Child With Fever and Neck Pain
Ill-appearing 4-year-old girl with high-grade fever, without chills or rigors, and cough of 3 days’ duration. She also had a sore throat and was unable to move her neck because of pain. No history of rhinorrhea, difficulty in breathing, vomiting, or diarrhea. She had had tonsillitis 2 weeks earlier that was treated with a 1-week course of amoxicillin. Medical history otherwise unremarkable. Immunizations up-to-date.

HISTORY
Ill-appearing 4-year-old girl with high-grade fever, without chills or rigors, and cough of 3 days' duration. She also had a sore throat and was unable to move her neck because of pain. No history of rhinorrhea, difficulty in breathing, vomiting, or diarrhea. She had had tonsillitis 2 weeks earlier that was treated with a 1-week course of amoxicillin. Medical history otherwise unremarkable. Immunizations up-to-date.
PHYSICAL EXAMINATION
Heart rate, 126 beats per minute; respiration rate, 30 breaths per minute; temperature, 39.5°C (103°F); blood pressure, 100/60 mm Hg. Throat examination revealed pharyngeal injection; slightly enlarged tonsils, without any exudates; and nondeviated uvula. Child had torticollis, with neck held mainly to the right, and significant nontender bilateral cervical lymphadenopathy. No drooling, hoarseness of voice, or trismus noted. Remaining examination findings normal.
LABORATORY FINDINGS
White blood cell count of 25,500/μL, with 5% bands and 80% neutrophils. Results of a rapid streptococcal antigen test, negative. Throat and blood culture results pending.
RADIOGRAPHIC STUDIES
Soft tissue radiograph and CT scans of the neck are shown.
“WHAT'S YOUR DIAGNOSIS?”
Answer on Next Page

ANSWER:RETROPHARYNGEAL ABSCESS
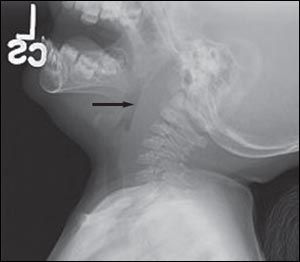
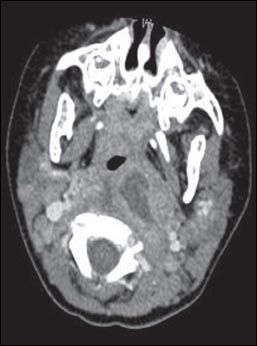
Figure 1 – Soft tissue radiograph of the neck of a 4-year-old girl with retropharyngeal abscess shows increased depth of the prevertebral space.
Retropharyngeal abscess results from suppuration of retropharyngeal lymphadenitis. It occurs most commonly in children between the ages of 2 and 4 years; however, other age-groups, including neonates, may be affected.1
ETIOLOGY
The retropharyngeal space contains lymph nodes that drain the nasopharynx, adenoids, posterior paranasal sinuses, middle ear, and eustachian tube. Infections in these areas (eg, pharyngitis, tonsillitis) may lead to suppurative adenitis of the retropharyngeal lymph nodes. Retropharyngeal infections progress from cellulitis to organized phlegmon to mature abscess. Retropharyngeal abscesses in children are often from nontraumatic causes, whereas regional trauma, foreign body, and complication of a procedure (eg, endoscopy) are more common causes in adults.2
Most retropharyngeal abscesses are polymicrobial. Causative organisms are primarily Streptococcus pyogenes, Staphylococcus aureus, and anaerobes. Haemophilus species are found on occasion.
CLINICAL PRESENTATION
Children with retropharyngeal abscess appear ill with high fever. Additional presenting symptoms include dysphagia; odynophagia; drooling with decreased oral intake; restricted neck movement, particularly with neck extension; change in voice (muffled or "hot potato" voice); neck swelling or mass; and trismus.3 Respiratory distress and stridor are uncommon in children.
EVALUATION
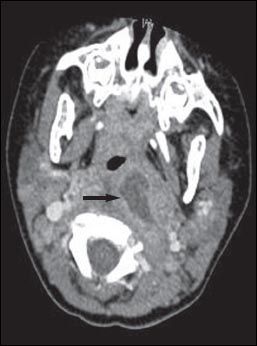

Figure 2 – A CT scan of the neck of the 4-year-old patient shows a retropharyngeal abscess.
The initial step in the evaluation of the child with potential deep neck space infection is an assessment of the degree of upper airway obstruction. Anxious, illappearing children with drooling must be monitored closely and an emergent artificial airway established, if necessary. If it is not clear whether the patient has retropharyngeal infection, epiglottitis, or other deep neck space infection, imaging or examination in the operating room may be necessary.
Physical findings. Examination of the oropharynx may be limited if the child is unable to open his or her mouth widely. When visualization is adequate, it may be possible to see midline or unilateral swelling of the posterior pharyngeal wall and pharyngeal injection, as in this patient. Tender anterior cervical lymphadenopathy is frequently present. A neck mass may be palpable if the infection has spread to the lateral pharyngeal space.
Laboratory results. The white blood cell count is usually increased, with a predominance of neutrophils and bands. It is important to obtain blood cultures for both anaerobic and aerobic bacteria and a throat culture for group A streptococci. Results of a rapid streptococcal antigen test may be helpful. If drainage is performed, pus should be cultured for aerobic and anaerobic bacteria.
Imaging studies. In patients with no signs of airway compromise and in whom the suspicion for retropharyngeal abscess is low, a lateral neck radiograph may be the initial study. When the suspicion is high, a CT scan with contrast is the preferred study.
When retropharyngeal infection (cellulitis or abscess) is present, the depth of the prevertebral space is increased (Figure 1) compared with the anteroposterior measurement of the adjacent vertebral body. Alternatively, the retropharyngeal space is considered pathologically widened when it is greater than 7 mm at C2 or 14 mm at C6 in children, and greater than 22 mm at C6 in adults.4 In some cases, a radiopaque foreign body, soft tissue mass, air-fluid level, or gas is visualized in the prevertebral area. A lateral view obtained during inspiration, with the neck held in normal extension, helps avoid false widening of the retropharyngeal space. False widening of the retropharyngeal space also may be caused by crying, particularly in infants.
CT of the neck with intravenous contrast provides ideal delineation of the retropharyngeal area. A CT scan may show an abscess (Figure 2), with extension to contiguous spaces in the neck or chest, and can differentiate between retropharyngeal abscess and cellulitis. It can also show loculations and the position of the carotid artery and internal jugular vein in relation to the infectious process, which helps guide the surgical approach in patients who require drainage.
DIFFERENTIAL DIAGNOSIS
The differential diagnosis of retropharyngeal infection includes epiglottitis, peritonsillar abscess, croup, bacterial tracheitis, parapharyngeal abscess, foreign body, angioedema or anaphylaxis, and tumor (lymphangioma or hemangioma).
MANAGEMENT
Children with suspected retropharyngeal infection require hospitalization and treatment in consultation with an otolaryngologist. Particular attention must be paid to maintenance of the airway. Intubation or, less commonly, tracheostomy may be necessary in patients with respiratory compromise. Immediate surgical drainage is necessary in patients with airway compromise and in those with a large (greater than 2-cm) hypodense area on the CT scan.5
Empiric antibiotic therapy should cover S pyogenes, S aureus (including methicillin-resistant S aureus), and respiratory anaerobes; this can be amended on the basis of the culture results. Antimicrobial therapy given early in the disease process (cellulitis or phlegmon) may prevent progression, precluding the need for surgery. Parenteral treatment is maintained until the patient is afebrile and clinically improved. This is followed by a 14- day course of oral therapy. Order a CT scan with contrast for patients who do not respond within 24 to 48 hours after initiation of antibiotic therapy.
Untreated or undertreated retropharyngeal abscess may lead to mediastinitis and spread to spinal and intracranial areas. Other complications include septicemia; aspiration pneumonia, if the abscess ruptures; internal jugular vein thrombosis; and jugular vein suppurative thrombophlebitis (Lemierre syndrome).2
This patient received intravenous ceftriaxone and clindamycin empirically. She underwent drainage of the abscess. Pus culture was positive for S aureus, sensitive to clindamycin; throat and blood cultures were negative. She recovered uneventfully.
References:
REFERENCES:
1.
Goldstein NA, Hammerschlag MR. Peritonsillar, retropharyngeal, and parapharyngeal abscesses. In: Feigin RD, Cherry JD, Demmler-Harrison GJ, Kaplan SL, eds.
Textbook of Pediatric Infectious Diseases
. 6th ed. Philadelphia: Saunders; 2009:177.
2.
Craig FW, Schunk FE. Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management.
Pediatrics
. 2003;111:1394-1398.
3.
Page NC, Bauer EM, Lieu JE. Clinical features and treatment of retropharyngeal abscess in children.
Otolaryngol Head Neck Surg
. 2008;138:300-306.
4.
Philpott CM, Selvadurai D, Banerjee AR. Paediatric retropharyngeal abscess.
J Laryngol Otol
. 2004;118:919-926.
5.
Coulthard M, Isaacs D. Retropharyngeal abscess.
Arch Dis Child
. 1991;66: 1227-1230.