Seasonal allergies: What every pediatrician needs to know
It’s springtime, which means flowers are blooming and children sneezing. Here’s a quick refresher on seasonal allergy diagnoses and prescriptions.
During the spring, exposure to pollen can trigger a range of symptoms in the nose, eyes, throat, lungs, or skin. Patients may refer to these spring allergy symptoms as hay fever. The classic presentation includes rhinorrhea, nasal congestion, sneezing, and/or nasal itching which are characteristic of allergic rhinitis, or watery itching eyes which are characteristic of allergic conjunctivitis.1 In addition, patients may present with cough secondary to postnasal drip or cough equivalent asthma, as allergens including pollen are common triggers for asthma.2 Finally, patients may present with a sore throat from postnasal drip or oral itching from pollen food allergy syndrome due to cross reactivity between pollen and food.3
Patients with spring allergies may have common physical exam findings:
- clear nasal discharge
- pale, boggy nasal mucosa
- turbinate hypertrophy
- adenoid facies (mouth breathing)
- allergic shiners (dark circles around the eyes)
- allergic salute (habit of wiping or rubbing the nose)
- allergic crease (dark line at the bend of the nose)
- rash around the eyes due to rubbing (periorbital atopic dermatitis)1,4,5
Allergic rhinitis is the most common cause of chronic nasal congestion affecting 7.2% of US children annually. According to a 2014 National Health Interview Survey, 5.2 million children reported hay fever in the past 12 months.6
Children with certain risk factors are more likely to have allergic rhinitis. These include a family history of atopy, and other allergic diseases such as asthma and atopic dermatitis.1,7
Allergic rhinitis symptoms can be triggered by one or more allergens. When the body is exposed to a substance it perceives as foreign, such as pollen, it responds by producing specific immunoglobulin E (IgE) antibodies. The antigen or allergen binds to the antibodies that cross link on allergy cells, such as mast cells, releasing chemical mediators such as histamine. Histamine triggers symptoms, including sneezing and a runny, itchy nose.1
Temporal classification of allergic rhinitis
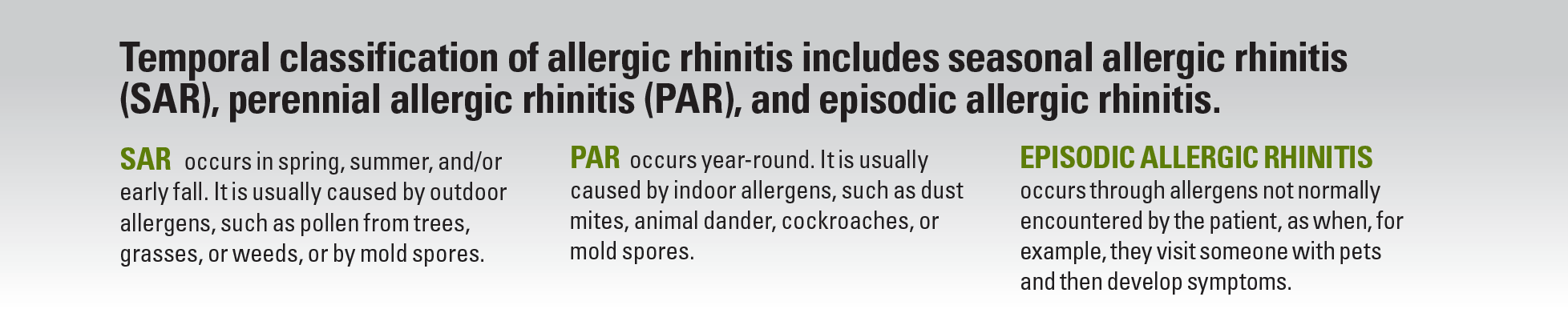
There are generally 3 pollen seasons, which vary based on the climate in which the patient lives. Spring is significant for tree pollen, including birch, cedar, cottonwood, and pine. However, in late spring, grasses, such as Timothy, Johnson, and rye, begin to pollinate. Toward the end of summer, ragweed pollen appears and continues into fall, along with outdoor molds. Environmental irritants, among them cigarette smoke, perfumes, diesel exhaust, and cleaning products, can also trigger nasal symptoms.8-13
Diagnosis
The diagnosis of allergic rhinitis is largely based on clinical history and physical exam. However, when patients do not improve with over-the-counter medication, the diagnosis is uncertain or the allergic trigger needs to be identified for targeted environmental mitigation, allergy testing is recommended. Specific IgE allergy testing, a blood sample or skin prick, helps aid in the diagnosis of allergies. A diagnostic algorithm for rhinitis is presented in Figure 1.1
Figure 1
The diagnosis of allergic rhinitis accounts for the timing, frequency or duration, and severity of symptoms. Classifying the disease is important to guide its management.
Allergic rhinitis classified by frequency and duration of symptoms is divided into intermittent and persistent. Intermittent allergic rhinitis has symptoms that last for fewer than 4 days per week or 4 weeks per year, whereas persistent allergic rhinitis symptoms last for more than 4 days per week and 4 weeks per year.1,7,14
Allergic rhinitis classified by severity of symptoms is divided into mild and moderate/severe. Mild allergic rhinitis does not interfere with the patient’s quality of life.1 However, moderate/severe allergic rhinitis has symptoms severe enough to decrease quality of life, such as disordered sleep, impaired daily activities, and missed school and work days.7 Results from recent studies suggest that poorly controlled allergic rhinitis can negatively affect academic performance.15
Further, it is important to note that approximately 30% to 50% of patients with chronic rhinitis may have a combination of allergic and nonallergic rhinitis, referred to as mixed rhinitis.5,16 Timely diagnosis and optimal management of allergic rhinitis is important to prevent complications, such as sinusitis, ear infections, chronic effusion, chronic headache, halitosis, dental problems, and sleep disturbances.1
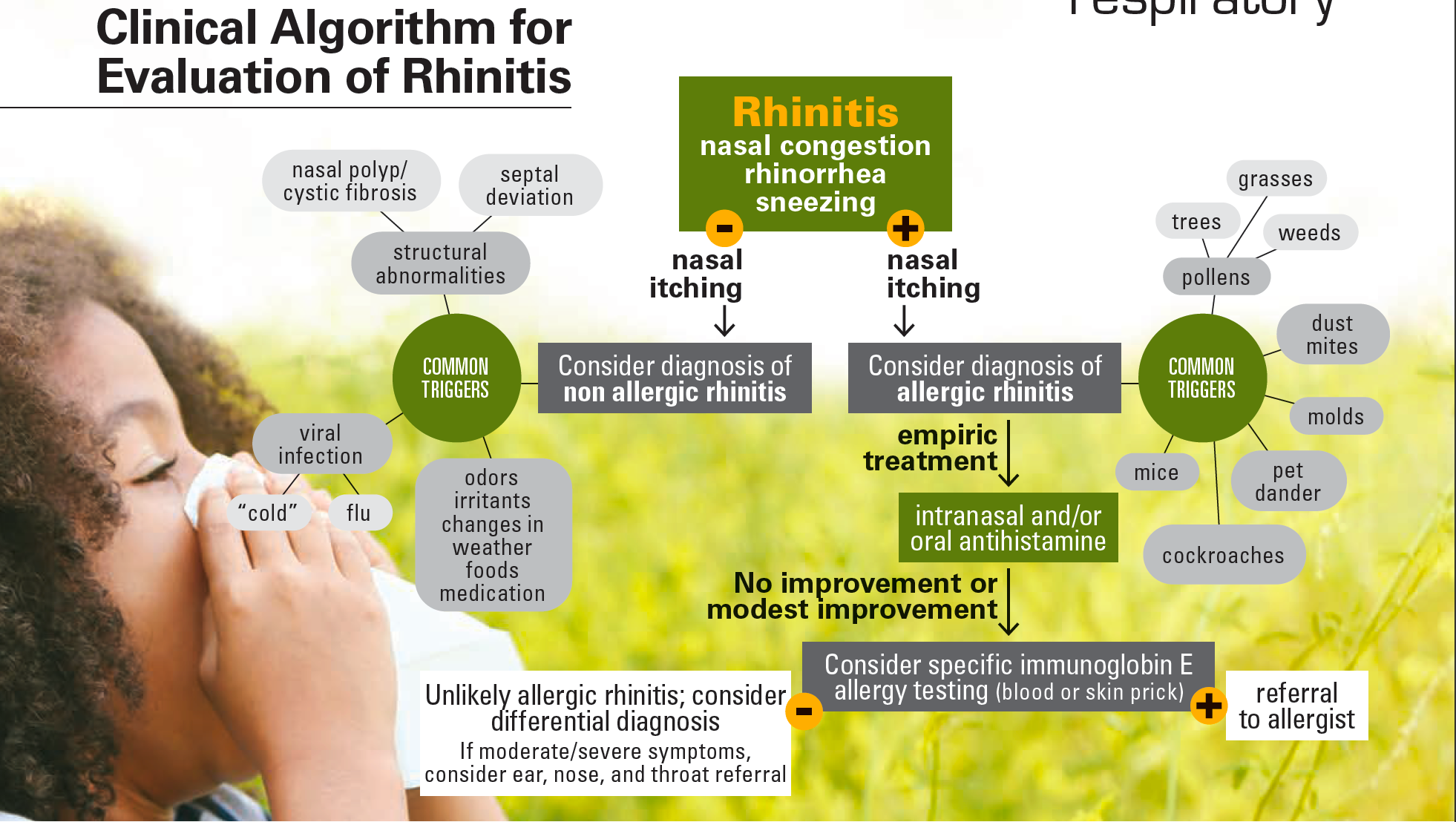
COVID-19 and environmental allergies
Sometimes it can be hard to tell the difference between allergies and viral illnesses, including coronavirus disease 2019 (COVID-19) infection. Many symptoms, such as nasal congestion, runny nose, cough, and headache, overlap, as illustrated in the National Center for Immunization and Respiratory Diseases’ Venn diagram (Figure 2).17 Therefore, it is crucial to keep COVID-19 infection high on the differential and to consider testing the patient.18
Figure 2
Management
PHARMACOLOGIC THERAPIES
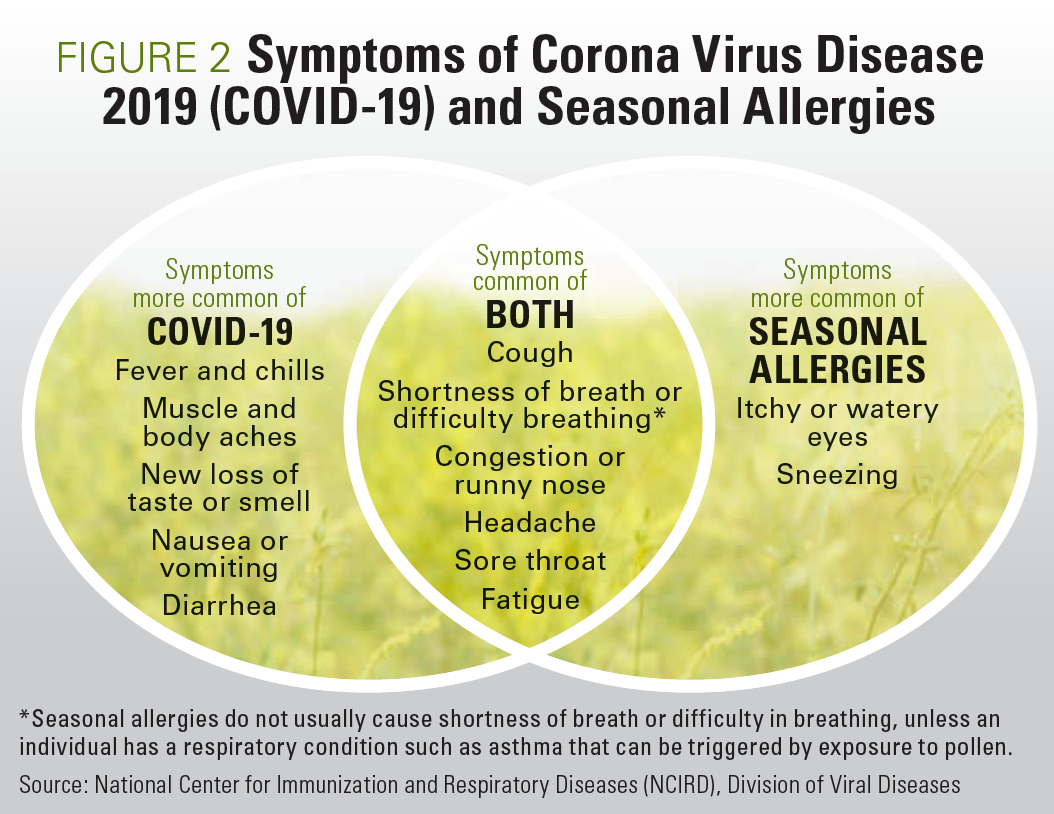
Managing allergic rhinitis and environmental allergies involves a 2-fold approach: pharmacologic therapies and environmental mitigation strategies. As exposure to allergens in sensitized individuals promotes inflammation, using medications to treat symptoms and mitigating exposure to allergens are very important. For treatment of seasonal allergy symptoms, initiating treatment with intranasal steroids and/or oral antihistamines is recommended 1 to 2 weeks prior to the start of the season; this should be continued throughout the season. The primary treatment for allergic rhinitis is intranasal steroids. However, they may not be tolerated in young children. Long-acting, nonsedating oral antihistamines (cetirizine, levocetirizine, fexofenadine, or loratadine) may be used in combination with or without intranasal steroids.1 An antihistamine or mast cell stabilizer eye drops, such as olopatadine or inhaled corticosteroids, are the mainstay of treatment for allergic asthma but therapy may need to be adjusted as outlined in the National Institutes of Health’s National Asthma Education and Prevention Program guidelines.2 Treatment of pollen food allergy syndrome entails avoiding the “fresh” form of culprit food(s) referenced in Figure 3, or other strategies such as peeling the skin or eating the cooked version. These strategies are typically tolerated.3
Figure 3
NATURAL REMEDIES AND COMPLEMENTARY AND ALTERNATIVE MEDICINE
Many patients inquire about the use of natural remedies in the treatment of allergic rhinitis and allergic conjunctivitis. Rinsing the nasal passages with over-the-counter saline in a squeeze bottle or a neti pot, for example, can be effective as a means of washing away the allergens and mucus to help reduce symptoms. Using humidifiers to treat nasal congestion is generally not recommended because it creates an environment which promotes the proliferation of dust mites and molds. Acupuncture has not been commonly used in the pediatric population, but findings from small studies suggest it may be beneficial in the treatment of allergic rhinitis.1 Natural remedies for the treatment of allergic conjunctivitis include applying a cold compress to the eyes or using refrigerated artificial tears to remove allergens.4
ENVIRONMENTAL MITIGATION STRATEGIES
The majority of individuals with allergy symptoms are allergic to more than one allergen. Exposure to allergens should be minimized because there is a symptom threshold and reducing exposure lowers the risk of symptom exacerbation. For example, a patient may be sensitized to dust mites, mold, and animal dander with minimal symptoms year-round; however, in spring, exposure to birch pollen may cause exacerbations because they have reached their symptom threshold due to cumulative exposure to allergens and tree pollen, and thus “tip them over the edge.”
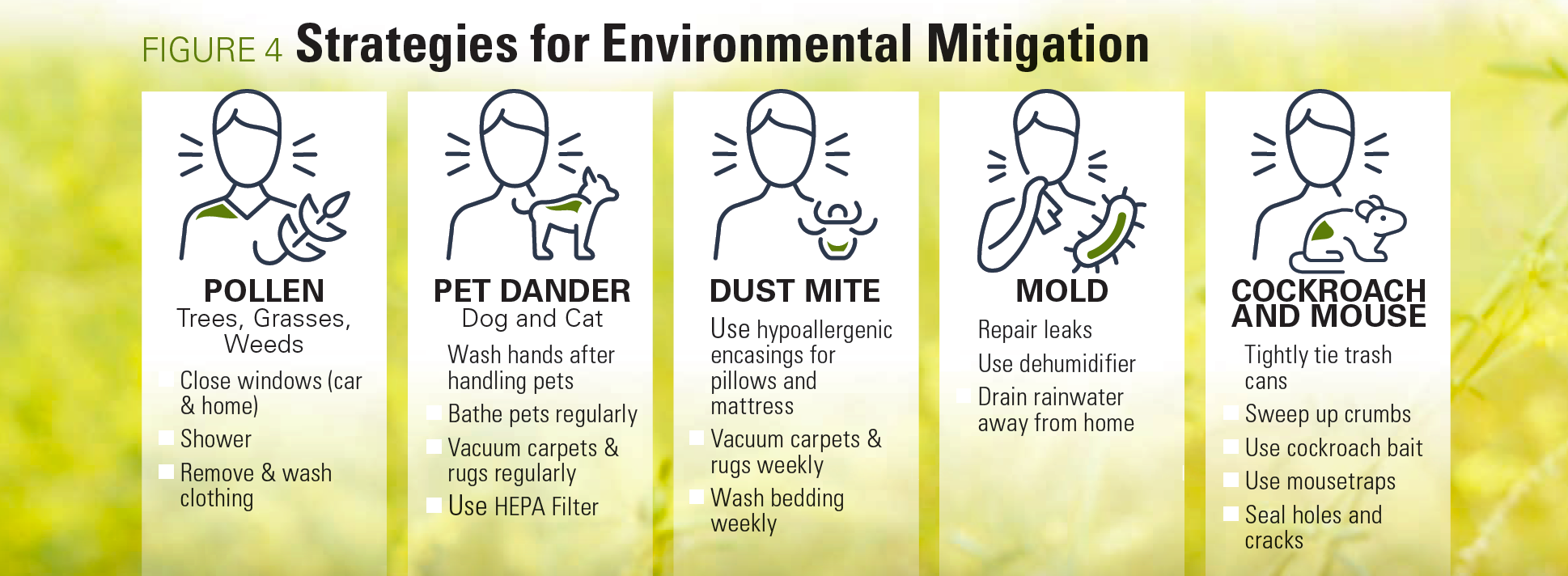
Pollens are microscopic and may be deposited on skin, hair, and clothing. Therefore, showering after coming in from outdoors is recommended. Trees tend to release the most pollen from 5 am to 9 am. Therefore, trying to minimize outdoor activities during the early morning hours may be helpful. Keeping windows closed in the car and home and wearing a mask with a small particle filter can also reduce pollen exposure. Figure 4 lists environmental mitigation strategies for common environmental allergens.1
Figure 4
IMMUNOTHERAPY
Subcutaneous and sublingual are 2 types of immunotherapy available for aeroallergens. Subcutaneous immunotherapy works by introducing small amounts of allergen(s) in escalating doses until a maintenance dose is reached that helps to desensitize allergy cells. Typically, the patient receives a maintenance dose monthly for 3 to 5 years under the supervision of a physician. In recent years, there have been few new allergy medications. In 2014, sublingual immunotherapy tablets were approved for grass (ages 5-65 years) and ragweed (ages 18-65 years) pollens. In 2017, a dust mite sublingual tablet was approved for use in adults.1 Sublingual tablets are not widely used in the pediatric population. One major barrier is the limited insurance coverage for these tablets. However, sublingual tablets may be used more frequently in the future as more children are formally diagnosed with common environmental allergens based on clinical history and confirmed with (blood sample or skin prick) allergy testing, and a more convenient home-based form of immunotherapy is desired.
When to refer patients to an allergist
If the patient does not improve with over-the-counter medications and there is evidence of sensitization to common environmental allergens on testing, consider referring to them to an allergist.1 Additionally, for patients who are atopic, a referral to an allergist to determine whether they are a candidate for allergen immunotherapy may be beneficial. Allergen immunotherapy is approved for the treatment of allergic rhinitis and asthma. For atopic patients with allergic rhinitis without preexisting asthma, subcutaneous allergen immunotherapy is indicated for the primary prevention of asthma.2
Conclusion
Spring allergies are common in the pediatric population. Recognizing signs or symptoms, classifying the disease and implementing a 2-fold management approach is key to quality of life for patients. Although pediatricians manage most cases of allergic rhinitis in children, knowing when to refer to an allergist is important.
References
- Seidman MD, Gurgel RK, Lin SY, et al. Clinical practice guideline: allergic rhinitis executive summary. Otolaryngol Head Neck Surg. 2015;152(20:197-206. doi:10.1177/0194599814562166
- Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI) administered and coordinated National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC); Cloutier MM, Baptist AP, Blake KV, et al. 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 2020;146(6):1217-1270. doi:10.1016/j.jaci.2020.10.003
- Poncet P, Sénéchal H, Charpin D. Update on pollen-food allergy syndrome. Expert Rev Clin Immunol. 2020;16(6):561-578. doi:10.1080/1744666X.2020.1774366
- Bielory L, Delgado L, Katelaris CH, Leonardi A, Rosario N, Vichyanoud P. ICON: diagnosis and management of allergic conjunctivitis. Ann Allergy Asthma Immunol. 2020;124(2):118-134. doi:10.1016/j.anai.2019.11.014
- Dykewicz MS, Wallace DV, Amrol DJ, et al. Rhinitis 2020: a practice parameter update. J Allergy Clin Immunol. 2020;146(4):721-767. doi:10.1016/j.jaci.2020.07.007
- Summary health statistics: national health interview survey, 2014. Centers for Disease Control and Prevention. Accessed January 16, 2021. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2014_SHS_Table_C-2.pdf
- Dykewicz MS, Wallace DV, Baroody F, et al. Treatment of seasonal allergic rhinitis: an evidence-based focused 2017 guideline update. Ann Allergy Asthma Immunol. 2017;119(6):489-511.e41. doi:10.1016/j.anai.2017.08.012
- Allergic rhinitis. American College of Allergy, Asthma and Immunology. Updated June 17, 2020. Accessed January 16, 2021. https://acaai.org/allergies/types/hay-fever-rhinitis
- Allergy facts. American College of Allergy, Asthma and Immunology. Updated January 9, 2018. Accessed January 16, 2021.https://acaai.org/news/facts-statistics/allergies
- Hay fever. Mayo Clinic. July 16, 2020. Accessed January 16, 2021. https://www.mayoclinic.org/diseases-conditions/hay-fever/symptoms-causes/syc-20373039
- Pollen allergy. Asthma and Allergy Foundation of America. Updated October 2015. Accessed January 16, 2021. https://www.aafa.org/pollen-allergy/
- Rhinitis (hay fever) overview. American Academy of Allergy, Asthma and Immunology. Accessed January 16, 2021. https://www.aaaai.org/conditions-and-treatments/allergies/rhinitis
- Rhinitis (nasal allergies). Asthma and Allergy Foundation of America. Updated October 2015. Accessed January 16, 2021. https://www.aafa.org/rhinitis-nasal-allergy-hayfever/
- Gentile D, Bartholow A, Valovirta E, Scadding G, Skoner D. Current and future directions in pediatric allergic rhinitis. J Allergy Clin Immunol Pract. 2013;1(3):214-226. doi:10.1016/j.jaip.2013.03.012
- Blaiss MS, Hammerby E, Robinson S, Kennedy-Martin T, Buchs S. The burden of allergic rhinitis and allergic rhinoconjunctivitis on adolescents: a literature review. Ann Allergy Asthma Immunol. 2018;121(1):43-52.e3. doi:10.1016/j.anai.2018.03.028
- Greiwe JC, Bernstein JA. Allergic and mixed rhinitis: diagnosis and natural evolution. J Clin Med. 2019;8(11):2019. doi:10.3390/jcm8112019
- Infographic: Venn diagram of the overlap of COVID-19 symptoms with seasonal allergy symptoms. Centers for Disease Control and Prevention. Updated September 10, 2020. Accessed January 16, 2021.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/infographic-overlap-symptoms.html#text
- Brough HA, Kalayci O, Sediva A, et al. Managing childhood allergies and immunodeficiencies during respiratory virus epidemics – the 2020 COVID‐19 pandemic: a statement from the EAACI‐section on pediatrics. Pediatr Allergy Immunol. 2020; 31(5):442-448. doi:10.1111/pai.13262
The Role of the Healthcare Provider Community in Increasing Public Awareness of RSV in All Infants
April 2nd 2022Scott Kober sits down with Dr. Joseph Domachowske, Professor of Pediatrics, Professor of Microbiology and Immunology, and Director of the Global Maternal-Child and Pediatric Health Program at the SUNY Upstate Medical University.