Managing enuresis in primary care: Part 2
The continuation of this informative article addresses treatments for nocturnal enuresis, constipation, UTIs, and extraordinary daytime urinary frequency in children.
Table 6
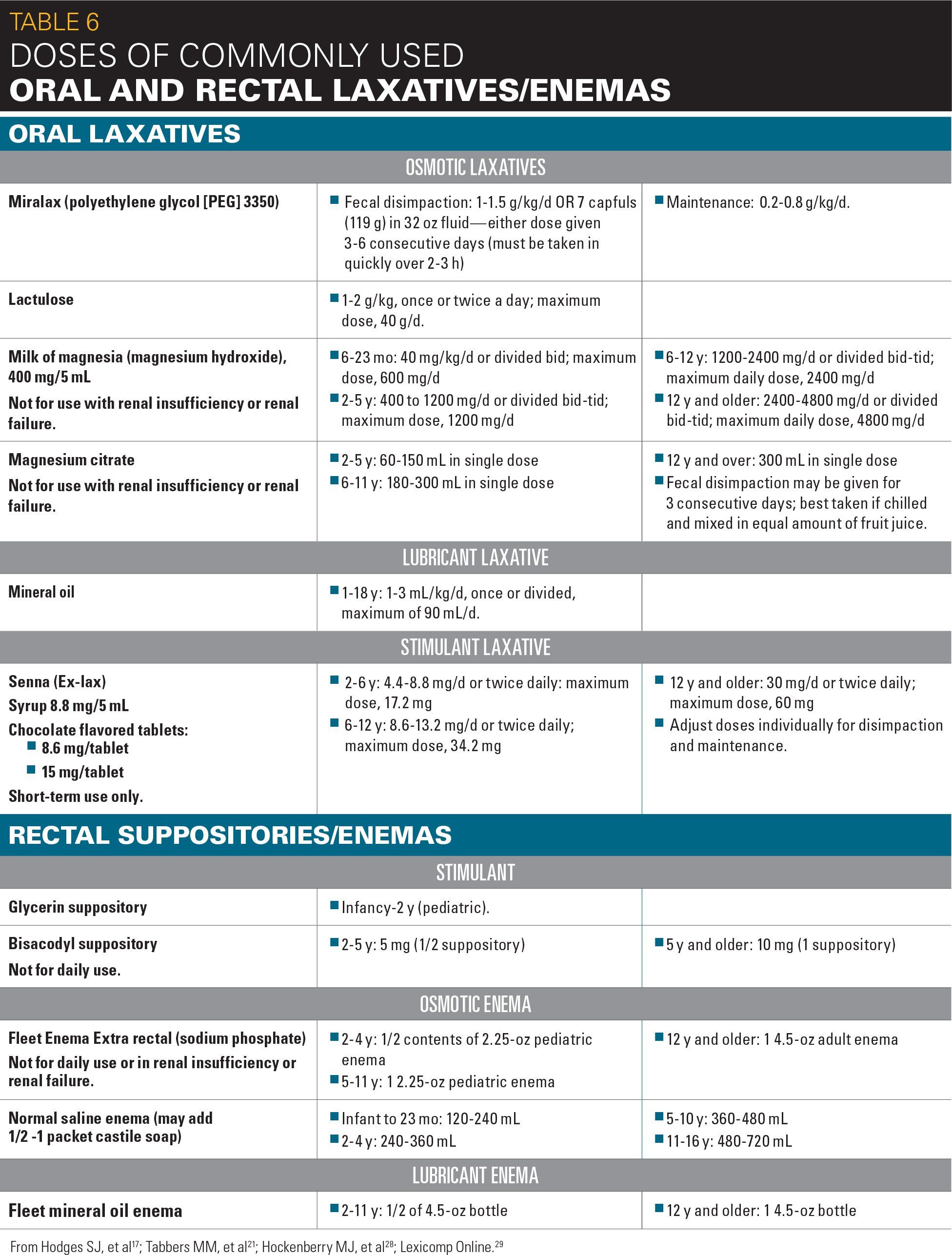
Table 7
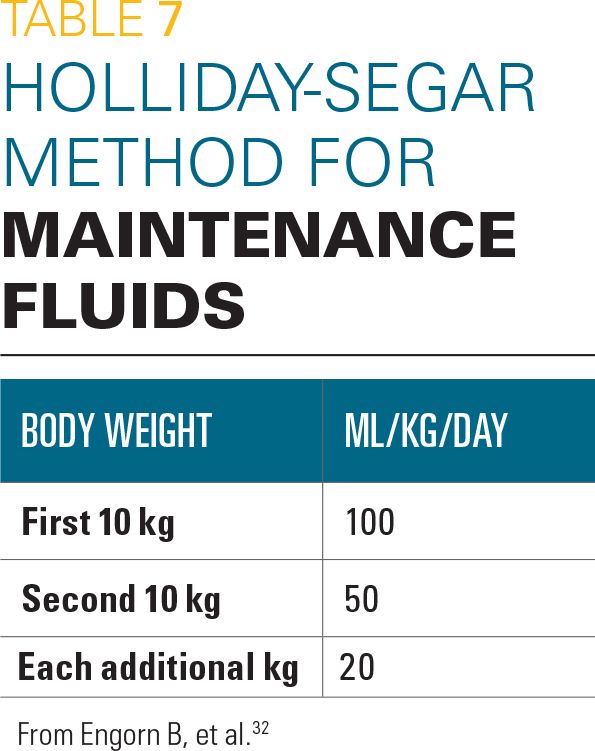
Figure 3
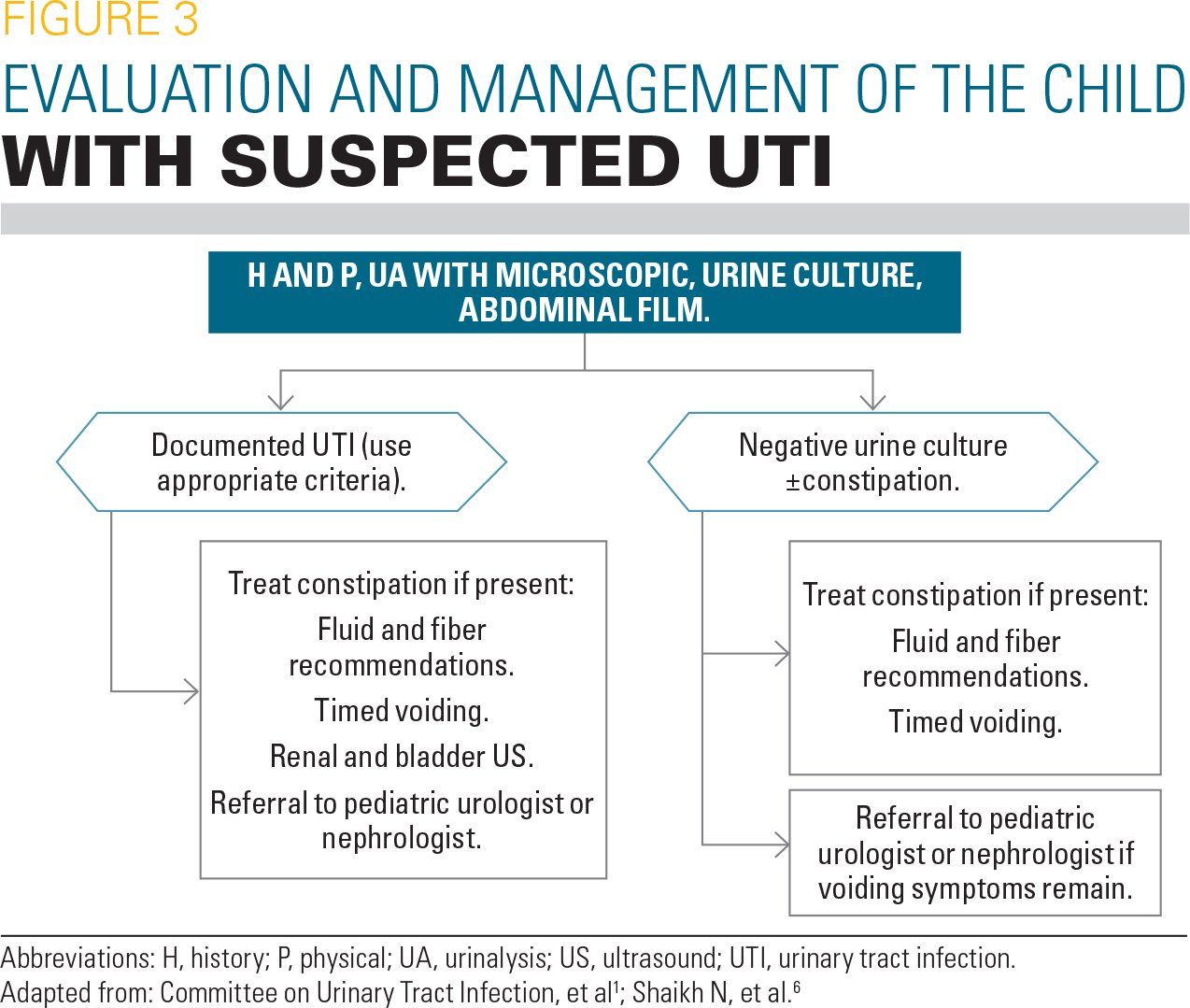
Table 8
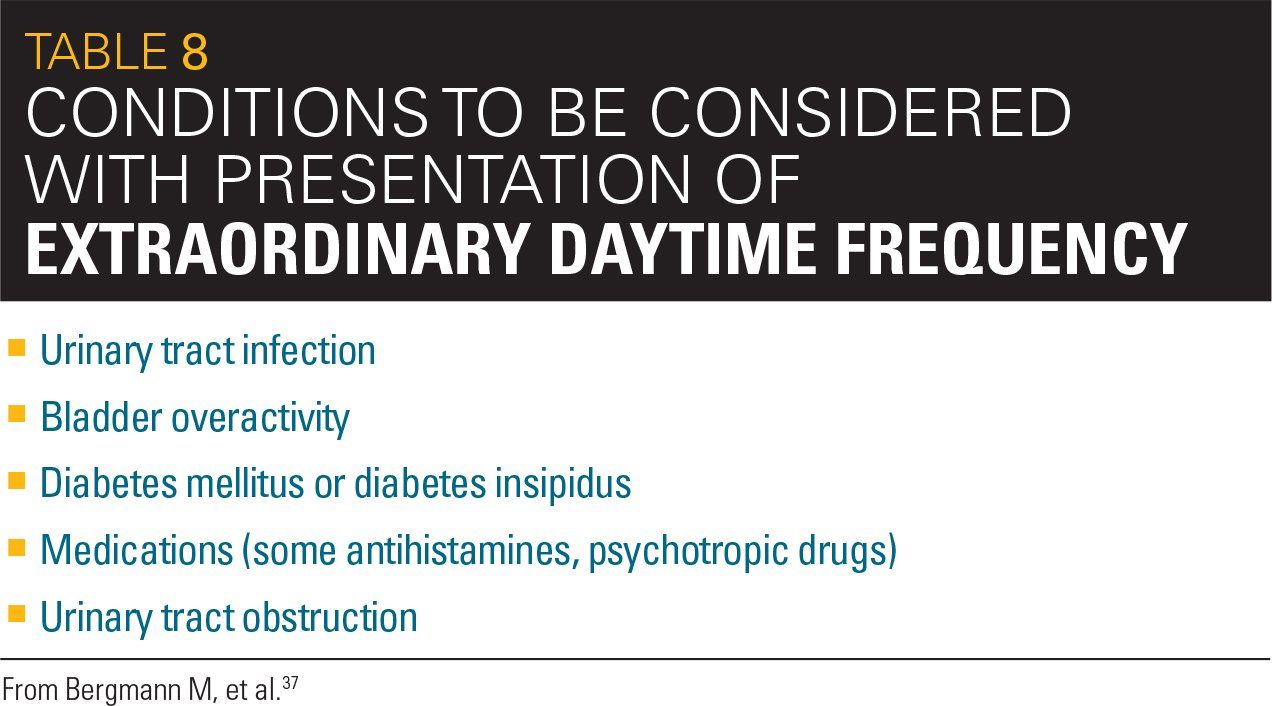
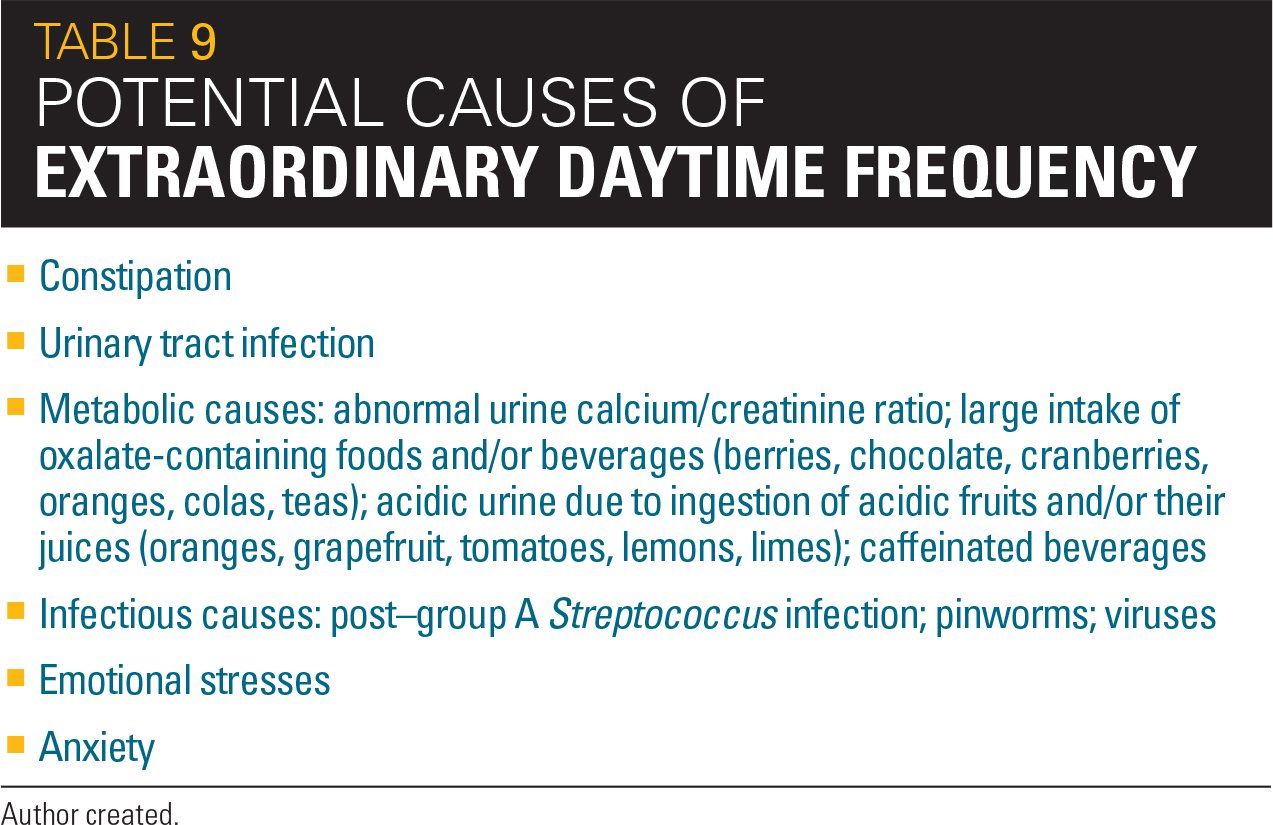
Table 9
Treatment of nocturnal enuresis
It is paramount to emphasize to the family that bedwetting is not the child’s fault, particularly when the parent conveys a feeling of blame or anger toward the child. It should be emphasized that punishments and shaming do not help. When the child is developmentally ready to work on the bedwetting, it is time to pursue intervention. Most often, this occurs when the child‘s social interactions are reduced because of the bedwetting, usually in the form of sleepovers.
Families differ in their goals for treatment, so this needs to be clarified at the outset. Some families want to reduce their workload, whereas others want the assurance that nothing is physically wrong with their child, or a family vacation or school trip may occur in the near future for which they want to prepare. The pediatric PCP may then explain that a carefully constructed program can be developed that may involve several methods of treatment, used in sequence or combination.3 It cannot be overemphasized that a long-term treatment plan needs to have the child’s involvement. In other words, the child needs to have the maturity and motivation to participate. It is also imperative that the family handle the bedwetting and its treatment in a positive fashion. Should negativity be demonstrated by family members, they should be counseled about the poor influence this attitude will have toward treatment and be encouraged to change their thinking.
Treatment of constipation
If constipation is diagnosed, a bowel cleanout is undertaken. Many PCPs initiate a bowel program with the family by starting with maintenance doses of laxatives. Quite frequently, the bowel program does not achieve its goals when begun in this manner. Parents report that with initiation of the laxative, the child was either stooling constantly, having bowel accidents, or that no change existed at all in bowel habits. Instead, the preferred method is to begin with a bowel cleanout. Only after the bowel is cleaned out appropriately will the maintenance laxative doses be effective (Table 617,21,28,29).
If a large stool load or balls of stool in the recto-sigmoid are identified on AXR, it is often a good idea to initiate the cleanout with enemas. When hard stool is present in the rectum, painful abdominal cramping with oral laxatives given by mouth can occur. Enemas can be in the form of a small volume Fleet enema, a glycerin or bisacodyl suppository, or a soap suds enema. It is important to explain to parents when purchasing a Fleet enema that different types are available. The PCP should specify the specific type he/she recommends (Table 6). When making recommendations, it is imperative to recognize any presence of renal disease.
Once the bowel cleanout phase has been accomplished, maintenance doses of laxatives are continued. The length of bowel therapy has not been agreed upon by pediatric gastroenterologists as a group. Certainly rectal distention and an abnormally large stool burden can develop over several months-to-years’ time prior to constipation being identified. Even after successful initiation of therapy, it is common for children to have relapses of constipation and require further cleanouts over time. One study showed that children diagnosed with functional constipation continued to have chronic constipation 3 to 12 years after initial diagnosis and treatment.30 In this author’s setting, clinicians recommend that maintenance laxative therapy continue for at least a year prior to weaning the doses.31 Whereas stimulant laxatives are not recommended for chronic use, osmotic and lubricant laxatives and bulking agents may be used long term.29
Other recommended treatments for constipation are adequate fluid and fiber intake. Fluid recommendations can be given based upon the Holliday-Segar maintenance fluid requirements (Table 7).32 Fiber intake recommendations are based upon the formula: age in years plus 5 grams equals the number of grams of fiber recommended per day up until the adult recommended amount of 25 grams to 35 grams/day.33 Current evidence does not support the use of fiber supplements.21 However, in children and adolescents who do not eat the recommended daily amount, fiber supplements such as fiber gummies, Benefiber, or fiber bars seem appropriate. Evidence does not support the use of probiotics in the treatment of childhood functional constipation. Anecdotal reports often do corroborate the successful use of probiotics and yogurt with active cultures (Bifidobacterium and Lactobacillus).
An important word of advice when discussing toileting habits with families is that children’s feet should be flat on the floor when using the toilet. Toilets in general are made for adults. If the child’s feet cannot be positioned flat on the floor comfortably when sitting on the toilet, a step stool or other device should be used. A child sitting on the toilet with dangling legs will be unable to push to have a bowel movement and may not be able to sufficiently evacuate.
It has been shown that at least 50% of children with bladder and bowel dysfunction will improve with successful constipation treatment and behavioral management.34 For those with nocturnal enuresis, the pattern of fluid intake is important so that the majority of fluids are consumed early in the day rather than late afternoon and evening. Many children are not in the habit of drinking the majority of fluids early in the day as school activities do not encourage this behavior. Teachers may be hesitant to allow children to use the bathroom when needed, so that children learn not to drink during school hours. This encourages the majority of fluids to be consumed late in the day, thus producing a good deal of urine during sleeping hours.
In contrast, the general recommendation is for fluid intake to be completed 2 to 3 hours prior to bedtime. The child should void at bedtime, so the night starts with an empty bladder. Using the maintenance fluid formula and giving the family written recommendations for a schedule of timing of fluid intake is helpful. It is also beneficial to write notes for water bottle and bathroom privileges to give to teachers.
Other treatments for nocturnal enuresis
When treatment of bowel issues and behavior modification techniques do not result in resolution of bladder issues, other therapies are suggested. One therapy is the wetness alarm. Wetness alarms have been shown to give high cure rates for nocturnal enuresis. The alarm consists of a sensor is worn on the underwear that causes an alarm to sound or vibrate when wetness is sensed. The wearer is then instructed to immediately get out of bed and go to the bathroom. At the initiation of alarm use, the child will often awaken to a totally wet bed. As more time passes with the use of the alarm, the child may awaken in the middle of urination and then eventually prior to its initiation. The conditioning occurs when the child awakens to the sensation of a full bladder and associates that sensation with the alarm.
It has been shown to take approximately 12 to 16 weeks of nightly use for the wetness alarm to be effective. Often the parent needs to get up with the child, particularly during the initial use of the alarm. The child may not respond to the alarm without parental assistance. The child needs to be awakened so that he/she realizes what is occurring for the conditioning to occur. As can be seen from this description, the use of a wetness alarm requires a motivated child and family member(s). It is generally not recommended for children aged younger than 8 years. Enuresis alarms can be obtained from online sites such as bedwettingstore.com and PottyMD.com. Insurance typically does not cover their cost.
One medication that has been used for children and adolescents for a “quick fix” for bedwetting is desmopressin (DDAVP). It is given for short periods, such as vacations, sleepovers, camping trips, or school trips. It works by increasing water permeability in the renal collecting tubules, which results in increased water reabsorption that causes decreased urine production.29 Its duration of action is estimated at 6 to 14 hours. Recommended dosing is to start at 0.2 mg and work up to a maximum of 0.6 mg nightly. It is recommended for use in nocturnal enuresis from age 6 years through adolescence. It is also recommended to keep fluid intake to a minimum in the hour prior to administration until at least 8 hours later. Desmopressin also may be used for long-term treatment of nocturnal enuresis, but is not considered a first-line therapy.
Other medications that are used for nocturnal enuresis are anticholinergics and the tricyclic antidepressant imipramine. Neither are used as first-line treatment. Some anticholinergics that are used are oxybutynin, tolterodine, and hyoscyamine. These medications suppress detrusor overactivity that can be present in monosymptomatic nocturnal enuresis. Imipramine has anticholinergic effects as well as a stimulant effect that is thought to lighten the level of sleep, making arousal from sleep easier. It is used in much smaller doses when treating nocturnal enuresis, as compared with depression. It may be prescribed nightly for 2 to 4 months, then weaned gradually by administering every 2, then every 3 days over the next 3 to 4 months to reduce risk of relapse.26 If imipramine is prescribed, special care must be taken for its storage at home as it is highly lethal when taken in overdose. There is no known specific antidote for its toxicity and death is usually the result of cardiac arrhythmia and cardiovascular collapse.
Urinary tract infections
It is necessary for a UTI to be culture proven to determine appropriate treatment and subsequent diagnostic evaluation (Figure 31,6).
The diagnosis of urinary tract infection cannot be made on symptomatology alone. A properly collected urine specimen for a macroscopic and microscopic urinalysis is the first step. It has become common practice for some primary care offices to obtain a midstream urine specimen from toilet-trained children and perform only a reagent test strip (dipstick) in the office in an attempt to diagnose a UTI. As discussed previously, this practice reveals many false-positive and false-negative results when checking for nitrites and leukocyte esterase. The urine must be sent to a lab for urine culture. Growth of any single organism from a midstream urine that is at least 50,000 colony forming units per high-power field (CFU/HPF) is indicative of a UTI. Bacterial counts of at least 10,000 CFU/HPF obtained by a catheter or any growth obtained by suprapubic tap are indicative of a UTI.35
A urine culture obtained by bagged specimen is not reliable unless it reveals negative results. Any growth of any bacteria in a bagged specimen renders the results unusable.36 Therefore, a bagged urine specimen should not be performed in a febrile, symptomatic child. The only reliable result of a bagged specimen is a negative one.
Children who exhibit daytime symptoms and incontinence and/or UTIs will benefit from a recommendation for adequate fluid intake, a recommended fluid intake schedule, and a recommended voiding schedule in which voiding occurs at a minimum of 5 times daily. Vibrating watches at a reasonable cost that are attractive to children can be obtained through PottyMD.com or bedwettingstore.com. Their alarms can be set to coincide with appropriate times during the school day for the child to take bathroom breaks. Reducing or eliminating acidic fruits and their juices (orange, grapefruit, tomato, lemon, lime) and caffeine and chocolate also may help, although much of this evidence is anecdotal.
When to image
If the clinician discovers findings of significant irritative voiding symptoms, interrupted urinary flow, urinary hesitancy or straining to void, daytime wetting, or UTI, urologic imaging can be undertaken. The PCP may initiate a workup with a renal and bladder US, which may diagnose structural abnormalities and determine bladder emptying. A voiding cystourethrogram (VCUG) also may be in order. Although the 2011 American Academy of Pediatrics (AAP) guidelines for diagnostic evaluation of the urinary tract after a first febrile UTI do not recommend a VCUG if the renal US is normal, many pediatric urologists are in disagreement with this recommendation. Many physicians believe that serious flaws existed in the interpretation of the data that was used to make this recommendation. Thus, many pediatric specialists recommend obtaining a VCUG after a first febrile UTI, particularly in a child aged younger than 4 years when the developing kidney is most prone to scarring. The data on this important topic continue to accumulate.
When to refer
A referral to a pediatric urologist or nephrologist can be made depending upon local referral practices. When this referral is made, the diagnostic images must be available, not just the written report. Children who present with monosymptomatic nocturnal enuresis or non-monosymptomatic nocturnal enuresis who do not improve with standard therapies also should be referred. So should children with UTIs despite treated constipation. Physical findings of occult spinal dysraphism (lower lumbar spine abnormalities) may be referred to a pediatric neurosurgeon. For children who have evidence of nocturnal enuresis and enlarged tonsils and signs of sleep apnea, a referral to a pediatric ears/nose/throat (ENT) or sleep specialist can be made. Sleep apnea can be associated with an increased production of urine overnight. When constipation is refractory with continued attempts at cleanout and treatment, referral to a pediatric gastroenterologist is recommended.
Extraordinary daytime urinary frequency
Another urinary disorder that deserves explanation is extraordinary urinary frequency, or pollakiuria. This disorder can begin with an abrupt or more gradual onset of urinary frequency of extreme proportion. Some children, generally in the age range of 3 to 7 years, will urinate small amounts as often as every 5 to 10 minutes. Many will exhibit such a strong urge that they cannot leave the toilet. When parents finally get them off the toilet, many return almost immediately or begin to cry due to discomfort. Children may spend nearly their entire day on the toilet. Some may even drink less fluids in an attempt to help their problem. It is important to take a good history and perform a physical exam. The children do not generally have daytime incontinence in association with the frequency. To rule out organic disease, potential conditions that deserve consideration are listed in Table 8.37
Should any of the factors be present that are listed in Table 9, appropriate diagnostic testing should be undertaken. To many PCPs, this may seem like such a benign problem that parents are advised to ignore it, or clinicians may advise that the children are merely vying for their parents’ attention. Parents also may be told that the children just like to visit bathrooms in various places. To the family, this problem is not benign. The child may be unable to leave the house for even a few minutes, which severely limits the family’s ability to accomplish day-to-day activities and can interfere with schooling. The symptoms can last for days to weeks prior to being referred to a specialist. Parents bring their children to the pediatric urology specialist’s office in total frustration, often at their wits’ end. In the past, specialists advised that extreme urinary frequency began as the result of psychosocial problems or emotional stress. Whereas such issues can be involved, it is a good idea to sort out other potential accompanying issues, in particular UTI and constipation.
Should a UTI and/or constipation be present, they should be treated appropriately. Families may be counseled about other potential causes of urinary frequency including those listed in Table 8. Potential stressors and worries should be identified, being cognizant of questioning the children as well as the parents. Children may reveal stressors of which the parents may not be aware. If so identified, they can be discussed and referrals made if appropriate. Other recommendations to treat urinary frequency are a liberal intake of fluids, in particular, water. Very concentrated urine may irritate the bladder further. Should the above treatments fail, referral to a pediatric specialist is in order.
Summary
The pediatric PCP can become comfortable with the evaluation and early treatment of enuresis, constipation, and UTIs. The treatment of constipation may ameliorate or resolve many wetting problems and should be attempted prior to referral. Daytime incontinence also may benefit from the use of timed voiding and adequate fluid intake. Nocturnal enuresis may show improvement as well using these techniques in addition to fluid restrictions late in the day and voiding at bedtime.
It is helpful to understand the psychologic effects of nocturnal enuresis on children and the limitations of their voluntary control of the problem. Using quantified criteria, particularly in the diagnosis of UTIs, will assist the PCP to correctly manage UTIs and recommend subsequent testing. In the long run, children and families will benefit from the pediatric PCP providing care of the child with urologic issues and making referrals for lack of response to treatment earlier rather than later.
References:
1. Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128(3):595-610.
2. Tu ND, Baskin LS, Arnhym AM. Nocturnal enuresis in children: etiology and evaluation. UpToDate. Available at: https://www.uptodate.com/contents/nocturnal-enuresis-in-children-etiology-and-evaluation. Updated November 15, 2017. Accessed March 14, 2018.
3. Tu ND, Baskin LS. Nocturnal enuresis in children: management. UpToDate. Available at: https://www.uptodate.com/contents/nocturnal-enuresis-in-children-management. Updated October 19, 2017. Accessed March 14, 2018
4. Allen HA, Austin JC, Boyt MA, Hawtrey CE, Cooper CS. Initial trial of timed voiding is warranted for all children with daytime incontinence. Urology. 2007;69(5):962-965.
5. Hagstroem S, Rittig N, Kamperis K, Mikkelsen MM, Rittig S, Djurhuus JC. Treatment outcome of day-time urinary incontinence in children. Scand J Urol Nephrol. 2008;42(6):528-533.
6. Shaikh N, Hoberman A. Urinary tract infections in infants and children older than one month: clinical features and diagnosis. UpToDate. Available at: https://www.uptodate.com/contents/urinary-tract-infections-in-infants-and-children-older-than-one-month-clinical-features-and-diagnosis?search=urinary-tract-infections-in-infants-and-children-older-than-one-month:clinical-features-and-diagnosis&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. Updated October 5, 2017. Accessed March 14, 2018.
7. Cederblad M, Nevéus,T, Ahman A, Osterlund Efraimsson E, Sarkadi A. “Nobody asked us if we needed help”: Swedish parents’ experiences of enuresis. J Pediatr Urol. 2014;10(1):74-79.
8. Moffatt ME, Kato C, Pless IB. Improvements in self-concept after treatment of nocturnal enuresis: randomized controlled trial. J Pediatr. 1987:110(4):647-652.
9. Longstaffe S, Moffatt ME, Whalen JC. Behavioral and self-concept changes after six months of enuresis treatment: a randomized, controlled trial. Pediatrics. 2000;105 (4 pt 2): 935-940.
10. Can G, Topbas M, Okten A, Kizil M. Child abuse as a result of enuresis. Pediatr Int. 2004;46(1):64-66.
11. Butler R, McKenna S. Overcoming parental intolerance in childhood nocturnal enuresis: a survey of professional opinion. BJU Int. 2002;89(3):295-297.
12. Ferrera P, Di Giuseppe M, Fabrizio GC, et al. Enuresis and punishment: the adverse effects on child development and on treatment. Urol Int. 2016;97(4):410-415.
13. Al-Zaben FN, Sehlo MG. Punishment for bedwetting is associated with child depression and reduced quality of life. Child Abuse Negl. 2015;43:22-29.
14. Yang S, Chua ME, Bauer S, et al. Diagnosis and management of bladder bowel dysfunction in children with urinary tract infections: a position statement from the International Children’s Continence Society. Pediatr Nephrol. October 3, 2017. Epub ahead of print.
15. Bloom DA, Seeley WW, Ritchey ML, McGuire EJ. Toilet habits and continence in children: an opportunity sampling in search of normal parameters. J Urol. 1993:149(5):1087-1090.
16. Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization committee of the International Children’s Continence Society. Neurourol Urodyn. 2016;35(4): 471-481.
17. Hodges SJ, Anthony EY. Occult megarectum-a commonly unrecognized cause of enuresis. Urology. 2012;79(2):421-424.
18. O’Regan S, Yazbeck S, Hamberger B, Schick E. Constipation a commonly unrecognized cause of enuresis. Am J Dis Child. 1986;140(3):260-261.
19. Lewis, SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920-924.
20. Benninga MA, Tabbers MM, van Rijn RR. How to use a plain abdominal radiograph in children with functional defecation disorders. Arch Dis Child Educ Pract Ed. 2016;101(4):187-193
21. Tabbers MM, DiLorenzo C. Berger MY, et al; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition; North American Society for Pediatric Gastroenterology. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258-274.
22. Holmes, EB. Ionizing radiation exposure with medical imaging. Medscape. Available at: https://emedicine.medscape.com/article/1464228-overview. Updated April 23, 2015. Accessed March 14, 2018.
23. Leech SC, McHugh K, Sullivan PB. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol. 1999 29(4):255-258.
24. Modin L, Walsted AM, Rittig CS, Hansen AV, Jakobsen MS. Follow-up in childhood functional constipation: a randomized, controlled clinical trial. J Pediatr Gastroenterol Nutr. 2016;62(4):594-599.
25. Hatori R, Tomomasa T, Ishige T, Tatsuki M, Arakawa H. Fecal retention in childhood: evaluation on ultrasonography. Pediatr Int. 2016;59(4):462-466.
26. Strasinger SK, Di Lorenzo MS. Urinalysis and Body Fluids. 6th ed. Philadelphia, PA: F.A. Davis Company; 2014.
27. Mundt LA, Shanahan K. Graff’s Textbook of Urinalysis and Body Fluids. 3rd ed. Philadelphia, PA: Wolters Kluwer; 2016.
28. Hockenberry MJ, Wilson D, Rodgers CC. Wong’s Essentials of Pediatric Nursing. 10th ed. St. Louis, MO: Elsevier Mosby; 2013.
29. Lexicomp Online. Pediatric and Neonatal Lexi-Drugs. Hudson, OH: Wolters Kluwer. Accessed March 14, 2018.
30. Loening-Baucke V. Constipation in early childhood: patient characteristics, treatment, and long-term follow up. Gut. 1993;34(10):1400-1404.
31. Kendall R. The Poo in You-Constipation and Encopresis Educational Video. YouTube. Available at: https://www.youtube.com/watch?v=SgBj7Mc_4sc. Published November 11, 2014. Accessed March 14, 2018.
32. Engorn B, Flerlage J. The Harriet Lane Handbook. 20th ed. Philadelphia, PA: Elsevier Saunders; 2015.
33. Williams CL, Bollella M, Wynder EL. A new recommendation for dietary fiber in childhood. Pediatrics. 1995;96(5 pt 2):985-988.
34. dos Santos J, Varghese A, Williams K, Koyle, MA. Recommendations for the management of bladder bowel dysfunction in children. Pediatr Therapeut. 2014;4;191.
35. Tullus K. Low urinary bacterial counts: do they count? Pediatr Nephrol. 2016;31(2):171-174.
36. Etoubleau C, Reveret M, Brouet D, et al. Moving from bag to catheter for urine collection in non-toilet-trained children suspected of having urinary tract infection: a paired comparison of urine cultures. J Pediatr. 2009:154(6):803-806.
37. Bergmann M, Corigliano T, Ataia I, et al. Childhood extraordinary daytime urinary frequency-a case series and a systematic literature review. Pediatr Nephrol. 2009;24(4):789-795.
Omalizumab outperforms oral immunotherapy in treating multi-food allergy
March 27th 2025A new clinical trial has found that omalizumab (Xolair; Genetech, Novartis) is more effective than oral immunotherapy (OIT) in treating multi-food allergy in individuals with severe allergic reactions to small amounts of common food allergens.