Sports-related concussion: When it's OK to return to play
Pediatricians need to understand both pathophysiology and management of concussion to correctly address the question of return-to-play for athletes after a jolt to the head.
Table 1

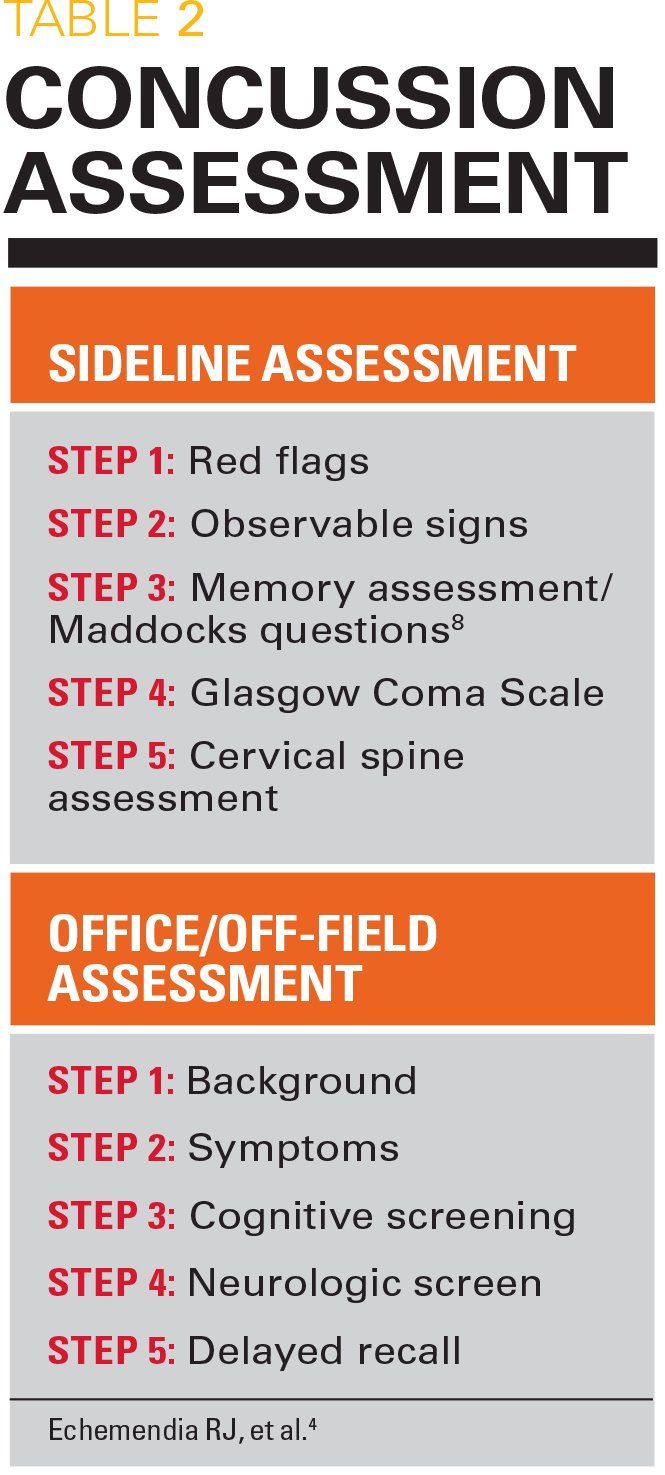
Table 2
Resources for Pediatricians
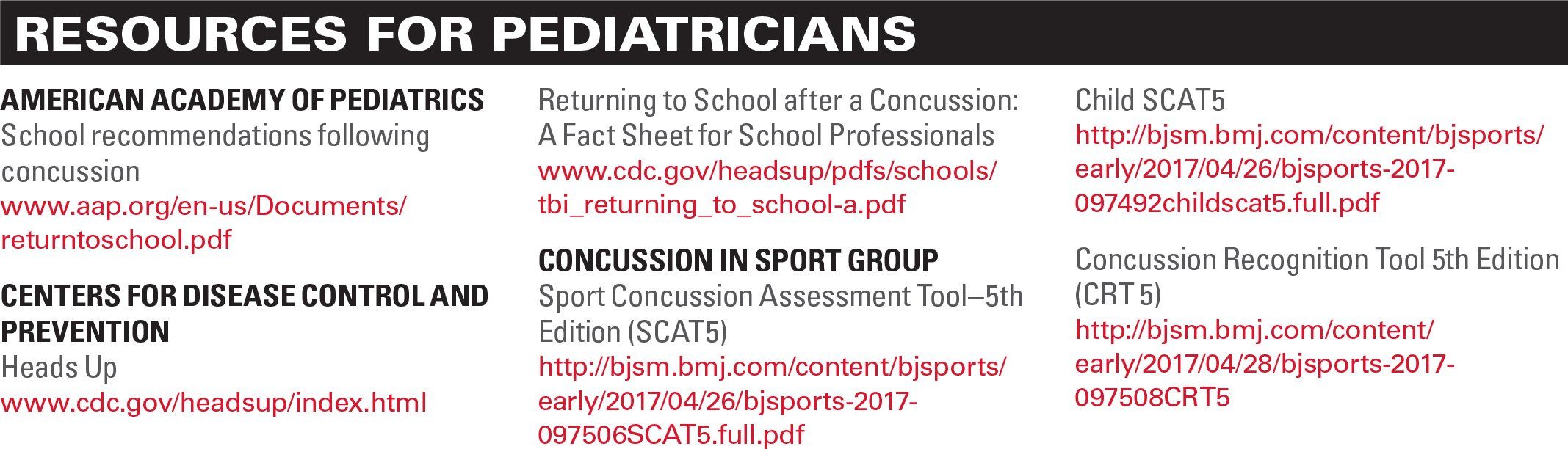
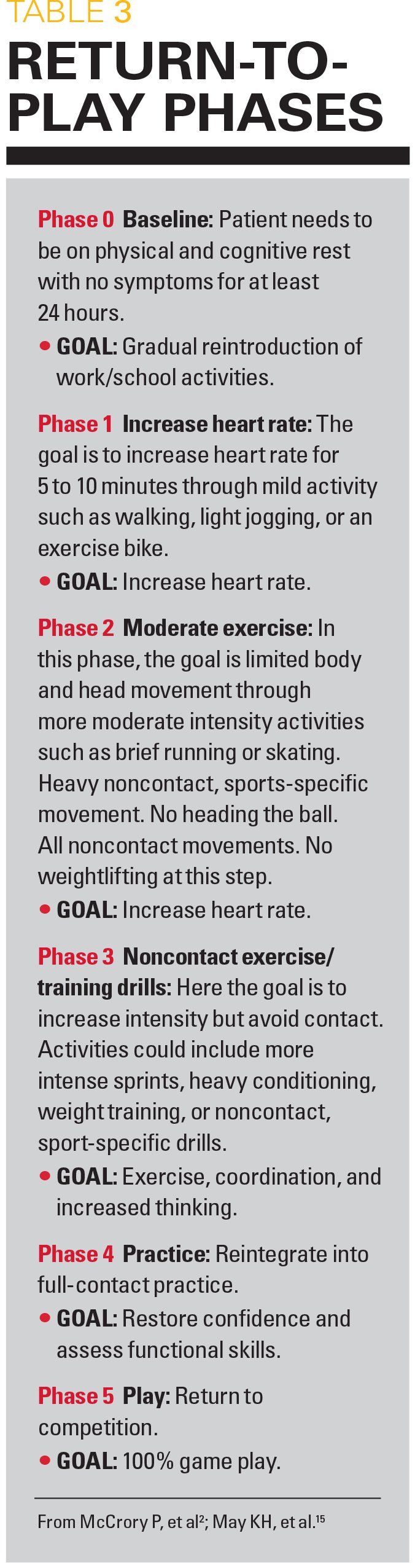
Table 3
Concussions are a common problem for the pediatrician with 1.6 to 3.8 million occurring per year in the United States.1 Although falls, motor vehicle accidents, and assaults are the most common etiology, 1 in 5 is a sports-related concussion (SRC). The percentage of SRC is even higher in adolescents. The pediatrician needs to be able to discuss this topic with parents and caregivers, identify common symptoms, and know when a child can return to play when an SRC is suspected.
Concussion is synonymous with mild traumatic brain injury (MTBI) and can be defined as: “a complex pathophysiologic process affecting the brain, induced by traumatic biomechanical forces secondary to direct or indirect forces to the head. MTBI is caused by a blow or jolt to the head that disrupts the function of the brain. This disturbance of brain function is typically associated with normal structural neuroimaging findings (ie, computed tomography [CT] scan, magnetic resonance imaging [MRI]).”1
A number of different features may be used in further defining the nature of an SRC:2
· May be caused by a direct blow to the head or elsewhere (eg, neck or face) with forces transmitted to the head.
· Has typically rapid onset of and short duration of neurologic impairment with spontaneous resolution of symptoms. However, in some cases, signs and symptoms may evolve over a longer period (minutes to hours).
· May result in neuropathologic changes, but the acute injury reflects a functional disturbance as opposed to a structural injury.
· Range of clinical signs and symptoms may not involve a loss of consciousness. Resolution of symptoms typically follows a sequential course, but prolonged symptoms occur in some.
· Only 10% of concussions involve a loss of consciousness.
Pathophysiology and symptoms
The disturbance in brain function from a concussion is more related to brain metabolism than to a structural injury or damage. Neuronal dysfunction involves a number of different processes and a complex cascade of metabolic and physiologic events3 that may result in a constellation of symptoms (Table 1).
Diagnosis and assessment
Scenario 1:A 15-year-old lacrosse player comes off the field after a helmet-to-helmet contact complaining of headache, ringing in his ears, dizziness, and nausea. What should be done next?
Although an SRC can be difficult to diagnose in real time, the adolescent clearly had a helmet-to-helmet contact and now has symptoms. Further, the majority of SRCs do not involve a loss of consciousness. In any suspected case of concussion, the athlete should be removed from the activity and assessed by a physician or other licensed healthcare provider.2
Diagnosing suspected SRC involves the assessment of clinical symptoms, physical signs, cognitive impairment, neurobehavioral symptoms, and sleep/wake disturbances (Table 1). An SRC diagnosis should be suspected when there are abnormalities in 1 or more of these domains.2
Sideline assessment
Sideline assessments consisting of neuropsychologic test batteries and memory function are both effective and practical. The Sport Concussion Assessment Tool–5th Edition (SCAT5)4 is one such test and is the most well-established and rigorously tested assessment for SRC. The SCAT5 should be administered by an appropriately trained health professional, whereas coaches and other nonlicensed personnel should use the Concussion Recognition Tool 5th Edition (CRT5).5 There is no evidenced-based recommendation for any particular tool or protocol and best practice dictates a tool such as the SCAT with possible addition of video review if available.6
However, the SCAT5 should not continue to be used as an assessment tool when more than 3 to 5 days have lapsed since the injury.2 The SCAT5 can be used in children aged older than 12 years and adults. There is also a version for children aged younger than 12 years.7
The SCAT5 employs an on-field rapid assessment for suspected SRC. It is important for the pediatrician to understand that the tool does not provide definitive diagnosis of a head injury. The immediate sideline assessment consists of 5 steps (Table 2):4
STEP 1: RED FLAGS
In Step 1, the pediatrician or health professional is looking for red flag signs that should lead to immediate removal and evaluation. The symptoms include:4
· Neck pain (consider cervical-spine injury)
· Double vision
· Numbness or weakness in an extremity (consider cervical-spine or spinal-cord injury)
· Severe or worsening headache (consider intracranial bleed)
· Seizure
· Loss of consciousness or deteriorating level of consciousness (consider intracranial bleed)
· Vomiting (consider increased intracranial pressure)
· Restless, agitated, or combative (consider increased intracranial pressure or bleeding)
STEP 2: OBSERVABLE SIGNS
In Step 2, the pediatrician is looking for observable signs of an SRC, such as:4
· Lying motionless on the playing surface
· Balance and gait abnormalities
· Disorientation or confusion
· Blank or vacant look
· Facial injury after head trauma
STEP 3: MEMORY ASSESSMENT/MADDOCKS QUESTIONS8
The SCAT5 uses 5 brief questions to assess the athlete’s memory. It is important for the pediatrician to know that standard orientation questions such as time, place, and person are unreliable in athletic competition.4
STEP 4: GLASGOW COMA SCALE (GCS)
The GCS is a well-known, researched, and practical assessment tool for impairment of conscious level in response to predetermined stimuli.
STEP 5: CERVICAL SPINE ASSESSMENT
In the final step the pediatrician asks the athlete if he or she is pain free at rest. If there is no pain at rest, the pediatrician then asks if the athlete remains pain free with full active range of motion and determines if limb and sensation are normal.
Office/off-field assessment
If the sideline assessment determines that SRC is no longer suspected, the physician or health professional can determine when it is appropriate for the athlete to return to play. If it is determined that additional testing is needed, it should be done in a distraction-free environment such as a medical or locker room.2 The office/off-field assessment should be performed when the patient is in a resting state at approximately the patient’s resting heart rate. It includes 5 steps (Table 2):4
STEP 1: BACKGROUND
In Step 1, the pediatrician takes a history focusing on prior concussions or head injuries, prior treatment for concussions, and previous recovery time. It is also important to establish whether the patient has a prior history of headaches, learning disabilities, depression, anxiety, or mental health comorbidities, as well as any current medication.
STEP 2: SYMPTOMS
The athlete is given a symptom form, reads it aloud, and completes a severity scale for the 22 listed symptoms such as headache, sensitivity to noise or light, and difficulty remembering.
STEP 3: COGNITIVE SCREENING
The athlete completes tasks related to orientation and immediate memory. The tool also assesses concentration by having the athlete repeat a series of numbers read backward to him or her and naming the months of the year in reverse order.
STEP 4: NEUROLOGIC SCREEN
The patient’s reading of the symptoms (step 2), cervical pain, double vision, finger-to-nose test, and tandem gait are all assessed as part of the SCAT5. A complete neurologic exam is also recommended, including cranial nerves, sensation, reflexes, cerebellar testing, finger-to-nose, rapid alternating hands, heel-to-shin, and Romberg test. The athlete is also asked to perform a number of balance tests such as standing on 1 leg and tandem gait. Balance is often off in the acute setting.
STEP 5: DELAYED RECALL
The patient is asked to repeat as many words from the immediate recall task at least 5 minutes later.
The athlete’s SCAT5 score is:
· Immediate recall-12/15
· Concentration-2/5
· Modified Balance Error Scoring System (m-BESS)-22/30
Return-to-play
Scenario 2:After 20 minutes, the athlete says he feels fine and wants to return to the game. The exam is now normal and concentration and delayed recall have improved. Can he return to play?
Creighton and colleagues9 developed a 3-step decision-based model that can assist the pediatrician in a return-to-play decision. It focuses on:
· Health status of the athlete. In this step, the pediatrician looks at medical factors related to how much healing has occurred, what current symptoms are, and potential seriousness of injury.
· Participation risk. In this step, the pediatrician looks at not only the current health status of the athlete, but also what risks are inherent to a particular sport, position of the particular athlete in question, and ability to protect. Different individuals may have different levels of acceptable risk
· Decision modifiers. Finally, there are other things that may influence a decision such as pressure from the athlete or family, timing of the season, external pressures, or fear of litigation.9
This athlete should not return to play despite not having symptoms. No patient should return to play on the same day as an SRC. All 50 states have Return-to-Play laws so the pediatrician should be familiar with the laws in his or her own state.
The 5th International Conference on Concussion’s 2016 Consensus Statement on Concussion in Sport states: “A player with diagnosed SRC should not be allowed to return to play on the day of injury.”2 The statement says further that athletes should rest until they become symptom free and can be encouraged to gradually increase cognitive and activity levels while keeping both to a level that does not increase symptoms. Unfortunately, the exact amount of and duration of rest is not known.
The significant concern for immediate return is second-impact syndrome-rapid cerebral vascular congestion due to flow dysregulation following a concussion that can lead to cerebral swelling and death.10 Typically second-impact syndrome occurs in the first 1 to 2 weeks after an initial concussion and this fact should be taken into account when giving guidelines for a return-to-play protocol. Often the protocol is spread out in children (no data on this) but it is suggested to allow phases to take 7 to 14 days depending on the child to fully return to contact.
Analysis from a US national registry over 30 years revealed approximately 9 deaths per year, most commonly in football, after a recent history of concussion.11 In a 2016 report in Pediatric Neurology that identified 17 patients in the published literature with second-impact syndrome in American football, male gender and young age appeared to be associated risk factors.10
Return-to-learn
Scenario 3:The lacrosse player is removed from the game and remains symptomatic. His parents are given education about red flags and he is told to follow up with his pediatrician. Two days after his lacrosse match, he is reporting daily headaches, dizziness, fatigue, and noise sensitivity. He is a good student and has several tests this week. What is the next step?
The pediatrician in the office should perform or repeat the SCAT5 to see any worsening or improvement in symptoms. Of note, many institutions and schools now require a preseason assessment so that objective changes are readily apparent when a pediatrician or health professional has no prior experience with an athlete.
Patients experiencing a concussion should avoid reinjury and avoid overexertion-both physical and mental. This may require some school accommodations. The athlete should not return to play until he or she has first successfully returned to school.2
Although lacking research demonstrating harm, cognitive rest (avoiding cognitive stressors such as video games, school work, texting, and TV) has been recommended by several clinical guideline statements.12 A number of studies have, in fact, demonstrated that intense cognitive activity may actually worsen concussive symptoms.13,14 Intense cognitive and intellectually demanding activities possibly stress an already metabolically altered brain and result in worsening symptoms.
Whereas returning to a normal routine is good for an adolescent, one of the main goals in management of the post-concussive patient is to limit cognitive activity to the point where it begins to reproduce or worsen symptoms.
One recommendation is that athletes should remain out of school as long as symptoms prevent concentration for up to 30 minutes. After the student athlete is able to tolerate 30 minutes of cognitive activity without a worsening of symptoms, the student may begin home tutoring or in-school instruction.12 The 2016 guideline recommends 24 to 48 hours of rest followed by gradual and more progressive increases in cognitive activity, being careful to not exacerbate symptoms.2
Most students will return to school while experiencing symptoms from their concussion. Certain “academic adjustments” may need to be made to the adolescent’s regular schedule and may need to be negotiated among school, parent, and the pediatrician.
These adjustments (see Resources for Pediatricians for a form the pediatrician can use to communicate with schools) need to be individualized to student and school but could include:12
· Shortened days
· 30 minutes of instruction with a 15-minute break
· Providing class notes
· Tutoring
· Decreasing course expectations
· Decreasing exposure to classes that exacerbate symptoms
· No computer work
· Untimed tests and quizzes
· Lunch in a quiet place
The 2016 concussion guidelines recommend a 4-stage approach for return-to-learn:2
· Stage 1. Typical daily activities at home that do not increase symptoms. Start with 5 to 10 minutes and gradually build up.
· Stage 2. School activities such as homework, reading assignments, and other cognitive activities outside of regular school.
· Stage 3. Return to school part time, partial days, or with extended breaks during the day.
· Stage 4. Return to school full time with normal educational activities until a full day can be achieved without symptoms.
Most students will recover within 4 weeks and the academic adjustments can be discontinued.2 “Academic accommodation” or “academic modification” may be required if longer-term assistance is needed. These official plans, often referred to as a 504 plan, may require input from the pediatrician and include accommodations such as extra time for work and tests. In academic modification, changes usually are longer and may involve altering grade-level educational plans through an individualized educational program (IEP). These IEPs are comprehensive plans developed among parents, teachers, and school staff to address unique educational needs of students and address any accommodations.
Guidelines for return-to-play
The American Academy of Pediatrics and the 2016 concussion guideline recommend a 6-step process allowing for gradual return-to-play (Table 3).2,15 The protocol progresses every 24 hours so long as symptoms do not occur. If any symptoms of concussion occur, the patient is returned to the previous phase.
Symptoms should be monitored at each phase and athletes should not progress if they begin to experience symptoms. Symptoms indicate the need for additional rest. When the athlete is not experiencing symptoms for a minimum of 24 hours, he or she may begin at the previous step where he/she experienced symptoms. Individual athletes will progress through the phases differently and it may take several weeks to complete all 6 phases. Younger athletes typically will take longer than older adolescents.
When to refer
If symptoms are persistent for more than 1 month in children, the athlete should be referred to a healthcare professional who is an expert in the management of concussion.
At this time when school-aged athletes are returning for fall sports programs, the pediatrician’s understanding of both the pathophysiology and management of concussion will help him or her to correctly address this common pediatric problem when these youngsters ask, “When can I play?”
References:
1. Centers for Disease Control and Prevention. Heads Up: Facts for Physicians About Mild Traumatic Brain Injury (MTBI). Available at: http://www.concussiontreatment.com/images/CDC_Facts_for_Physicians_booklet.pdf. Accessed July 2, 2018.
2. McCrory P, Meeuwisse W, Dvorák J, et al. Consensus statement on concussion in sport-the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847.
3. Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228-235.
4. Echemendia RJ, Meeuwisse W, McCrory P, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): background and rationale. Br J Sports Med. 2017;51(11):848-850.
5. Echemendia RJ, Meeuwisse W, McCrory P, et al. The Concussion Recognition Tool 5th Edition (CRT5): background and rationale. Br J Sports Med. 2017;51(11):870-871.
6. Patricios J, Fuller GW, Ellenbogen R, et al. What are the critical elements of sideline screening that can be used to establish the diagnosis of concussion? A systematic review. Br J Sports Med. 2017;51(11):888-894.
7. Davis GA, Purcell L, Schneider KJ, et al. The Child Sport Concussion Assessment Tool 5th Edition (Child SCAT5): background and rationale. Br J Sports Med. 2017;51(11):859-861.
8. Maddocks DL, Dicker GD, Saling MM. The assessment of orientation following concussion in athletes. Clin J Sport Med. 1995;5(1):32-35.
9. Creighton DW, Shrier I, Shultz R, Meeuwisse WH, Matheson GO. Return-to-play in sport: a decision-based model. Clin J Sport Med. 2010;20(5):379-385.
10. McLendon LA, Kralik SF, Grayson PA, Golomb MR. The controversial second impact syndrome: a review of the literature. Pediatr Neurol. 2016;62:9-17.
11. Thomas M, Haas TS, Doerer JJ, et al. Epidemiology of sudden death in young, competitive athletes due to blunt trauma. Pediatrics. 2011;128(1):e1-e8.
12. Halstead ME, McAvoy K, Devore CD, et al; Council on Sports Medicine and Fitness; Council on School Health. Returning to learning following a concussion. Pediatrics. 2013;132(5):948-957.
13. Howell D, Osternig L, Van Donkelaar P, Mayr U, Chou LS. Effects of concussion on attention and executive function in adolescents. Med Sci Sports Exerc. 2013;45(6):1030-1037.
14. Sady MD, Vaughan CG, Gioia GA. School and the concussed youth: recommendations for concussion education and management. Phys Med Rehabil Clin N Am. 2011;22(4):701-719.
15. May KH, Marshall DL, Burns TG, Popoli DM, Polikandriotis JA. Pediatric sports specific return to play guidelines following concussion. Int J Sports Phys Ther. 2014;9(2):242-255.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.