Osteoid Osteoma in an Obese 17-Year-Old Boy
During a well adolescent visit, an obese 17-year-old boy complained of left knee pain of 4 years’ duration. The pain was worse at night. He was able to ambulate. He associated the pain with a left tibial fracture he sustained after falling off a bicycle 4 years earlier; he denied recent trauma.

During a well adolescent visit, an obese 17-year-old boy complained of left knee pain of 4 years' duration. The pain was worse at night. He was able to ambulate. He associated the pain with a left tibial fracture he sustained after falling off a bicycle 4 years earlier; he denied recent trauma.
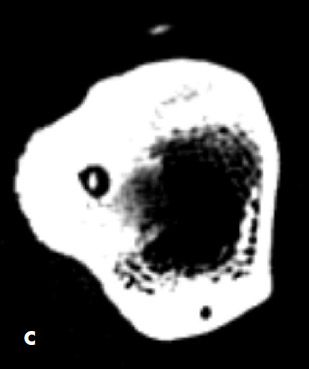
A nontender bony mass was noted over the left anterior tibia. The patient was referred to an orthopedist. Radiographs of the left knee revealed a sclerotic lesion in the proximal diaphysis of the left tibia, with a suggestion of central lucency (A). A second radiograph was read as compatible with chronic osteomyelitis with sequestrum formation. Further evaluation with a CT scan revealed a 5-cm sclerotic lesion in the tibial diaphysis with a lucent nidus with speckled calcification at its center and overlying soft tissue swelling (B and C). There was no periosteal reaction or fracture.
A complete blood cell count, erythrocyte sedimentation rate, and C-reactive protein level were normal. A trial of ibuprofen provided partial relief.
The clinical features, radiographic findings, and pain relief with NSAIDs are characteristic of osteoid osteoma. This solitary lesion is the third most common benign bone tumor. It is usually seen in the second and third decades of life, with a male preponderance. More than 50% of cases occur in the diaphysis or metaphysis of lower extremity long bones and present with longstanding pain that is worse at night.1 Spinal osteoid osteomas occur almost exclusively in the posterior vertebral elements and cause painful scoliosis from paravertebral spasm.2 Intra-articular osteoid osteomas occur in a juxta-articular bone within a synovial bone and present with pain, decreased range of motion, joint effusion, and soft tissue swelling.1

Radiographs show an area of cortical thickening and sclerosis. A lucent nidus is seen in 85% of cases.3 Other imaging modalities (eg, technetium-99m scan) are helpful when the lesion is not clearly demonstrated on plain radiographs.1 CT scans can help identify the nidus within the radiologically dense reactive zone around it and help differentiate it from chronic osteomyelitis. MRI findings show marrow and soft tissue edema, which can be confused with malignant tumors or osteomyelitis.4
Although prostaglandin E2 seems to play a role in the pain mechanism, the pathogenesis of osteoid osteoma is controversial. Some believe that the lesions are neoplasms, whereas others think they represent an unusual healing and reparative process, with no evidence of fracture, infection, or infarction.
Spontaneous regression over a period of years is likely. The nidus calcifies, ossifies, and ultimately blends in with the surrounding bone, with a gradual diminishing of pain. Thus, conservative treatment with NSAIDs and watchful waiting is often the first-line management and is especially useful in children with lesions that warrant removal but are difficult to access surgically.
The need for surgical resection depends on symptom severity and the extent of interference with activities of daily living. The nidus can be removed by either en bloc resection or the burr-down technique. Minimally invasive techniques, such as percutaneous nidus removal via CT-guided core-drill excision5 and destruction of the nidus via thermoregulation,6 radiofrequency,7 and laser8 are alternatives.
Secondary osteoarthritic changes (limping, leg length discrepancies, muscle atrophy, and structural deformities) may be seen with intra-articular lesions if treatment is delayed.
References:
REFERENCE:
1.
Lee EH, Shafi M, Hui JH. Osteoid osteoma: a current review.
J Pediatr Orthop
. 2006;26:695-700.
2.
Pettine KA, Klassen RA. Osteoid-osteoma and osteoblastoma of the spine.
J Bone Joint Surg Am
. 1986;68:354-361.
3.
Yildiz Y, Bayrakci K, Altay M, Saglik Y. Osteoid osteoma: the results of surgical treatment.
Int Orthop
. 2001;25:119-122.
4.
Moser T, Giacomelli MC, Clavert JM, et al. Image-guided laser ablation of osteoid osteoma in pediatric patients.
J Pediatr Orthop
. 2008;28:265-270.
5.
Assoun J, Railhac JJ, Bonnevialle P, et al. Osteoid osteoma: percutaneous resection with CT guidance.
Radiology
. 1993;188:541-547.
6.
de Berg JC, Pattynama PM, Obermann WR, et al. Percutaneous computedtomography- guided thermocoagulation for osteoid osteomas.
Lancet
. 1995;346: 350-351.
7.
Rosenthal DI, Hornicek FJ, Wolfe MW, et al. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment.
J Bone Joint Surg Am
. 1998;80:815-821.
8.
Gangi A, Dietemann JL, Guth S, et al. Percutaneous laser photocoagulation of spinal osteoid osteomas under CT guidance.
AJNR
. 1998;19:1955-1958
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.