Spondylolysis: Underrecognized cause of low back pain
When teenaged athletes complain of lumbar back pain that worsens with activity, there should be a high index of suspicion for a spondylolysis.
Figure 1
Table
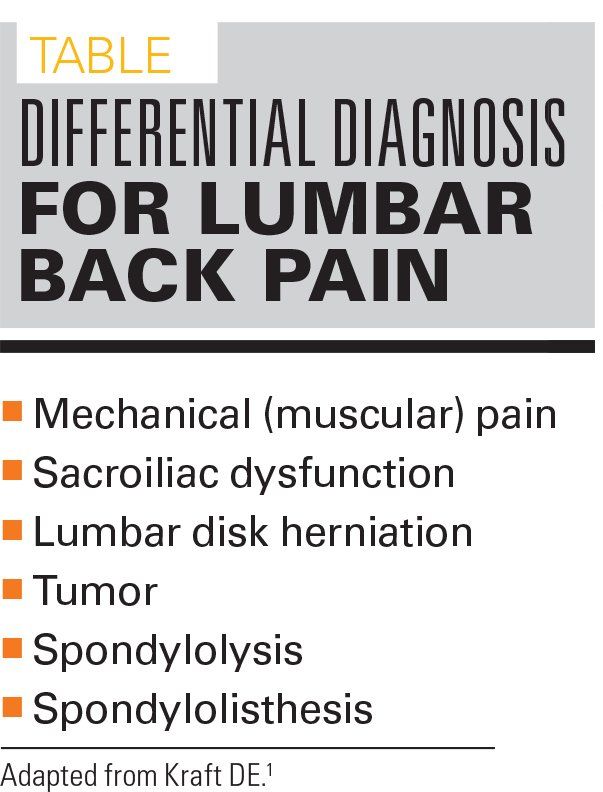
Figure 2
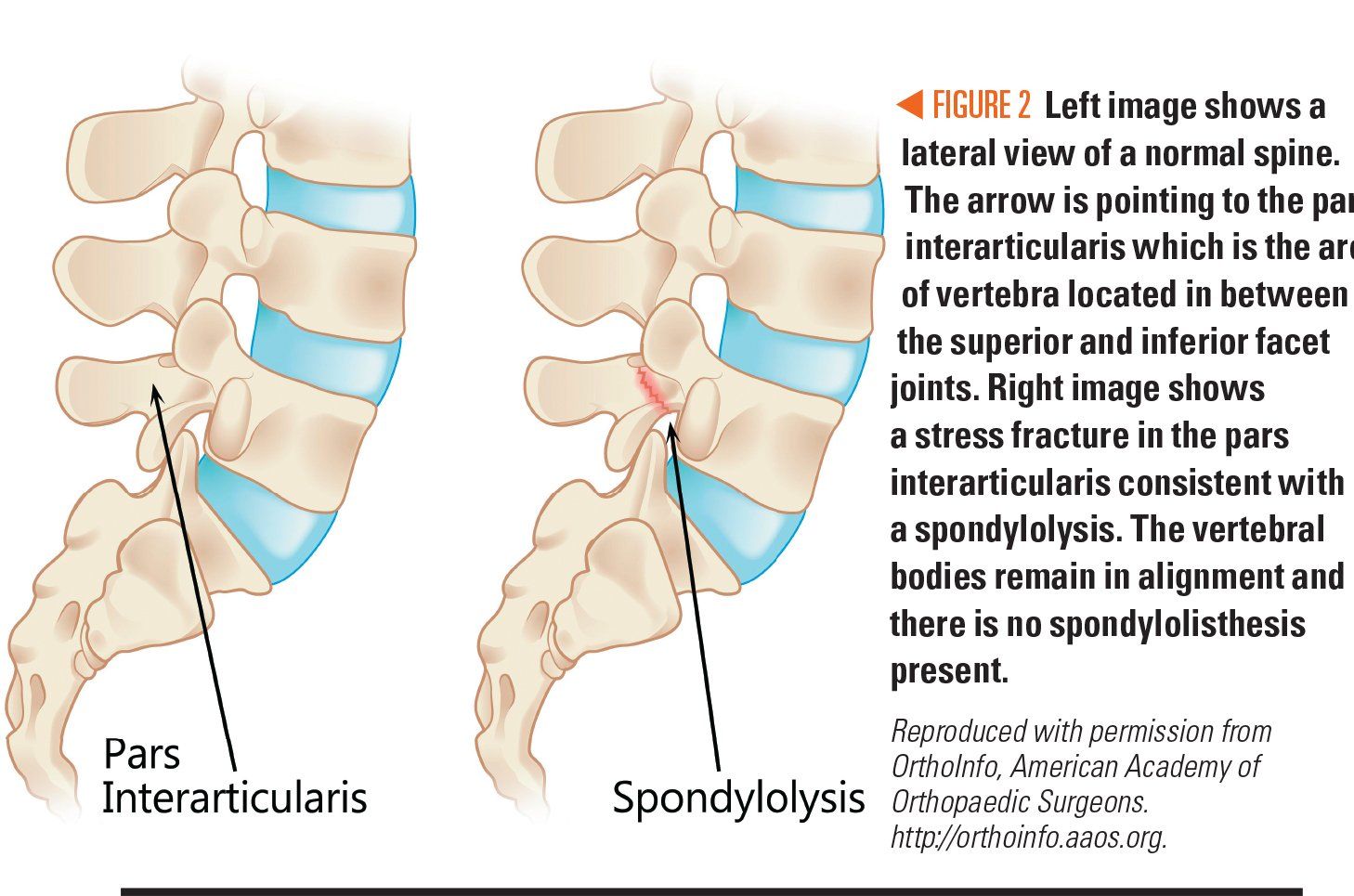
Figure 3
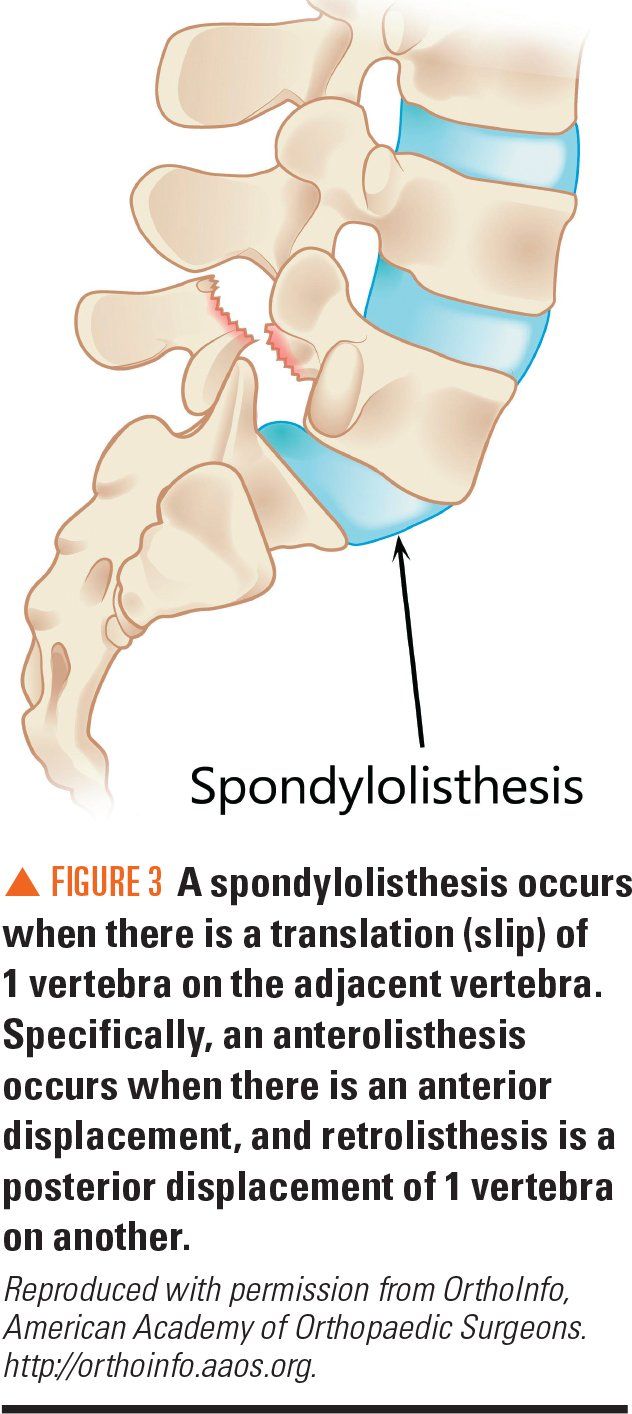
Figure 4
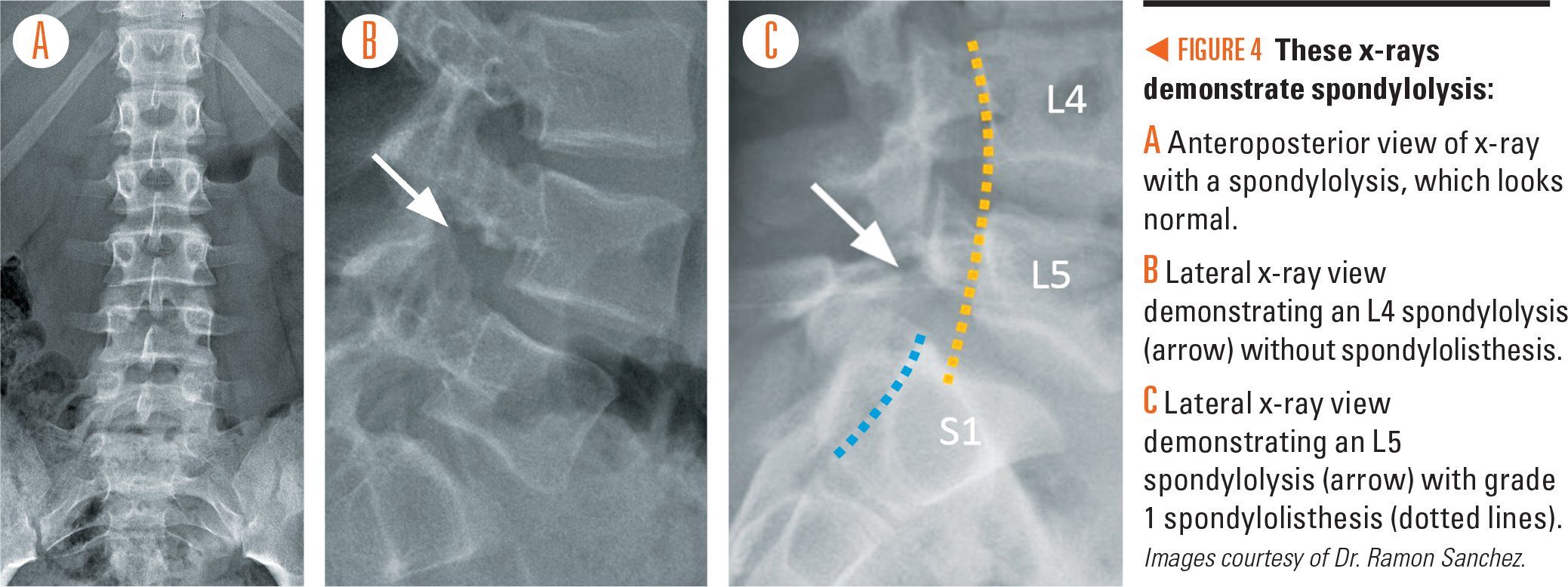
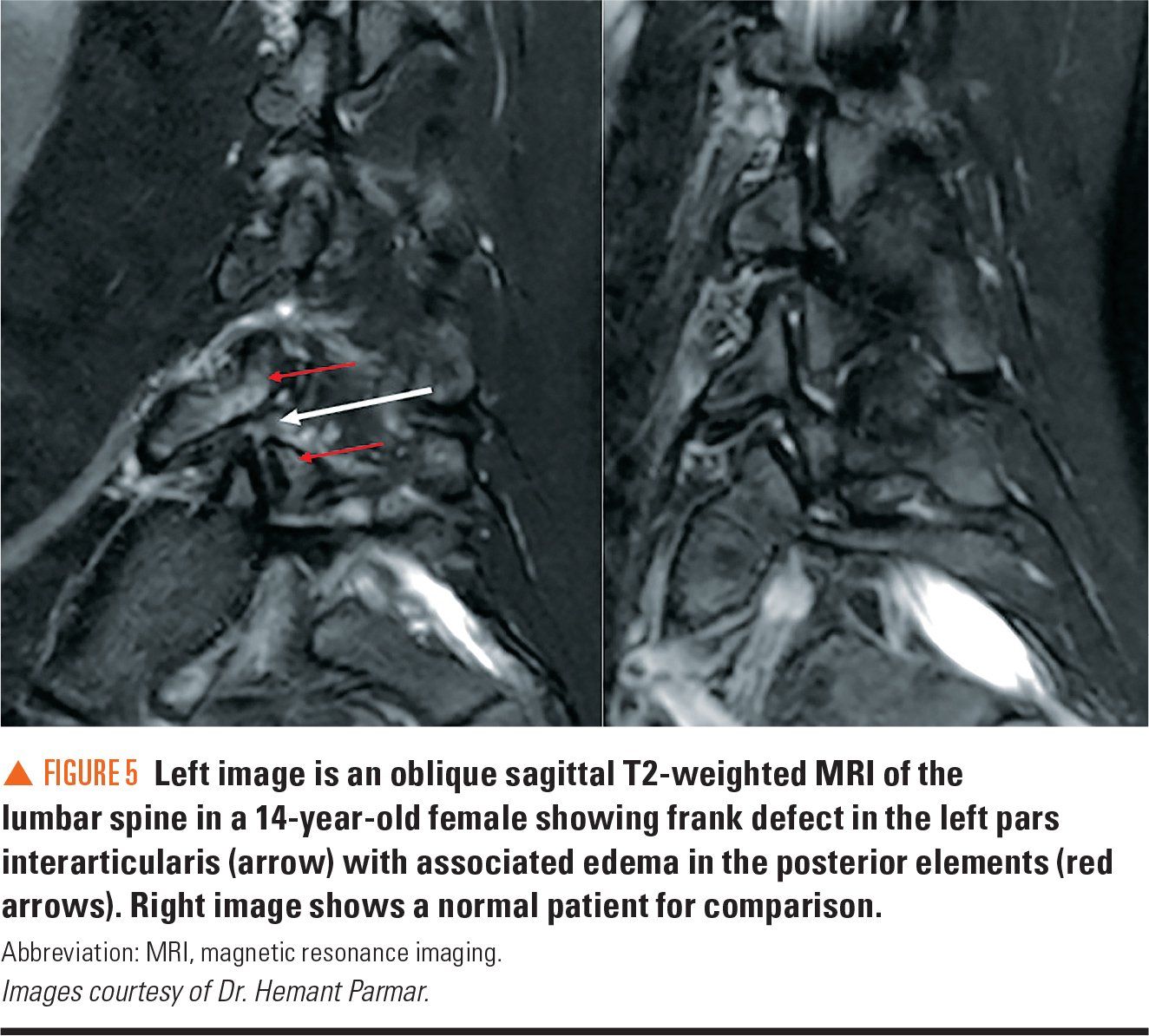
Figure 5
ICD-10 codes
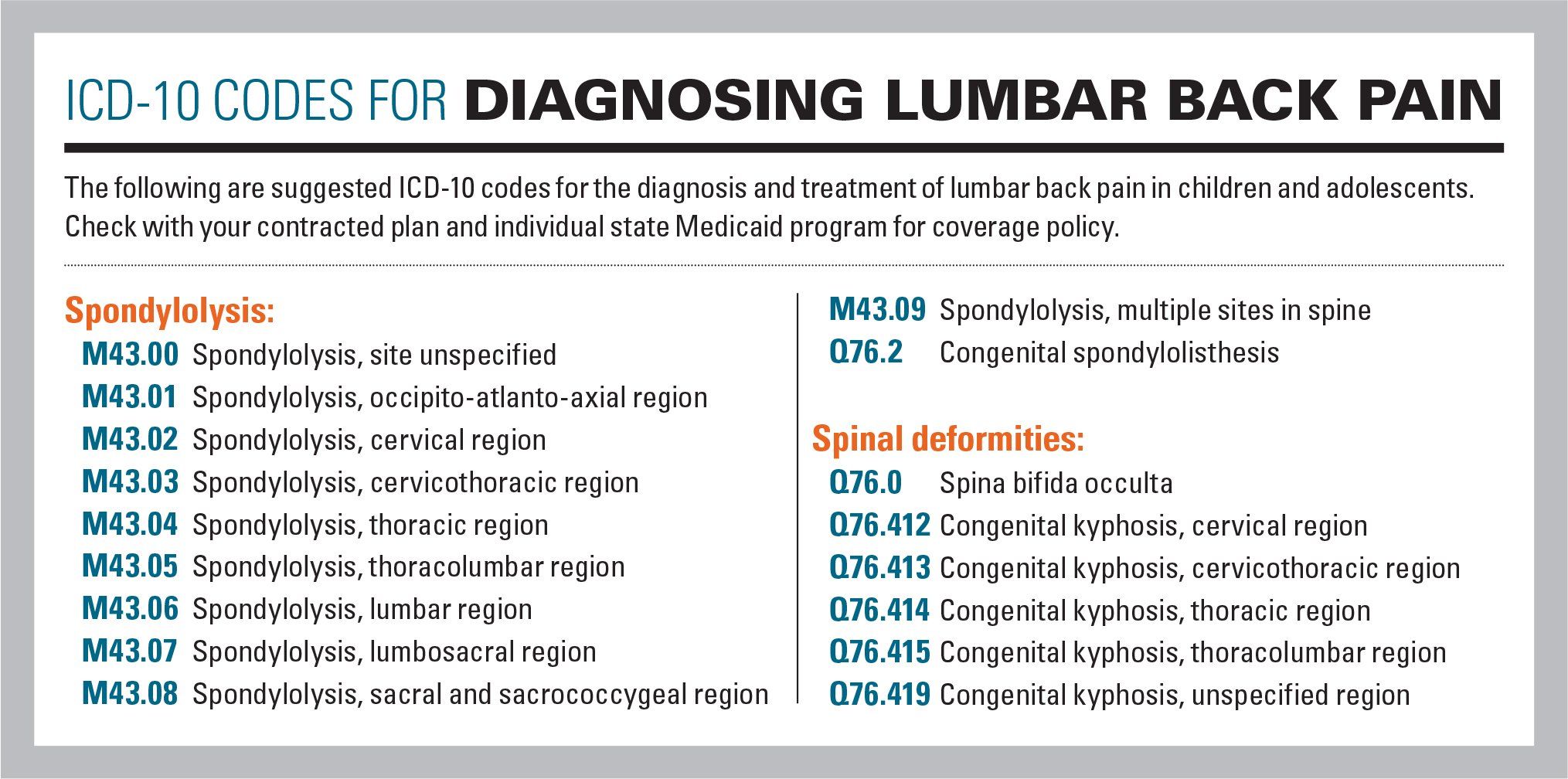
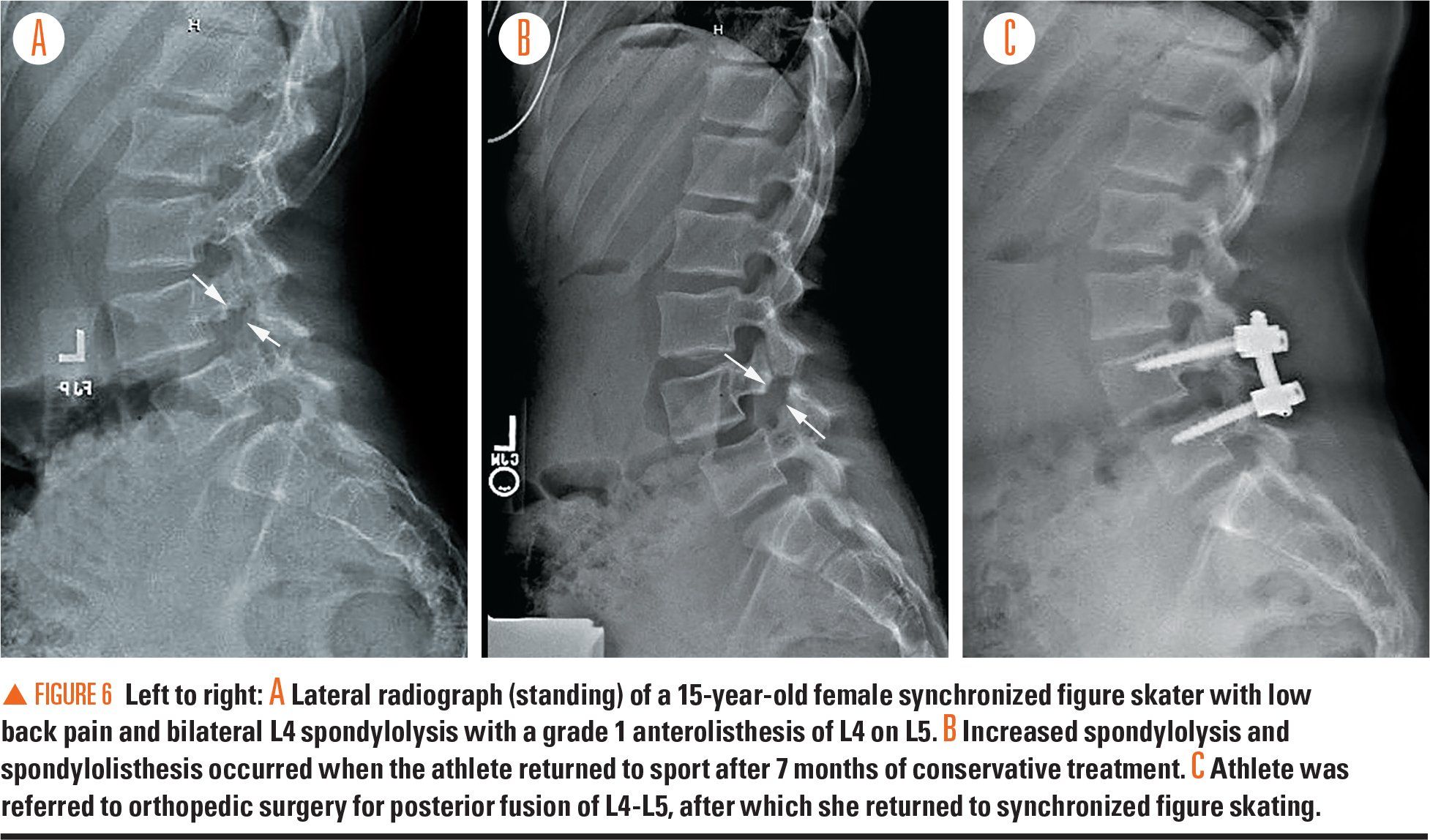
Figure 6
A 15-year-old female competitive gymnast presents to the clinic with 3 months’ history of right-sided lumbar back pain. She reports no specific injury but the pain has been worsening over time and has not improved despite 2 weeks of rest. The pain worsens with extension maneuvers such as back walkovers, back flips, and back handsprings. The pain is sharp in quality and does not radiate down her legs. Ice, heat, and anti-inflammatory medications have not helped. She denies neck pain, limping, nighttime pain, and incontinence of bowel or bladder.
Exam and workup
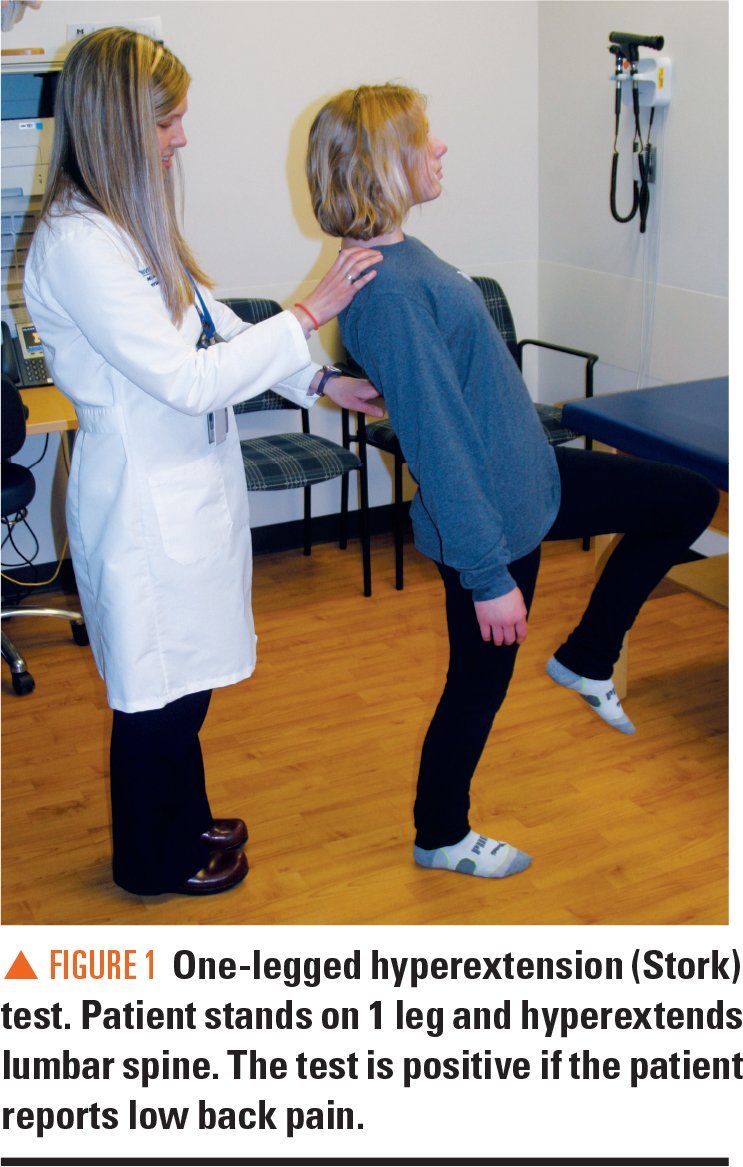
A physical exam reveals tenderness on palpation at the midline of the L4-L5 level and pain with lumbar extension. The patient also has a positive 1-legged hyperextension (Stork) test consisting of pain when she lifts up her right leg, flexing at the hip and knee while extending her lumbar spine (Figure 1). She has 5/5 strength in her lower extremities bilaterally and symmetric 2/4 patellar and Achilles deep tendon reflexes.
Possible etiologies of this athlete’s pain include mechanical (muscular) back pain, sacroiliac dysfunction, lumbar disk herniation, spondylolysis, and spondylolisthesis (Table).1 Although mechanical back pain is most likely, pain with extension in a gymnast raises concerns about the possibility of a spondylolysis with or without spondylolisthesis.
A FABER test (hip is Flexed, ABducted, and Externally Rotated to evaluate for development of pain at the ipsilateral sacroiliac joint) may help evaluate for sacroiliac joint involvement in addition to palpation and compression of the joint. This gymnast does not have a positive FABER test, which makes sacroiliac joint dysfunction less likely. Disk herniation often causes pain with forward flexion and this athlete’s pain worsens with lumbar extension, making disk herniation less likely and the possibility of spondylolysis more concerning.
Initial diagnostic workup consisting of lumbosacral radiographs (anteroposterior [AP] and lateral views) is normal, which rules out spondylolisthesis. A spondylolysis, however is not always apparent on x-ray. Given a high suspicion for this condition, and this athlete’s desire to continue to participate in her sport, the next step is to proceed with magnetic resonance imaging (MRI), which confirms a spondylolysis of the right L5 vertebra.
What is spondylolysis?
The most common identifiable etiology of lumbar back pain in adolescents is spondylolysis. One recent study identified spondylolysis as the cause in 30% of adolescent athletes presenting with lumbar back pain.2 Another study found that 40% of pediatric patients presenting for evaluation for lumbar back pain had a spondylolysis (9% of elementary students, 60% of junior high students, and 32% of high school students had a spondylolysis).3 In this study, all patients who had spondylolysis were athletes. The study was performed in an orthopedic clinic, but general pediatricians should consider this injury in patients presenting for evaluation for low back pain.
A spondylolysis is a stress fracture to the pars interarticularis, which is a portion of the vertebral bone that joins the facet joints in the posterior aspect of the spine (Figure 2). A spondylolysis is usually caused by chronic stress applied to the lumbar spine, most likely due to repetitive lumbar hyperextension and rotation that cause shear and compressive forces on the pars interarticularis. In a small proportion of cases, an acute incident may cause this injury. A spondylolysis may be unilateral or bilateral and is most commonly seen at the L5 level (85% to 95% of the time), followed in frequency at L4. Spondylolysis is possible, but is much less common, at higher lumbar vertebral levels.
Sports such as gymnastics, dance, diving, volleyball, rowing, and football (linemen) have traditionally been thought to present high risk for spondylolysis. However, a recent study of nonelite athletes found that baseball, soccer, and basketball had the highest prevalence in males whereas gymnastics, marching band, and softball had the highest prevalence in females.2 Another recent study in New York found that soccer, basketball, lacrosse, baseball, tennis, and football were sports most associated with spondylolysis.4 It is important to consider the sports common to the surrounding geographic area.2 In general, adolescent athletes with back pain have a higher prevalence of spondylolysis compared with nonathletes.5
The adolescent growth spurt is a common factor in development of this injury as increased growth velocity places additional force on the spine during extension activities. Spinal deformities such as kyphosis and spina bifida occulta are also associated with spondylolysis. Tight hamstrings as well as gluteal and lumbar extensor weakness may increase risk of this condition.
Spondylolisthesis is a potential complication of a spondylolysis (Figure 3). This occurs when there is a bilateral spondylolysis with an anterior translation (slip) of 1 vertebra. Spondylolistheses are graded based on the amount of slippage of the width of the vertebral body. A grade 1 spondylolisthesis is the most common and least severe, with the amount of slippage less than 25% of the width of the vertebral body. Grade 2 is 25% to 50%; grade 3 is 50% to 75%; and grade 4 is slippage greater than 75% of the vertebral body width.
Patients with spondylolysis may complain of midline or lateral back pain that typically worsens with extension. It is unusual to have complaints of numbness, tingling, or limping, but these may occur if a spondylolisthesis is present and progresses to impact the spinal cord.
Diagnostic evaluation
The primary care physician should evaluate for the presence of any “red flags” that might raise concerns for malignancy or other worrisome etiology prompting further workup. Red flags would include symptoms starting at younger than age 4 years; nighttime pain; incontinence of bowel or bladder; fever; weight loss; history of malignancy; or severe and worsening pain.
As long as none of these factors are present, appropriate initial workup consists of AP and lateral radiographs (Figure 4).6 The radiographs may or may not show the presence of a spondylolysis. However, the lateral view evaluates for the presence of spondylolisthesis, which would indicate that there is a bilateral spondylolysis. Previously, oblique view radiographs of the lumbar spine were recommended to look for the “Scottie dog” sign. However, these views are not usually helpful as they may be normal even in the presence of spondylolysis. Given the additional radiation exposure without added value,7 these oblique views are no longer typically obtained.
If radiographs are completely normal, and there is high clinical suspicion for spondylolysis, it is prudent to consider initiating treatment that includes prolonged rest and physical therapy. Many athletes are anxious to return to sport, and finding a definitive diagnosis with advanced imaging can be helpful. There is variation of practice in the choice of advanced diagnostic imaging. Options include MRI, computed tomography (CT), bone scintigraphy, and single-photon emission computed tomography.
Computed tomography is the best way to visualize bone and it has been considered a gold standard for diagnosing spondylolysis. However, MRI is becoming more popular due to the lack of associated radiation.8 Dhouib and colleagues found that an MRI has 81% sensitivity and 99% specificity.9 Although typical MRI protocols usually are geared toward evaluation for disk pathology, which is more common in the adult population, a protocol that includes thin-cut oblique sequences may be helpful for visualizing the pars interarticularis to help assess for the presence of spondylolysis at this location (Figure 5). It may be useful to discuss the most appropriate test for the patient with a local radiologist.
Treatment protocols
Treatment of spondylolysis is typically very successful with conservative management. The cornerstones of initial treatment are rest, activity modification, physical therapy, and gradual progression back to activity when the athlete is pain free. Physical therapy can address lower extremity inflexibility and core weakness. One approach may be to wait until the athlete’s pain is decreased to initiate physical therapy. However, a recent study demonstrated that early initiation of physical therapy may decrease time to return to sport by an average of 25 days.10
Some providers may place athletes in a brace to immobilize the spine to help promote bony healing, but there is concern for further weakening of abdominal and core muscles with prolonged immobilization. The use of bracing in treatment of spondylolysis is debated. However, braces may be used to help reduce pain, allow for bony healing, and make the patient more comfortable with activities such as prolonged sitting in school. Bony healing is not necessary for resolution of symptoms as many athletes may have fibrous healing and still will be successfully able to return to sport pain free.11 Return to sport is typically achieved within 3 to 6 months, after the athlete has gradually added back extension-based activities and is able to participate in his/her sport without back pain.
Complications include development of spondylolisthesis if a patient has a bilateral spondylolysis. There is a small risk of progression that is highest around the adolescent growth spurt, which typically will occur prior to skeletal maturity. Referral to a spine surgeon should be made for spondylolistheses greater than grade 2, for significant change in degree of spondylolisthesis, or persistent symptoms for longer than 6 months despite conservative treatment and compliance (Figure 6). Development of neurologic symptoms such as progressive radiculopathy and cauda equina syndrome warrant urgent referral to a spine surgeon.
Prognosis for the patient
When teenaged athletes complain of lumbar back pain that worsens with activity, there should be a high index of suspicion for a spondylolysis. Careful consideration should take into account appropriate further workup with diagnostic imaging and course of treatment, the cornerstones of which are rest, physical therapy, and gradual return to activity.
Most patients do very well with conservative management, particularly in the short term. Of a small group of elite male ice hockey players, 96% were able to return to elite-level play with an average return to play at 8 weeks.12 In another study in which a retrospective review with telephone follow-up found that most patients (67%) are able to return to their previous level or higher of sport, however, 45% of patients reported recurrence of symptoms at long-term follow-up and 34% required medical treatment.10
There is no evidence that sports participation increases the chance of progression of spondylolisthesis.
References:
1. Kraft DE. Lumbar and thoracic spine. In: American Academy of Pediatrics Council on Sports Medicine, American Academy of Orthopedic Surgeons; Harris SS, Anderson SJ eds. Care of the Young Athelete. 2nd ed. Elk Grove Village, IL: American Academy of Pediatrics. 2009:331-342.
2. Selhorst M, Fischer A, MacDonald J. Prevalence of spondylolysis in symptomatic adolescent athletes: an assessment of sport risk in nonelite athletes. Clin J Sport Med. November 14, 2017. Epub ahead of print.
3. Nitta A, Sakai T, Goda Y, et al. Prevalence of symptomatic lumbar spondylolysis in pediatric patients. Orthopedics. 2016;39(3):e434-e437.
4. Ladenhauf HN, Fabricant PD, Grossman E, Widmann RF, Green DW. Athletic participation in children with symptomatic spondylolysis in the New York area. Med Sci Sports Exerc. 2013;45(10):1971-1974.
5. Schroeder GD, LaBella CR, Mendoza M, et al. The role of intense athletic activity on structural lumbar abnormalities in adolescent patients with symptomatic lower back pain. Eur Spine J. 2016;25(9):2842-2848.
6. Tofte JN, CarlLee TL, Holte AJ, Sitton SE, Weinstein SL. Imaging pediatric spondylolysis: a systemic review. Spine (Phila PA 1976). 2017;42(10):777-782.
7. Beck NA, Miller R, Baldwin K, et al. Do oblique views add value in the diagnosis of spondylolysis in adolescents? J Bone Joint Surg Am. 2013;95(10):e65.
8. Ledonio CG, Burton DC, Crawford CH 3rd, et al. Current evidence regarding diagnostic imaging methods for pediatric lumbar spondylolysis: a report from the Scoliosis Research Society Evidence-Based Medicine Committee. Spine Derform. 2017;5(2):97-101.
9. Dhouib A, Tabard-Fougere A, Hanquinet S, Dayer R. Diagnostic accuracy of MR imaging for direct visualization of lumbar pars defect in children and young adults: a systemic review and meta-analysis. Eur Spine J. September 23, 2017. Epub ahead of print.
10. Selhorst M, Fischer A, Graft K, et al. Long-term clinical outcomes and factors that predict poor prognosis in athletes after a diagnosis of acute spondolysis: a retrospective review with telephone follow-up. J Orthop Sports Phys Ther. 2016;46(12):1029-1036.
11. Klein G, Mehlman CT, McCarty M. Nonopertive treatment of spondolylosis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop. 2009;29(2):146-156.
12. Donaldson LD. Spondylolysis in elite junior-level ice hockey players. Sports Health. 2014;6(4):356-359.

Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.
Meet the Board: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI
May 20th 2022Contemporary Pediatrics sat down with one of our newest editorial advisory board members: Vivian P. Hernandez-Trujillo, MD, FAAP, FAAAAI, FACAAI to discuss what led to her career in medicine and what she thinks the future holds for pediatrics.