States, according to the CDC. In the 1950s, a decade before the measles vaccine became available in 1963, nearly all children got measles by the time they were 15 years old. It is estimated that measles affected 3 million to 4 million people in the United States each year with an estimated 400 to 500 deaths, 48,000 hospitalizations, and 1000 cases of encephalitis. A highly effective vaccination program is the reason measles was eliminated from the United States in 2000.
Presenting to parents
Reviewing the history of vaccination and showing parents a historical timeline (Figure) are strong tools for convincing them, especially those with vaccination hesitancy, of the safety and efficacy of childhood vaccines in preventing serious illness and death in children, as well as protecting the public.
Although adherence to childhood vaccination scheduled by age 24 months in the United States is high, pediatricians continue to be challenged by vaccine hesitancy. In my pediatric practice, I have presented historical facts regarding pre- and postvaccination morbidity and mortality reports to parents in my prenatal sessions. These presentations persuaded many, if not most, vaccine-hesitant parents to accept vaccination for their children. Having used this method successfully in my 50 years of pediatric practice, I recommend that pediatricians try to make a serious effort to present this information to parents (Table) to convince them that vaccines can safely prevent serious and deadly infections in their children and community.
References
1. Plotkin SA, ed. History of Vaccine Development. Springer; 2011. Accessed June 9, 2021. doi:10.1007/978-1-4419-1339-5
2. Willis NJ. Edward Jenner and the eradication of smallpox. Scott Med J. 1997;42(4):118-121. doi:10.1177/003693309704200407
3. Henry EH. Experience in Massachusetts and a few other places with smallpox and vaccination. Boston Med Surg J. 1921;185:221-228. doi:10.1056/NEJM192108251850802
4. Henderson DA. The eradication of smallpox—an overview of the past, present, and future. Vaccine. 2011;29:D7–D9. doi:10.1016/j.vaccine.2011.06.080
5. Kotar SL, Gessler JE. Smallpox: A History. McFarland & Company, Inc; 2013.
6. World Health Assembly, 33. Thirty-third World Health Assembly, Geneva, May 5-23, 1980: verbatim records of plenary meetings, reports of committees. World Health Organization. Accessed August 23, 2021, https://apps.who.int/iris/handle/10665/154894
7. Plotkin SA. Vaccines: past, present and future. Nat Med. 2005; 11(suppl 4):S5-S11. doi:10.1038/nm1209
8. Pasteur L, Chamberland C-E. Sur la vaccination charbonneuse. C.R. Acad. Sci. Paris. 1881; 92:1378-1383.
9. Centers for Disease Control and Prevention. Historical Perspectives A Centennial Celebration: Pasteur and the Modern Era of Immunization. Morb Mortal Wkly Rep. 1985;34(26)389-390.
10. Baicus A. History of polio vaccination. World J Virol 2012;1(4):108-114. doi:10.5501/wjv.v1.i4.108
11. Strebel PM, Sutter RW, Cochi SL, et al. Epidemiology of poliomyelitis in the United States one decade after the last reported case of indigenous wild virus-associated disease. Clin Infect Dis.1992;14(2):568–579. doi:10.1093/clinids/14.2.568
12. Centers for Disease Control and Prevention. Epidemiology and Prevention of Vaccine-Preventable Diseases, 11th Edition (The Pink Book). Updated April 15, 2019. Accessed August 23, 2021. http://www.cdc.gov/vaccines/Pubs/pinkbook/downloads/dip.pdf