Pediatric Musculoskeletal Infections: Advances in Diagnosis and Management
Musculoskeletal infections in children encompass a broad spectrum of entities that vary greatly in severity and complexity. Their presentation ranges from obvious and acute to insidious and chronic.
Musculoskeletal infections in children encompass a broad spectrum of entities that vary greatly in severity and complexity. Their presentation ranges from obvious and acute to insidious and chronic.
Musculoskeletal infections include osteomyelitis (an infection of any bone), septic arthritis (a joint infection), and pyomyositis. These infections are somewhat common in children. The peak incidence of bone infections occurs between ages 5 and 10 years; joint infections occur most frequently during the first 5 years of life. The majority of infections occur as a result of hematogenous inoculation, although penetrating trauma or surgical procedures can initiate the process. Timely workup is essential to ensure accurate diagnosis and prompt treatment for improved clinical outcomes.
This 2-part article reviews management approaches to pediatric musculoskeletal infections. In this first part, we describe principles of patient evaluation, classification of osteomyelitis and corresponding approaches to management, and special forms of osteomyelitis. The second part, to appear in a later issue of this journal, will focus on significant causative organisms to watch out for.
EVALUATING PATIENTS
History and examination. A thorough history and clinical examination remain paramount in the evaluation of infants, children, and young adults who may have a musculoskeletal infection. Most of these infections are bacterial; Staphylococcus aureus is isolated as the most common organism in all age categories. Other frequently involved organisms are listed in Table 1.
The most common site of bone infection is the metaphysis because of the blood supply that is characteristic in children (Figure 1). Infection begins in the metaphyseal venous sinusoid, where there is a change from high-flow arterioles to low-flow venous sinusoids. Evidence suggests that the reticuloendothelial system there is poorly developed with a lack of local resistance because of tissue macrophages. With the development of infection, there is thrombosis of the medullary vessels and suppression of macrophages.
The infection eventually tracks through the porous metaphyseal cortical surface and elevates the surrounding periosteum. If the metaphysis is intra-articular, the infection will then break into the joint and cause concurrent septic arthritis.
In neonates, the metaphyseal vessels penetrate directly into the chondroepiphysis, allowing an infection in the metaphysis to readily invade and destroy the chondroepiphysis and subsequently invade the joint. In older children, the physis serves as a mechanical barrier to the spread of infection.
A relevant history taking includes the time of disease onset, the nature and location of symptoms, the presence of constitutional symptoms, any recent infection or treatment with antibiotics, a refusal to move an extremity or bear weight, any recent trauma, foreign travel, and a known recent or remote exposure to infectious disease. Pertinent physical findings include temperature elevation or fever, focal tenderness, warmth, erythema, swelling, limited range of motion, pseudoparalysis, a limp, synovitis, rash, and joint effusion.
Initial laboratory studies include a complete blood cell count with differential, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level, and blood cultures.1,2Table 2 lists other studies that may be considered, along with their indications.3
Sequential determination of the CRP level perhaps is the most important laboratory test used in evaluating the patient's response to treatment. The CRP value begins to rise within 6 hours of the infection and increases several hundred-fold, reaching a peak within 36 to 50 hours of onset; with treatment, it returns to normal levels more quickly than does the ESR. Although blood cultures yield abnormal results in only 30% to 50% of cases, they are important in identifying some isolates of organisms that may serve as a guide to treatment.
Aspiration of joint fluid has the greatest yield of organisms in cases of suspected septic arthritis. Generally, white blood cell (WBC) counts higher than 50,000/mL with greater than 75% polymorphonuclear (PMN) cells suggest infection; those lower than 25,000/mL with less than 25% PMN cells suggest nonbacterial inflammation. In septic arthritis, lactate levels are elevated and glucose levels are lower than in the serum. In cases of suspected osteomyelitis, bone aspiration and culture at the time of biopsy may provide the only means of obtaining a positive culture and, therefore, should be considered.
Imaging. High-quality plain radiographs are essential in all cases; baseline anteroposterior and lateral projections should be obtained. Deep soft tissue swelling is the key finding early in the process of osteomyelitis. Changes in the bone resulting from osteomyelitis may not occur for 1 to 2 weeks after the onset of infection (Figure 2). The intraosseous abscess breaks through the cortical bone and collects subperiosteally; with time, a periosteal response occurs, making it visible on radiographs.

Figure 2 A

Figure 2 B
Ultrasonography is particularly well suited for young children of small body size in whom there is an increased ratio of cartilage to bone and a somewhat decreased ratio of fat to lean body mass. Its advantages include low cost, the absence of radiation exposure, its noninvasive nature, the ability to detect and localize joint fluid for aspiration in the hip under general anesthesia or sedation, and the ability to detect early changes in the deep soft tissues in osteomyelitis.4
Together with early periosteal thickening, juxtacortical soft tissue swelling is the earliest sign of acute osteomyelitis on ultrasonography. In septic arthritis, the presence of a joint effusion (pyarthrosis) in a patient with clinical signs of joint infection is confirmatory. Ultrasonography facilitates recognition and guided aspiration of joint fluid at an early stage, thereby allowing for early diagnosis and treatment.
Technetium (Tc) 99m-diphosphonate scanning often is used for evaluation of infection. This technique helps most in localizing the process if it is occurring in difficult-to-localize sites, such as the spine or pelvis. It consists of 3 phases: blood flow (essentially a radionuclide angiogram), blood pool (performed after a brief period to evaluate soft tissue pooling), and delayed images (performed 2 to 3 hours later to evaluate calcium phosphate deposition in bone). Gallium-67 (67Ga) citrate and indium-labeled leukocyte scanning has been proposed as a useful adjunctive study in cases in which the Tc scanning results are normal.5,6
Although Tc bone scanning is nonspecific, it is useful in defining multiple sites, such as in chronic recurrent multifocal osteomyelitis. Gadolinium imaging is useful in identifying abscess and delineating infectious borders.
In acute osteomyelitis, Tc bone scanning demonstrates increased uptake but may yield false-positive results associated with other noninfectious factors, such as trauma or tumors. In septic arthritis, bone scans may show decreased uptake early in the disease process and, later, increased uptake resulting from hyperemic response.
In some cases, 67Ga citrate scans may prove more informative than 99Tc methylene diphosphonate scans.7,8 Some physicians have found that indium-111-labeled WBC scans are less sensitive for spinal infection compared with conventional scans; however, these scans show a marked improvement in specificity compared with bone scans, particularly when complicating conditions are superimposed.
MRI is another powerful diagnostic tool for evaluation of infections. Typically, musculoskeletal infections are evaluated with low signal intensity on T1-weighted images and with increased marrow signal intensity on T2-weighted images.7,8 Of the advanced imaging studies currently available, MRI is the most helpful in defining pathoanatomy before surgery. MRI also may be used to observe abscess formation, subperiosteal fluid collection, marrow extension, and anatomic localization.
OSTEOMYELITIS
In this condition, the host can be infected through hematogenous spread (Figure 3) or direct inoculation. Although the exact time definitions vary, osteomyelitis is classified broadly as acute, subacute, and chronic (longer than 6 weeks) according to the time lapse between the suspected onset and the diagnosis.

Acute. In children with acute hematogenous osteomyelitis (AHO), by definition, symptoms develop acutely and usually are evaluated within the first several days after onset. The acute, focal bone pain usually is accompanied by systemic findings of fever or malaise.9 Clinical findings and a high index of suspicion are important in making the diagnosis. Consider the most relevant conditions in the differential diagnosis, such as trauma, leukemia, malignant bone tumors (eg, Ewing sarcoma or osteogenic sarcoma), and bone infarction resulting from sickle cell crisis.10
Antibiotic therapy is indicated; the dose and duration of antibiotic vary with the age of the child, site of infection, amount of destruction, treatment used, and response to treatment. Currently, clinical responses to treatment, as well as laboratory values (eg, CRP level), are used to determine when to switch to oral antibiotics after initiating intravenous treatment. The primary role of surgery is to evacuate purulent material with removal of necrotic bone. The diagnosis must be elucidated early to prevent increased morbidity and mortality.
Subacute. This category is thought to result from an altered host-pathogen relationship, such as a decrease in bacterial virulence or an increase in host resistance, or from a partially treated osteomyelitis.11S aureus is the most common pathogen cultured from this lesion.
Subacute hematogenous osteomyelitis differs from AHO in that the child usually is afebrile, has minimal pain, and is generally less symp- tomatic. A gradual and insidious type of extremity pain without signs of systemic illness develops in children who have subacute osteomyelitis.
At presentation, bone pain usually is noted for at least 2 to 3 weeks or even several months. Laboratory test results often are unremarkable, although the ESR or CRP level may be elevated. Unlike in patients who have AHO, radiographs usually show bony changes at presentation.
The key to treating children who have subacute osteomyelitis is establishing the correct diagnosis early and ruling out bony tumors. Treatment consists of appropriate antibiotics and decompression/debridement of sequestered purulent material or necrotic bone or both (Figure 4). Because biopsy often is needed for diagnosis (to differentiate from a neoplastic process), decompression/debridement usually is done in the same surgical setting as the biopsy.
Figure 4 A
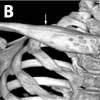
Figure 4 B

Figure 4 C
Chronic. In its classic form, chronic osteomyelitis usually is the result of acute hematogenous or post-traumatic osteomyelitis; manifestations of chronic osteomyelitis are now rare in North America. The condition is present when symptoms have persisted for longer than 6 weeks before therapy, when bone infection has been present for at least 1 month after surgery for trauma, or when the existing osteomyelitis was managed inadequately.
Classic features include the presence of dead bone (sequestrum) (Figure 5), often surrounded by gross purulence, and reactive new bone (involucrum). Draining sinuses may erupt as the infection erodes through overlying tissue planes. The diagnosis includes biopsy by intraoperative frozen section with tissue cultures for possible underlying organisms (aerobic, anaerobic and, if suspected, even fungal organisms).

Principles of treatment include decompression of abscess; debridement of all necrotic tissue, leaving behind viable bone and periosteum; and identification of the causal organism to ensure that the most appropriate antibiotic is selected for long-term treatment. Attempts to reconstruct usually should be made after the infection has resolved.
Special forms and associated conditions. Several special, rare forms of osteomyelitis may occur in children. Understanding of their characteristics and how they differ from more common osteomyelitis is important in making the diagnosis.
Neonatal and infantile infections. Although the neonatal period usually is defined as the first 28 days of life, the pathogenesis of neonatal infections extends over the first 6 to 10 weeks. The characteristics of neonatal osteomyelitis vary according to whether it was hospital- or community-acquired. Almost half of infants with neonatal osteomyelitis have multiple sites of infection.12
Causative organisms probably include S aureus, group B Streptococcus, and Gram-negative bacteria.13Candida albicans also may be involved in patients who are receiving prolonged broad-spectrum antibiotic treatment and in immunosuppressed patients. Manifestation of their musculoskeletal infection usually occurs between 2 and 4 weeks of life but may occur up to 10 weeks after delivery.
Because neonates with osteomyelitis have immature immune systems, they have a less intense inflammatory response and are more susceptible to organisms that are less virulent in older children. Antibiotic selection should be considered carefully with the help of an infectious disease specialist and a neonatal intensivist, especially for hospital-acquired sepsis.
Chronic recurrent multifocal osteomyelitis (CRMO). This is a condition of insidious onset that involves multiple bone locations and is associated with pain and malaise. Related conditions include SAPHO syndrome (Synovitis, Acne, Palmoplantar pustulosis, Hyperostosis, Osteitis) and other inflammatory disorders, such as peripheral arthritis, sacroiliitis, psoriasis, pyoderma gangrenosum, and inflammatory bowel disease.
The histologic and radiographic findings usually are suggestive of CRMO. However, blood and bone culture results usually are normal and antibiotics have not been found to be necessary in treatment.
Usually, treatment consists of NSAIDs and local management of the symptoms.14 Some investigators consider an autoimmune pathogenesis.15 The general outcome is considered to be good, and the disease is self-limited.
Sickle cell disease. Persons with sickle cell disease are predisposed to osteomyelitis secondary to ischemic injury of both bone and the GI tract. This injury results in a high incidence of seeding of infarct beds with GI flora, most commonly Salmonella, as opposed to the more common cause of osteomyelitis in the general population, S aureus.
Salmonella osteomyelitis typically is an infection of the diaphysis of the long bones. The most common bones involved are the femur and the humerus. Other bones commonly involved are the tibia, radius, lumbar vertebrae, and ulna. Most patients have involvement of only 1 bone, although multiple bone involvement also has been reported. The duration of symptoms may range from a few months to several years; the symptom-free interval between the initial illness and the osteomyelitis may be as long as 25 years.
Salmonella species and S aureus are the most common causative organisms of sickle cell disease.16 Empiric antibiotic selection should cover both organisms until specific culture results are available. Initial use of oxacillin and ampicillin or chloramphenicol or cefotaxime, 100 to 200 mg/kg for 24 hours, is considered appropriate.
The initial management of musculoskeletal pain in children who have sickle cell bone crisis should include oxygen, hydration, and analgesics. If the children do not improve within 1 to 3 days and have persistent fever and the appearance of systemic illness, infection should be suspected as the underlying cause. A combination sequential radionuclide bone marrow and bone scan in children may help differentiate bone infarct from bone pain that is caused by osteomyelitis.17
SEPTIC ARTHRITIS
This condition occurs as a result of primary seeding of the synovial membrane, most often from hematogenous infection or infection in the adjacent metaphyseal bone. Typically, the disease has an acute onset in which the child is irritable, febrile, and anorexic. On examination, active or passive motion of the involved joint, such as short-arc rotation of the hip, causes severe pain. Neonates may display only "failure to thrive," anorexia, irritability, and lethargy and may not move the affected limb (pseudoparalysis).
Destruction of the cartilage that results from proteolytic enzymes released from synovial cells evolves within 3 to 5 days. The diagnosis of septic arthritis hinges on elevated laboratory test results (ESR, greater than 40 mm/h; WBC count, higher than 12,000/mL) and a clinical presentation of fever and non-weight bearing on the infected joint; however, atypical presentations are possible.18
The cornerstone of treatment is arthrotomy and irrigation of the involved joint, along with appropriate constitutional support, including antibiotics and hydration. The traditional use of parenteral antibiotics for 4 or 6 weeks for septic arthritis has been challenged in favor of a shorter duration and earlier shifting from intravenous to oral antibiotics for less expensive and more convenient and effective alternatives.19
TREATMENT
Antibiotic treatment. To manage the most common organisms in each age category adequately, empiric selection of an antibiotic is relied on while awaiting culture results and for patients with normal culture results (see Table 1). If an organism is identified, however, there is greater confidence that the antibiotic selected has the appropriate spectrum of coverage.
Currently, the clinical response to treatment and laboratory values (eg, serial CRP levels) are used to determine whether switching to oral medications is appropriate. During the initial treatment period, when close monitoring of the clinical response and serial CRP levels are necessary, intravenous antibiotic delivery usually is preferred. Consultation with an expert in infectious diseases to determine the optimal duration of parenteral therapy is recommended.
During the acute period of illness--characterized by fever; irritability; inflammation; and an elevated WBC count, CRP level, and ESR--starting intravenous antibiotics is recommended. There is no established duration of treatment, because most often the approach varies with the age and general well-being of the child, site of infection, amount of destruction, treatment used, and response to treatment. Generally, the duration of antibiotic therapy is about 5 to 7 weeks for uncomplicated osteomyelitis and about 3 to 5 weeks for uncomplicated septic arthritis.19,20 Close clinical and laboratory monitoring during the treatment course helps identify patients who may benefit from a longer duration of treatment or another treatment regimen.
Surgery. Many authors agree that in cases in which there is soft tissue or intraosseous abscess formation, surgical decompression is necessary for improvement and eventual resolution of infection. Although some children respond well to medical treatment alone, surgery plays a key role (eg, in early management of septic arthritis). It has been suggested that if significant improvement has not resulted within 36 to 48 hours, surgical exploration and debridement should be considered, regardless of radiographic features. Clearly, these decisions need to be individualized, taking into account all clinical, laboratory, and radiologic information.
References:
REFERENCES:
1.
Unkila-Kallio L, Kallio MJ, Eskola J, Peltola H. Serum C-reactive protein, erythrocyte sedimentation rate, and white blood cell count in acute hematogenous osteomyelitis of children.
Pediatrics.
1994; 93:59-62.
2.
Unkila-Kallio L, Kallio MJ, Peltola H. The usefulness of C-reactive protein levels in the identification of concurrent septic arthritis in children who have acute hematogenous osteomyelitis: a comparison with the usefulness of the erythrocyte sedimentation rate and the white blood-cell count.
J Bone Joint Surg.
1994;76A:848-853.
3.
Copley L, Dormans JP. Musculoskeletal infections. In Dormans JP, ed.
Pediatric Orthopaedics: Core Knowledge in Orthopaedics.
Philadelphia: Elsevier Mosby; 2005:337-352.
4.
Mah ET, LeQuesne GW, Gent RJ, Paterson DC. Ultrasonic features of acute osteomyelitis in children.
J Bone Joint Surg.
1994;76B:969-974.
5.
Love C, Palestro CJ. Radionuclide imaging of infection.
J Nucl Med Technol.
2004;32:47-57.
6.
Lewin JS, Rosenfield NS, Hoffer PB, Downing D. Acute osteomyelitis in children: combined Tc-99m and Ga-67 imaging.
Pediatr Radiol.
1986;158:795-804.
7.
Erdman WA, Tamburro F, Jayson HT, et al. Osteomyelitis: characteristics and pitfalls of diagnosis with MR imaging.
Radiology.
1991;180:533-539.
8.
Mazur JM, Ross G, Cummings J, et al. Useful-ness of magnetic resonance imaging for the diagno-sis of acute musculoskeletal infections in children.
J Pediatr Orthop.
1995;15:144-147.
9.
Mustafa MM, Saez-Llorens X, McCracken GH Jr, Nelson JD. Acute hematogenous pelvic osteomyelitis in infants and children.
Pediatr Infect Dis J.
1990; 9:416-421.
10.
Dormans JP, Drummond DS. Pediatric hematogenous osteomyelitis: new trends in presentation, diagnosis, and treatment.
J Am Acad Orthop Surg.
1994;2:333-341.
11.
Roberts JM, Drummond DS, Breed AL, Chesney J. Subacute hematogenous osteomyelitis in children: a retrospective study.
J Pediatr Orthop.
1982; 2:249-254.
12.
Narang A, Mukhopadhyay K, Kumar P, Bhakoo ON. Bone and joint infection in neonates.
Indian J Pediatr.
1998;65:461-464.
13.
Baevsky RH. Neonatal group B beta-hemolytic streptococcus osteomyelitis.
Am J Emerg Med.
1999; 17:619-622.
14.
McCarthy JJ, Dormans JP, Kozin SH, Pizzutillo PD. Musculoskeletal infections in children: basic treatment principles and recent advancements.
Instr Course Lect.
2005;54:515-528.
15.
Gallagher KT, Roberts RL, MacFarlane JA, Stiehm ER. Treatment of chronic recurrent multifocal osteomyelitis with interferon gamma.
J Pediatr.
1997;131:470-472.
16.
Chambers JB, Forsythe DA, Bertrand SL, et al. Retrospective review of osteoarticular infections in a pediatric sickle cell age group.
J Pediatr Orthop.
2000;20:682-685.
17.
Skaggs DL, Kim SK, Greene NW, et al. Differentiation between bone infarction and acute osteomyelitis in children with sickle-cell disease with use of sequential radionuclide bone-marrow and bone scans.
J Bone Joint Surg.
2001;83A:1810-1813.
18.
Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm.
J Bone Joint Surg.
1999;81A:1662-1670.
19.
Kim HK, Alman B, Cole WG. A shortened course of parenteral antibiotic therapy in the management of acute septic arthritis of the hip.
J Pediatr Orthop.
2000;20:44-47.
20.
Jackson MA, Nelson JD. Etiology and medical management of acute suppurative bone and joint infections in pediatric patients.
J Pediatr Orthop.
1982;2:313-323.


















