Update on Sexually Transmitted Diseases: Gonorrhea and Chlamydial Infections
Gonorrhea (aka "the clap," or "the drip") is caused by sexually transmitted Neisseria gonorrhoeae--a Gram-negative diplococcus. One of the most common reportable diseases in the United States, gonorrhea frequently affects sexually active adolescents. Approximately 30% of the 350,000 annual cases involve 15- to 19-year-olds. (That percentage is thought to be an underestimate!) Those most often infected are young women 15 to 24 years old. Recent data suggest that infection rates are higher among teens who are homeless or pregnant, and in those from a minority group or an economically disadvantaged background.
Gonorrhea (aka "the clap," or "the drip") is caused by sexually transmitted Neisseria gonorrhoeae--a Gram-negative diplococcus. One of the most common reportable diseases in the United States, gonorrhea frequently affects sexually active adolescents. Approximately 30% of the 350,000 annual cases involve 15- to 19-year-olds. (That percentage is thought to be an underestimate!) Those most often infected are young women 15 to 24 years old. Recent data suggest that infection rates are higher among teens who are homeless or pregnant, and in those from a minority group or an economically disadvantaged background.1
Updates on Sexually Transmitted Diseases:
•Herpes Simplex Virus Type 2 Infections
with Patient Education Guide
•Human Papillomavirus Infection
Sexually Transmitted Diseases: A Photo Quiz
Chlamydia trachomatis is the most common cause of sexually transmitted disease (STD) worldwide. The obligate intracellular bacterium has a predilection for columnar epithelium (found in the cervix) and the cells of the urethra. Like gonorrhea, rates of chlamydialinfection are highest in females aged 15 to 24. Infection is associated with new sexual partners, pregnancy, homelessness, and being from an economically disadvantaged minority group.
Here I review the magnitude of the problem and the consequences of undiagnosed infection. I also discuss new diagnostic tests and current treatment regimens.
GENITOURINARY TRACT INFECTIONS

Figure 1 – Symptomatic gonococcal urethritis typically presents with penile discharge and dysuria within 2 weeks of exposure. (Courtesy of the Public Health Agency of Canada)
When most physicians consider gonorrhea or chlamydial infection, painful, purulent urethritis or cervicitis comes to mind. Many clinicians believe that if their patient has no pain, dysuria, or genital discharge, then a pelvic examination or a male urethral swab is unnecessary. This misconception has contributed to the current epidemic of gonorrhea and chlamydial infection.
Both gonorrhea and chlamydial infection are usually asymptomatic; they are often discovered during routine screening, or when a partner becomes symptomatic. In one screening series, up to 84% of adolescent boys infected with N gonorrhoeae had no symptoms.2 Other school-based screenings for C trachomatis revealed that chlamydial infection was diagnosed in 2% to 4% of boys and in 8% to 16% of girls who were asymptomatic.3,4
Why are these infections so common among teenagers? The reasons are varied. From a biologic perspective, the adolescent girl's cervix has an increased amount of ectropion (columnar epithelium that extrudes over the exocervix and into the vaginal vault) that makes her more susceptible to these infections. In addition, adolescents tend to use condoms incorrectly and inconsistently. Serial monogamy--involving multiple sexual partners--is also associated with increased risk of STD exposure. Finally, some populations have higher rates of STDs, sexual abuse, and prostitution; these factors--combined with inadequate access to medical care--increase the risk of acquiring an infection during adolescence.
Because rates of asymptomatic gonorrhea and chlamydial infection are so high, most adolescent medicine providers recommend an annual pelvic examination with screening cultures in sexually active girls. Sexually active boys should provide a yearly first-morning void urine sample to screen for leukocyte esterase. If results are positive, more specific testing via urethral swab or urine DNA tests is indicated.
GONORRHEA

Figure 2 – Gonococcal urethritis is among the most common causes of Bartholin gland abcesses, which cause pain and labial swelling. (Courtesy of the CDC/Susan Lindsley)
In boys, symptomatic gonococcal urethritis typically occurs from 1 to 14 days after exposure. Patients may complain of dysuria and penile discharge initially (
Figure 1
). In approximately one third of patients, untreated infection progresses to involve the epididymis and surrounding structures along the genitourinary tract. Typically, patients with epididymitis present with unilateral scrotal pain, warmth, and swelling, with particular discomfort around the spermatic cord and epididymis. Prostatitis is an uncommon complication of gonococcal urethritis. Nevertheless, the diagnosis should be considered when lower back pain, urinary retention or frequency, and chills or fever accompany urethritis.
In girls, N gonorrhoeae infection can cause symptoms at any point between the outer and inner genitourinary tract. Itis one of the most common causes of Bartholin gland abscesses, which typically present as pain and swelling of the labia minora (Figure 2). If the patient complains of dysuria and/or urinary frequency, suspect gonococcal urethritis. Consider gonococcal cervicitis (Figure 3) in a girl with purulent vaginal discharge or with pelvic discomfort secondary to cervical edema.
Endocervical infections can progress to pelvic inflammatory disease (PID) when organisms spread through the cervical os into the uterus and/or fallopian tubes. It is not uncommon for PID to spread into the peritoneum and cause ovarian abscesses or even inflammation of the hepatic visceral capsule (Fitz-Hugh and Curtis syndrome).
CHLAMYDIAL INFECTION
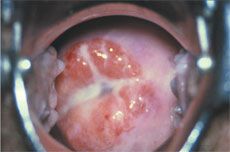
Figure 3 – Purulent vaginal discharge or pelvic discomfort secondary to cervical edema suggests gonococcal cervicitis. (Courtesy of the Public Health Agency of Canada)
Chlamydial urethritis is usually asymptomatic in boys, but it can produce a watery penile discharge 1 to 3 weeks after sexual exposure. Like gonorrhea, this infection can progress to epididymitis in young men. It rarely causes prostatitis;however, this diagnosis should be considered when prostate symptoms (described earlier) accompany known chlamydial urethritis
Chlamydial cervicitis can present with purulent discharge and vaginal blood spotting but is usually asymptomatic. Almost half of all cases of PID are caused by chlamydial infection. As with gonorrhea, this infection can spread to the ovaries and hepatic visceral capsule.
MINOR PATHOGENS IN GENITOURINARY INFECTIONS
When evaluating patients with infection-based genitourinary complaints, be sure to consider other causes of nongonococcal urethritis (NGU) or cervicitis. Most commonly, Ureaplasma urealyticum and Mycoplasma genitalium can cause NGU and may be implicated in PID. Ureaplasma is thought to act as a co-infectious agent with other patho- gens and probably does not cause PID on its own. Conversely, infection with M genitalium is more frequently diagnosed as a true sexually transmitted disease and may be an independent cause of both lower and upper genital tract infections.
EXTRA-GENITOURINARY INFECTIONS
In sexually active adolescents, gonorrhea and chlamydial infection can be present outside the genitourinary tract--depending on the type of sexual activity involved. Many adolescents consider oral sex to be "safe sex," but, of course, this is far from the truth. Fellatio (more so than oral-vaginal sex) can lead to gonococcal pharyngitis within a week of exposure. This infection is commonly asymptomatic, but it can cause fever, sore throat, and/or cervical lymphadenopathy, and may predispose the patient to disseminated gonorrhea (described below). Consider gonococcal pharyngitis when cultures of a throat swab are negative for streptococci in a sexually active teenager who has no concomitant signs of a viral syndrome. (Note: C trachomatis does not cause pharyngeal infections.)
The teenager with rectal gonorrhea or chlamydial infectionmay complain of rectal discharge, pain or difficulty with defecation, constipation, or rectal bleeding. These infections are typically acquired through unprotected anal sexual contact and often occur in heterosexual females and gay males. Any patient with a rectal STD is at increased risk for infections with hepatitis B virus and HIV; counsel and test such patients for these infections.
DISSEMINATED INFECTIONS

Figure 4 – Among the myriad manifestations of disseminated gonococcol infection are necrotic pustules that primarily involve the distal extremities. (Courtesy of the CDC/Dr Wiesner)
Gonococcal infection can spread hematogenously. Manifestations run the gamut from a monoarticular septic arthritis to full-blown disseminated gonococcal infection (DGI). The knee is most commonly involved in gonorrheal septic arthritis, but almost any large joint can be affected. Synovial fluid cultures are positive in fewer than a quarter of infected patients.
The specter of fulminant DGI is raised by the symptom constellation that includes polyarthritis, dermatitis, and tenosynovitis. DGI commonly spreads from asymptomatic gonorrheal infections of the pharynx or genitourinary tract. Persons with complement deficiencies tend to be at increased risk for disseminated infection, as are pregnant and menstruating women. The associated arthritis typically affects the knees, wrists, and ankles. Tenosynovitis can target tendons in the hands and fingers, as well as any joint in the lower extremities. Skin findings include necrotic pustules that primarily involve the distal extremities (Figure 4).
Reiter syndrome does not represent true bacterial dissemination in the classic sense, but it is probably an immune-mediated disorder that is frequently related to chlamydial infection. In some series, the traditional triad of urethritis, arthritis, and conjunctivitis has been associated with chlamydial urethritis in up to 50% of patients. Almost all patients with Reiter syndrome test positive for the HLA-B27 histocompatability antigen. Most patients with Reiter syndrome have bilateral arthritis of the heels or sacroiliac area, which distinguishes it from DGI.
DIAGNOSING GONORRHEA AND CHLAMYDIAL INFECTION
Historically, the diagnosis of gonorrheal urethritis or cervicitis was confirmed with a culture of either the distal urethra (in males) or the cervix (in females). The culture, plated on Thayer-Martin agar, was considered the diagnostic gold standard.
Over the past 10 years, a number of urine-based nucleic acid amplification tests (NAATs) have been developed as an alternative. Their obvious advantage (for males especially) is that they can be run on a first-void urine sample, thereby obviating an uncomfortable intra-urethral sampling. Most NAATs still require a cervical specimen, although some of the newer tests are approved for diagnosis of gonorrhea from vaginal canal or urine specimens (thus potentially avoiding a speculum examination).
When you suspect gonorrheal infection of an extragenital site (such as the pharynx, rectum, blood, or joint space), a culture or NAAT is still needed for diagnostic confirmation.
Before NAATs, most chlamydial infections were diagnosed on clinical criteria alone. (Cultures for C trachomatis are notoriously unreliable, and it is extremely difficult to obtain pathogen confirmation.) NAATs provide a reasonably accurate diagnostic modality. Specimens can be obtained from urine samples (in both males and females) as well as directly from the genital site, as indicated by the test manufacturer.
Be aware, however, that some states have specific requirements for Chlamydia testing protocols when the results may be used as forensic evidence. Therefore, if your teenage patient is a victim of sexual assault, contact your local child protection agency to determine exactly which test should be used to diagnose chlamydial infection.
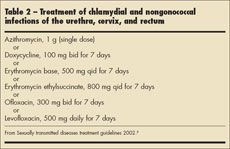
TREATMENT GUIDELINES
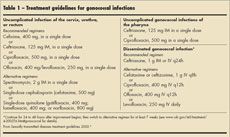
The 2002 CDC guidelines for the treatment of uncomplicated gonococcal and chlamydial infections can be accessed online at the CDC Web site (Tables 1 and 2).5 A few practical points deserve mention. Many pediatricians are uncomfortable prescribing fluoroquinolones for their patients. Most adolescent medicine providers would argue that these medications are probably safe and reasonable options in older teenagers--especially those who have already experienced most of their adolescent growth spurt.
There are, however, certain instances when fluoroquinolones should be avoided. If your male patient acquires urethritis or proctitis from sexual contact with another male, then these agents should be avoided because of the high rates of resistance to these medications in the "males-who-have-sex-with-males" population. Similarly, strains of gonorrhea acquired in the Pacific Islands, Southeast Asia, Hawaii, and California are often resistant to this drug class.
One final note: sexually transmitted infections tend to "travel together" from partner to partner. Therefore, when gonorrhea or chlamydialinfection has been diagnosed definitively (or when the patient has symptoms that suggest infection), treat for both infections--in case the culture or NAAT was not sufficiently sensitive. The patient should also be evaluated for other occult "traveling companions," such as HIV infection and syphilis.
References:
REFERENCES:
1.
Fortenberry JD, Neinstein LS. Overview of sexually transmitted diseases. In: Neinstein LS, ed.
Adolescent Health Care--A Practical Guide.
4th ed. Philadelphia: Lippincott Williams & Wilkins. 2002: 1085-1087.
2.
Pack RP, Diclemente RJ, Hook EW 3rd, Oh MK. High prevalence of asymptomatic STDs in incarcerated minority male youth: a case for screening.
Sex Transm Dis.
2000;27:175-177.
3.
Burstein GR, Waterfield G, Joffe A, et al. Screening for gonorrhea and chlamydia by DNA amplification in adolescents attending middle school health centers. Opportunity for early intervention.
Sex Transm Dis.
1998;25:395-402.
4.
Wiesenfeld HC, Lowry DL, Heine RP, et al. Self-collection of vaginal swabs for the detection of
Chlamydia,
gonorrhea, and trichomoniasis: opportunity to encourage sexually transmitted disease testing among adolescents.
Sex Transm Dis.
2001; 28:321-325.
5.
Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention. Available at:
www.cdc.gov/std/treatment/ default.htm.
Accessed February 10, 2006.
Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.