Are These New Erythematous Papules Related to the Patient's Hypopigmented Macules?
An 8-year-old girl presents with a 1-year history of the progressive development of multiple 5- to 8-mm hypopigmented macules all over her body. Her parents do not recall any other skin changes, and no other skin changes are evident on presentation.
Case: An 8-year-old girl presents with a 1-year history of the progressive development of multiple 5- to 8-mm hypopigmented macules all over her body (A).

Her parents do not recall any other skin changes, and no other skin changes are evident on presentation.
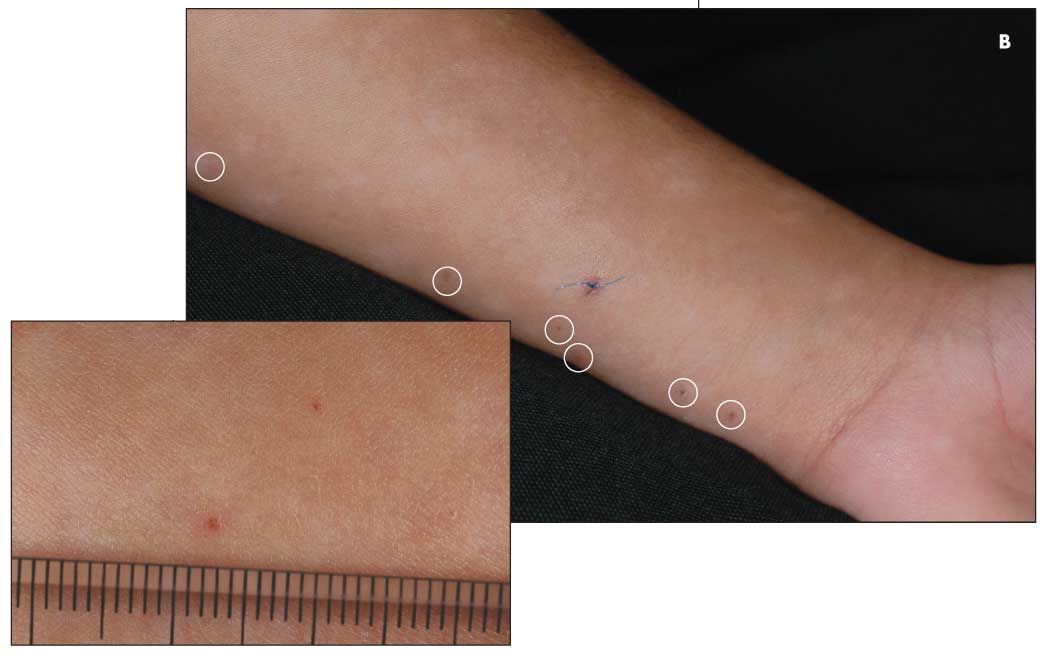
She returns a month later; at this visit, several 1-mm erythematous papules are noted on her forearm (B). These are biopsied.
Will the biopsy results shed light on the cause of the hypopigmented macules as well as the new papules on her forearm?
(Answer on next page.)
Yes; the new papules are part of an inflammatory disorder, and the hypopigmented macules are postinflammatory lesions.
The surprise diagnosis in this girl was pityriasis lichenoides et varioliformis acuta (PLEVA). PLEVA is thought to be a manifestation of a benign process that results from perivascular lymphocytic infiltration that extends into the epidermis, producing inflammation and occasionally necrosis. In my Dermclinic case in the April 2009 issue of CONSULTANT FOR PEDIATRICIANS,1 I mentioned that there are 2 forms of this process: PLEVA is the acute form; the chronic form is pityriasis lichenoides chronica (PLC). Both forms are generally self-limited. Topical corticosteroids and oral antibiotics (erythromycin and, where age-appropriate, tetracycline) are usually prescribed; however, the results are often disappointing.
The lesson to be learned from this girl's presentation is always to follow up with patients who present with unexplained pigmentary changes and/or cutaneous scarring, since these findings are often secondary events. Here, the patient's hypopigmented macules (C) were what remained after the initial PLEVA papules resolved.

Unfortunately, there is no effective therapy for this girl's postinflammatory hypopigmentation other than time; repigmentation will likely occur over the course of the next few years. To prevent further hypopigmentation, treatment of the primary process, in this case PLEVA, is required.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.