Internal Jugular Phlebectasia
A 16-year-old girl with internal jugular phlebectasia presented for followup ultrasound evaluation. At age 15 months, she was noted to have a right-sided neck mass that appeared when crying or straining. Her weight, height, and head circumference were normal. She had no cardiac anomalies and was otherwise healthy.

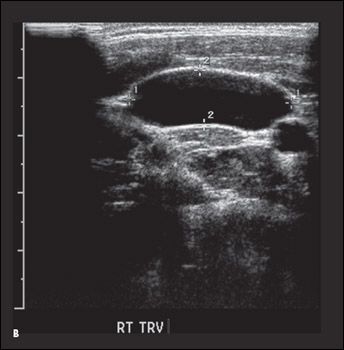
A 16-year-old girl with internal jugular phlebectasia presented for followup ultrasound evaluation. At age 15 months, she was noted to have a right-sided neck mass that appeared when crying or straining. Her weight, height, and head circumference were normal. She had no cardiac anomalies and was otherwise healthy. An ultrasonogram performed at 18 months of age showed a fusiform dilation of the right internal jugular vein; it measured 0.71 to 0.79 cm along the mid-portion when the infant was at rest and 2.98 cm when she was crying. The dilation extended from the mandible down to the clavicle. An ultrasound evaluation at 22 months showed no interval change. At 16 years' follow-up, the dilation had an average diameter of 1.88 cm at rest (A and B) and a 3.95-cm diameter during a Valsalva maneuver (C and D).
Internal jugular phlebectasia is associated with few complications; those that are seen include Horner syndrome,1 thrombosis,2 heart failure,3 and slight dysphagia.4 Thus, most studies recommend observation.5-8 Surgical intervention is generally reserved for cosmetic and psychological purposes.9,10 However, the fear of rupture or thrombosis has led some to recommend surgery universally.9 Postoperative complications are rare but may include intracranial hypertension and thrombosis of the right internal jugular vein with infarction of the right pontine9 and injury to vital neck structures, especially with jugular phlebectasia resection.

Tracking the natural history of internal jugular phlebectasia can help answer the question of whether medical intervention is necessary or would benefit the patient. Reports of conservative management describe cases with 6-month follow-up5; 1-year follow-up with no progressive dilation6; 24-month follow-up with reduced dilation7; 3-year follow-up8; and 8.5-year follow-up.11 In a review of 45 children with jugular vein phlebectasia, all but 5 ultimately underwent surgery; the remaining 5 children were observed for 2 to 15 years.9
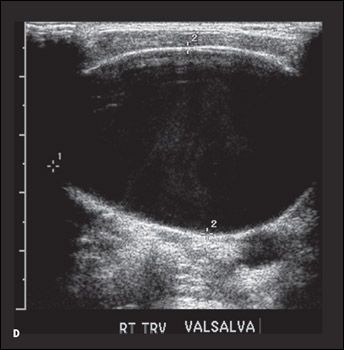
In this patient, serial ultrasonography easily confirmed the clinical diagnosis and provided an excellent modality for follow-up. Despite the progressive dilation noted concomitantly with the patient's growth, she has continued to develop normally, has required no activity restrictions, and has remained asymptomatic.
References:
REFERENCES:
1.
Inci S, Bertan V, Kansu T, Cila A. Horner's syndrome due to a jugular venous ectasia.
Childs Nerv Syst
. 1995;11:533-535.
2.
Zohar Y, Ben-Tovim R, Talmi YP. Phlebectasia of the jugular system.
J Craniomaxillofac Surg
. 1989;17:96-98.
3.
Spiro SA, Coccaro SF, Bogucki E. Aneurysm of the internal jugular vein manifesting after prolonged positive pressure ventilation.
Head Neck
. 1991;13:450-452.
4.
Bosshardt TL, Honig MP. Congenital internal jugular venous aneurysm: diagnosis and treatment.
Mil Med
. 1996;161:246-247.
5.
Chao HC, Wong KS, Lin SJ, et al. Ultrasonographic diagnosis and color flow Doppler sonography of internal jugular venous ectasia in children.
J Ultrasound Med
. 1999;18:411-416.
6.
Erdem CZ, Erdem LO, Camuzcuoglu I. Internal jugular phlebectasia: usefulness of color Doppler ultrasonography in the diagnosis.
J Trop Pediatr
. 2002;48:306-310.
7.
Indudharan R, Quah BS, Shuaib IL. Internal jugular phlebectasia-an unusual cause of neck swelling.
Ann Trop Paediatr
. 1999;19:105-108.
8.
Mickelson SA, Spickler E, Roberts K. Management of internal jugular vein phlebectasia.
Otolaryngol Head Neck Surg
. 1995;112:473-475.
9.
Jianhong L, Xuewu J, Tingze H. Surgical treatment of jugular vein phlebectasia in children.
Am J Surg
. 2006;192:286-290.
10.
Sander S, Eliçevik M, Unal M, Vural O. Jugular phlebectasia in children: is it rare or ignored?
J Pediatr Surg
. 1999;34:1829-1832.
11.
Paleri V, Gopalakrishnan S. Jugular phlebectasia: theory of pathogenesis and review of literature.
Int J Pediatr Otorhinolaryngol
. 2001;57:155-159.