Translocation Down (Trisomy 21) Syndrome
Six-year-old East Indian boy delivered by normal spontaneous vaginal delivery to a para 3, gravida 2, 42-year-old mother following uncomplicated, full-term pregnancy. Apgar scores: 9 and 9, at 1 and 5 minutes, respectively. Birth weight, 2.5 kg. Infant hypotonic at birth with numerous dysmorphic features. Delayed developmental milestones; IQ measured at 80.
HISTORY
Six-year-old East Indian boy delivered by normal spontaneous vaginal delivery to a para 3, gravida 2, 42-year-old mother following uncomplicated, full-term pregnancy. Apgar scores: 9 and 9, at 1 and 5 minutes, respectively. Birth weight, 2.5 kg. Infant hypotonic at birth with numerous dysmorphic features. Delayed developmental milestones; IQ measured at 80.
No family history of chromosomal abnormality.
PHYSICAL EXAMINATION
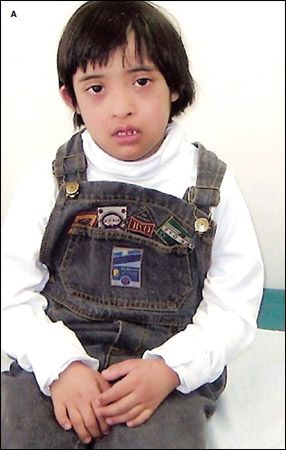
Dysmorphic features include brachycephaly, epicanthal folds, up-slanting palpebral fissures (A); short, broad hands; bilateral single palmar crease; and bilateral single flexion crease of the fifth finger (B).

In 1866, John Langdon Haydon Down, a British physician, described the clinical characteristics of the syndrome that now bears his name.1 The syndrome is characterized by mental retardation, dysmorphic facial features, and other distinctive phenotypic traits. In 1959, Lejeune and colleagues2 reported that the syndrome is caused by an extra copy of chromosome 21. Down (trisomy 21) syndrome is the most common aneuploidy in humans.
"WHAT'S YOUR DIAGNOSIS?"
ANSWER: DOWN SYNDROME EPIDEMIOLOGY
The overall incidence is approximately 1 in 700 live births.3 The risk of Down syndrome is directly related tomaternal age. A meta-analysis of 9 published studies on the birth prevalence of Down syndrome reveals that the incidence rises from 1 in 1449 live births at a maternal age of 20 years to 1 in 26 live births at amaternal age of 45 years.3 The incidence is much higher if spontaneous and therapeutic abortion isconsidered.More than 75% of pregnancies with a trisomy 21 fetus are spontaneouslyaborted early in pregnancy.4,5
There is no association with paternal age, birth order, ethnicity, or country of birth.6
ETIOLOGY
Down syndrome is caused by the presence of extra genetic material from chromosome 21. The Down syndrome-specific region has been mapped to 21q22.2-22.3.7 In approximately 95% of cases, the condition is the result of non-familial trisomy 21 or non-disjunction of chromosome 21 during the meiotic formation of the oocyte orspermatocyte.8,9 DNA testing has shown that the oocyte is the location of the non-disjunction in about 92% of cases.10 Theexact mechanism for this meiotic error is not understood.
In approximately 3% to 4% of cases, the extra genetic material is the result of an unbalanced translocation between chromosome 21 and another acrocentric chromosome--usually chromosome 14--which is referred to as the robertsonian translocation.8 Approximately 75% of translocations arise de novo; 25% are inherited from a translocation carrier parent.8 Non-homologous translocations that involve more than 2 different acrocentric chromosomes are more frequent than homologous translocations.11 In the remaining 1% to 2% of cases, 2 cell lines are present--one normal and the other trisomy 21; this is referred to as mosaicism.9
CLINICAL FEATURES
The phenotype in translocation Down syndrome is indistinguishable from that in regular trisomy 21 syndrome. Patients with mosaicism are usually phenotypically less severely affected.
General. Hypotonia that improves with age, short stature, obesity during adolescence, hypermobility of the joints with laxity of the ligaments, cheerfulness, gentleness, and a patient nature.
CNS. Mental retardation.
Skull and face. Brachycephaly with relatively flat occiput; microcephaly; large fontanels that close later than normal; up-slanting palpebral fissures; inner epicanthal folds; hypoplasia of frontal, sphenoidal, and maxillary sinuses; midfacial hypoplasia; and a flat nasal bridge.
Eyes. Speckled iris (Brushfield spots), refractive errors, strabismus, nystagmus, and cataract.
Ears. Small ear lobes with overfolding of an angulated upper helix, and sensorineural hearing loss.
Mouth. Macroglossia, fissures, furrowed tongue, and a high arched palate.
Teeth. Delayed eruption, microdontia, and hypoplastic and hypocalcified teeth.
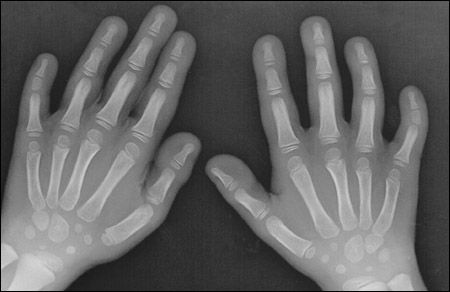
Figure – Radiograph shows hypoplasia of the middle phalanges of the fifth fingers.
Neck. Short neck with loose overlying skin.
Skin. Cutis marmorata, xerosis, and hyperkeratosis.
Hands and feet. Short and broad hands, hypoplasia of the midphalanx of the fifth finger (Figure), clinodactyly of the fifth finger, single transverse palmar or simian crease, distal palmar axial triradius, ulnar loops on fingertips, and a wide space between the first 2 toes.
Pelvis. Hypoplasia of the pelvis, with outward lateral flaring of the iliac wings, and a shallow acetabular angle.
Genitalia. Micropenis and decreased testicular volume.
ASSOCIATED ANOMALIES
Congenital heart disease occurs in 40% to 60% of patients with Down syndrome. The most common problems are endocardial cushion defect, ventricular septal defect, atrial septal defect, and tetralogy of Fallot.12 GI anomalies occur in 12% of patients and include tracheoesophageal fistula, duodenal atresia orstenosis, pyloric stenosis, annular pancreas, Meckel diverticulum, omphalocele, Hirschsprung disease, and imperforate anus.4,13,14 Other associated anomalies include renal hypoplasia, obstructive uropathy, cryptorchidism, diastasis recti, umbilical hernia, choanal atresia, preaxial polydactyly, and prune belly syndrome.15,16
COMPLICATIONS
Persons with Down syndrome are susceptible to infection and are at increased risk for otitis media, periodontal disease, and fungal infections of the skin and nails. They also have an increased risk of autism, obsessive-compulsive disorder, hearing loss from recurrent otitis media, seizures, presenile dementia orAlzheimer disease, spinal cord compression from atlantoaxial instability, slipped capital femoral epiphysis, osteoporosis, obstructive sleep apnea, male infertility, anovulation,glaucoma, glomerulonephritis, hypothyroidism, diabetes mellitus, celiac disease, mitral valve prolapse, leukemia, leukemoid reaction, and retinoblastoma.8,14,17-19
Mortality associated with Down syndrome has improved appreciably over the past few decades. In the United States, the median age at death was 25 years in 1983; in 1997, the median age at death was 49 years. The most common causes of death are congenital heart disease and respiratory infection.20
DIAGNOSIS AND DIFFERENTIAL DIAGNOSIS
The diagnosis is usually based on the presence of the typical dysmorphic features. Hypothyroidism, Beckwith-Wiedemann syndrome, Zellweger syndrome, Smith-Magenis syndrome, and tetrasomy 12p can be distinguished by the unique clinical features of these conditions.11
The diagnosis of Down syndrome should be confirmed with cytogenetic studies, which also help determine the risk of recurrence. Karyotyping of the parents should be performed when a translocation is identified.
PRENATAL DIAGNOSIS
A low maternal serum level of a-fetoprotein and unconjugated estriol, and an elevated maternal serum level of b-human chorionic gonadotropin are biochemical markers for Down syndrome. These are often referred to as the "triple test."4,5 Concerned women younger than 35 years should be offered maternal serum screening at 16 to 18 weeks' gestation. When the result of the triple test is positive, the likelihood of Down syndrome is 2%.5 When these abnormalities are present together with fetal ultrasonographic evidence of nuchal translucency (caused by subcutaneous edema at the base of the skull), the risk of Down syndrome is about 80% to 85%.19
Amniocentesis or chorionic villus sampling to examine the fetal chromosomes should be offered to women who will be 35 years or older on their delivery due date and to those with abnormal maternal serum screening results or prenatal ultrasonography.5 Chorionic villus sampling offers the opportunity for first-trimester diagnosis, when elective pregnancy termination carries the lowest risk of maternal morbidity.5
In a fetus with established Down syndrome, a fetal echocardiogram should be performed at 20 weeks' gestation to look for cardiac malformations. Ultrasonography should be performed at 28 to 32 weeks' gestation to monitor growth and to screen forduodenal atresia.
MANAGEMENT
A multidisciplinary approach is important and should include a psychologist, occupational therapist, social worker, schoolteacher, and various pediatric specialists. All children with Down syndrome should have a thorough physical examination, an echocardiogram, and an auditory brainstem response in the neonatal period.4,8 Thyroid function tests need to be repeated when the child is 6 months old and yearly thereafter.
Within the first year, the child needs to be assessed by a pediatric ophthalmologist or by an ophthalmologist who has experience with disabled children. Each annual assessment should include an age-appropriate developmental and physical examination, complete blood count, audiologic evaluation, and ophthalmologic assessment.8
Specific growth charts are available for children with Down syndrome and should be used if growth delay is suspected.12 If growth delay is present, a careful evaluation is necessary to search for an underlying medical condition as a cause of the problem.
Radiographs to investigate for atlantoaxial instability should be obtained when the child is 3 to 5 years old.Appropriate skin care should be discussed.8 Regular dental care helps prevent periodontal disease.
Education and rehabilitation need to be provided to maximize the child's potential.21 Some children with Down syndrome benefit from regular class participation with additional support; others requirespecial class placement.21 Adolescents require sex education that includes information oncontraception, sexually transmitted diseases, and the risk of exploitation.
RECURRENCE RISK
The risk of recurrence of trisomy 21 syndrome in a subsequent pregnancy increases to 1% above the baseline risk determined by the maternal age.5,11,12 After a secondtrisomy 21 pregnancy, the risk increases to10% above that determined by maternal age.22 If the mother has trisomy 21 syndrome, there is a 50% chance that her child will be affected.4,22
In Down syndrome children with arobertsonian translocation, the translocation is presumed to arise de novo if both parents have a normal karyotype. The recurrence risk in this setting is about 2% to 3%.5,11 When one parent is a robertsonian translocation carrier, the risk of recurrence depends on the sex of the carrier parent and the specific chromosome involved in the translocation.11 If the mother is a rob(14q21q) carrier, the risk of recurrence is 10% to 15%.4,11,22 If the father is a rob(14q21q) carrier, the risk of recurrence is less than 5%.4,11,22 If the parent has a 21:21 translocation, the risk of recurrence is virtually 100%.4,11,22
References:
REFERENCES:
1.
Down JL. Observations on an ethnic classification of idiots.
London Hospital Reports. 1866;3:259-262.
2. Lejeune J, Gautier M, Turpin R. Etude des chromosomes somatiques de neuf enfants mongoliens. Compte Rendu d'Acad Sci.1959;248:1721-1722.
3. Bray I, Wright DE, Davies C, Hook EB. Joint estimation of Down syndrome risk and ascertainment rates: a meta-analysis of nine published data sets. Prenat Diag.1998;18:9-20.
4. Chen H. Down syndrome. In: Chen H, ed. Atlas of Genetic Diagnosis and Counseling.Totowa, NJ: Humana Press; 2006:295-300.
5. Newberger DS. Down syndrome: prenatal risk assessment and diagnosis. Am Fam Physician.2000;62:825-832.
6. Carothers AD, Castilla EE, Dutra MG, Hook EB. Search for ethnic, geographic, and other factors in the epidemiology of Down syndrome in South America: analysis of data from the ECLAMC project, 1967-1997. Am J Med Genet. 2001; 103:149-156.
7. Rogers PT. Down syndrome: managing the child and family. In: Hoekelman RA, Adam HM, Nelson NM, et al, eds. Primary Pediatric Care.Philadelphia: Mosby; 2001:1462-1470.
8. American Academy of Pediatrics. Committee on Genetics. Health supervision for children with Down syndrome. Pediatrics.2001;107:442-449.
9. Leung AK, Kao CP. Hereditary childhood disorders. Consultant.1998;38: 1929-1933.
10. Ballesta F, Queralt R, Gomez D, et al. Parental origin and meiotic stage of non-disjunction in 139 cases of trisomy 21. Ann Genet.1999;42:11-15.
11. Tolmie JL. Trisomy 21 Down syndrome. In: Rimoin DL, Connor JM, Pyeritz RE, et al, eds. Emery and Rimoin's Principles and Practice of Medical Genetics. Philadelphia: Churchill Livingstone; 2002:1131-1183.
12. Tyler C, Edman JC. Down syndrome, Turner syndrome, and Klinefelter syndrome: primary care throughout the life span. Prim Care Clin Office Pract.2004;31:627-648.
13. Leung AK, Mui CY, Lau JT. Hirschsprung's disease and mongolism. J Natl Med Assoc.1986;78:443-446.
14. Jones KL. Down syndrome (trisomy 21 syndrome). In: Jones KL, ed. Smith's Recognizable Patterns of Human Malformation.Philadelphia: Elsevier Saunders; 2006:7-12.
15. Ariel I, Wells TR, Landing BH, Singer DB. The urinary system in Down syndrome: a study of 124 autopsy cases. Pediatr Pathol.1991;11:879-888.
16. Mercer ES, Broecker B, Smith EA, et al. Urological manifestations of Down syndrome. J Urol. 2004;171:1250-1253.
17. Robson WL, Leung AK, Woodman RC, Trevenen CL. Anti-neutrophil cytoplasmic antibody associated glomerulonephritis in a patient with Down's syndrome. Pediatr Nephrol.1995;9:204-205.
18. Robson WL, Leung AK. Down's syndrome and renal abnormalities. Pediatr Nephrol.1993;7:775.
19. Roizen NJ, Patterson D. Down's syndrome. Lancet. 2003;361:1281-1289.
20. Yang Q, Rasmussen SA, Friedman JM. Mortality associated with Down's syndrome in the USA from 1983 to 1997: a population-based study. Lancet.2002; 359:1019-1025.
21. Leung AK, Robson WL, Fagan J, et al. Mental retardation. J R Soc Health.1995;115:31-32, 37-39.
22. Firth HV, Hurst JA, Hall JG. Down syndrome (trisomy 21). In: Firth HV, Hurst JA, Hall JG, eds. Oxford Desk Reference: Clinical Genetics. Oxford, England: Oxford University Press; 2005:524-525.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.